1 ...7 8 9 11 12 13 ...25 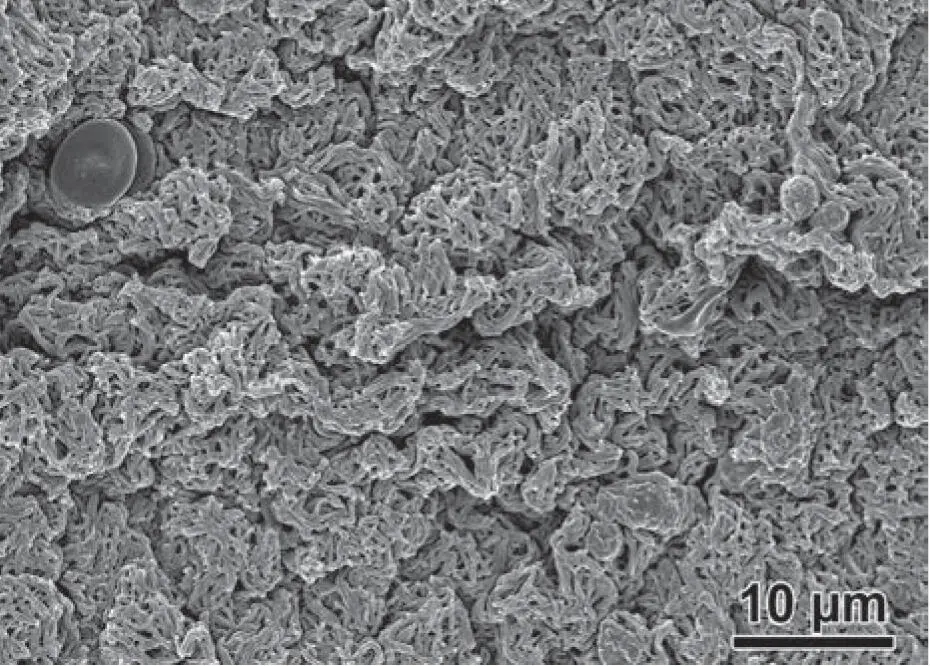
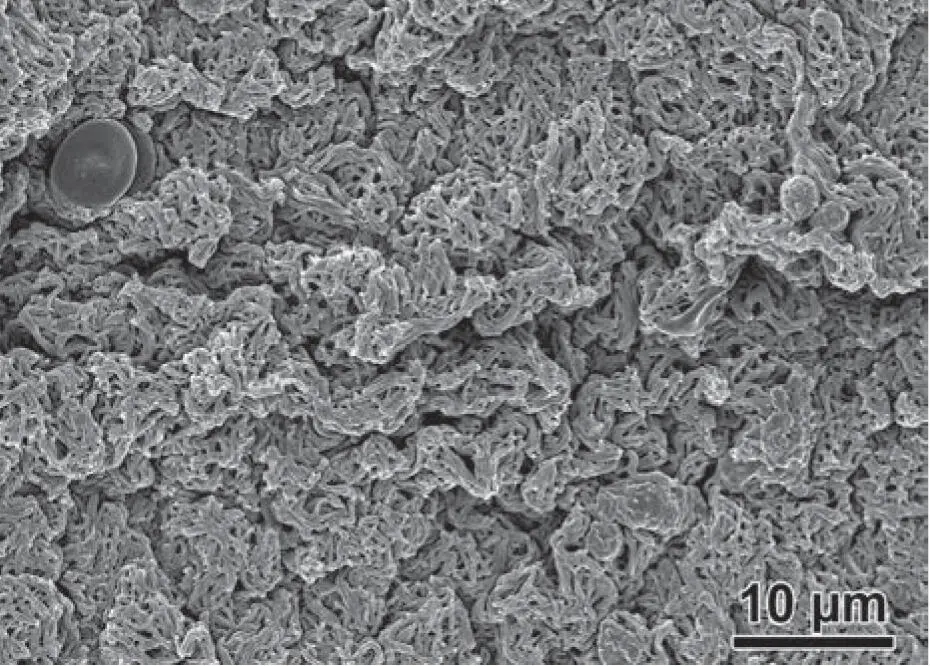
Fig 2-2SEM examination of the fibrin clot revealing a dense and mature fibrin matrix with various cell types entrapped within its matrix.
PRF forms a “superclot” consisting of an intimate assembly of cytokines, glycanic chains, and structural glycoproteins enmeshed within a slowly polymerized fibrin network.
The fibrin scaffold produced following centrifugation has further been identified as a biologic 3D network with the ability for the fibrillar micropores to support cell migration, proliferation, differentiation, and delivery of GFs. Platelets have theoretically been described as being massively trapped within the fibrin network, and the release of GFs is largely dictated by the actual timespan in which the 3D PRF scaffold is broken down (typically within 2–3 weeks). 18One of the major advantages of PRF when compared to PRP is the fact that by simply removing anticoagulants, a fibrin matrix is formed with a natural autologous delivery system capable of slowly and gradually releasing GFs over time. 7–9This leads to GF delivery over a period of 2 to 3 weeks as opposed to only a few hours observed in PRP. 12
Finally, stem cells exist naturally in whole blood, albeit at extremely low levels. 19,20Stem cells have the ability and potential to differentiate into many cell types, including adipocytes, osteoblasts, and chondrocytes. Many commercial enterprises report that mesenchymal stem cells (MSCs) exist in extremely high numbers in PRF or that only certain protocols or machinery favor their accumulation, but these reports have not been validated in any high-quality peer-reviewed journal. While future research investigating the impact of MSCs in blood is necessary, it may represent a potential future strategy to isolate MSCs relatively easily at low cost.
The commercial claims that MSCs exist in extremely high numbers in PRF or that only certain protocols or machinery favors their accumulation have not been validated.
Growth Factors in Blood
Naturally, GFs are critical to wound healing, and a variety of GFs have been commercialized as recombinant human sources once their roles were established. GFs are largely responsible for the migration of cells and also play a critical role in their adhesion, proliferation, and differentiation. While GFs exist in all tissues, it is important to note that blood serves as a main reservoir of numerous GFs and cytokines promoting angiogenesis and tissue regeneration for wound healing. It is also important to note that certain GFs may exist as inactive or partially active precursors that require proteolytic activation, or may further require binding to matrix molecules for activity or stabilization. For this reason, interfering with the natural clotting cascade such as when utilizing PRP may affect the bioactivity of certain GFs. 12Typically, GFs also have extremely short biologic half-lives in the order of a few minutes. 21The body has been trained to secrete various GFs in programmed orders to activate very complex cellular processes. 22Unlike recombinant human GFs that typically only comprise a single GF, platelet concentrates create the opportunity to deliver many autologous GFs simultaneously. Furthermore, leukocytes are known immune cells capable of “sensing” their microenvironment during the regenerative phase. Together with platelets, leukocytes serve as a major cell type during the natural wound healing process. The GFs most accumulated and delivered in PRF include VEGF, PDGF, TGF-β1, EGF, and IGF. 23,24Their individual roles are discussed below.
Unlike recombinant human GFs that typically only comprise a single GF, platelet concentrates create the opportunity to deliver many autologous GFs simultaneously.
VEGF
VEGF is secreted by activated thrombocytes and macrophages to damaged sites to promote angiogenesis. The VEGF family is related to PDGF and includes VEGF-A, -B, -C, -D, and -E. VEGF has previously been isolated and utilized as a recombinant GF described as the most potent GF for angiogenesis of tissues, stimulating new blood vessel formation, and facilitating nutrients and increased blood flow to sites of injury. 25,26It has potent effects on tissue remodeling, and the incorporation of recombinant human VEGF into various bone biomaterials alone has been demonstrated to increase new tissue regeneration. 27
PDGF
PDGFs are essential regulators that mainly promote the migration, proliferation, and survival of mesenchymal cell lineages. 28–33Platelets are of course the major source of PDGF, with various groups divided into homo- (PDGF-AA, PDGF-BB, PDGF-CC, and PDGF-DD) and heterodimeric (PDGF-AB) polypeptide dimers linked by disulfide bonds. They are mainly present in large quantities in platelet α-granules. Therefore, the ability to concentrate platelets in PRF leads to the massive accumulation and subsequent release of PDGF following centrifugation. It is important to note that because PDGF has an extremely short half-life (characterized by as little as 2 minutes), the ability for the PRF scaffold to act as a reservoir of GFs by protecting PDGF from matrix metalloproteinases actually drastically improves its release profile in living tissues when compared to PRP. Because it plays such a critical role in the mechanisms of physiologic healing, a recombinant source (rhPDGF-BB) was made commercially available with FDA clearance for the regeneration of various defects in medicine and dentistry.
Because PDGF has an extremely short half-life (characterized by as little as 2 minutes), the ability for the PRF scaffold to act as a reservoir of GFs by protecting PDGF from matrix metalloproteinases actually drastically improves its release profile in living tissues when compared to PRP.
TGF-β1
TGF-β is a large superfamily of more than 30 members that mediate tissue repair, immune modulation, and ECM synthesis. 34,35TGF-β1 is the predominant isoform that supports cell proliferation of practically all cell types. 21It further plays a role in angiogenesis, re-epithelialization, and connective tissue regeneration. 21Platelets are known to be a major source of TGF-β production. Specific to bone healing and remodeling, TGF-β also exerts effects by being heavily released from autogenous bone. 21
EGF
The EGF family is responsible for the chemotaxis and angiogenesis of endothelial cells and mitosis of mesenchymal cells. It further enhances epithelialization and markedly shortens the overall healing process time when administered as a recombinant source. EGF is typically secreted naturally by the body after acute injury and acts to significantly increase the tensile strength of wounds. EGF receptors exist on most human cell types, including those that play a critical role during wound repair such as fibroblasts, endothelial cells, and keratinocytes. 36
IGF
IGFs are positive regulators of proliferation and differentiation of most cell types. 37IGF is found in high levels in PRF because it is highly released from platelets during their activation and degranulation, leading to the differentiation of mesenchymal cells. IGF is also an extremely attractive GF because it constitutes the major axis of programmed cell apoptosis regulation by inducing survival signals protecting cells from many apoptotic stimuli. 37
Comparative Analysis of PRP Versus PRF
Years ago, much research investigated the comparative analysis in bioactivity and tissue regenerative properties of PRP and PRF. 12The aim was to determine if PRF was significantly better than previously utilized PRP with respect to the initial cell content, GF release, and clinical benefit. Naturally, the release profile of GFs has been an important and highly investigated research topic over the years and differs quite significantly between PRP and PRF. The typical advantage of PRF over PRP is that it enables the controlled release of GFs over an extended period of time because of its fibrin matrix. Therefore, when PRF is directly compared to PRP, a much longer GF delivery response has been observed 38( Fig 2-3). In a first study on this topic performed by our research team, GF release from three different platelet concentrates including PRP, L-PRF, and A-PRF demonstrated a much higher total amount of GFs released from PRF when compared to PRP over a 10-day period. In order to precisely quantify each GF in a comparative fashion, PDGF, VEGF, TGF-β1, EGF, and IGF were compared at numerous time points including 15 minutes, 60 minutes, 8 hours, 24 hours, 3 days, and 10 days (see Fig 2-3). Interestingly, at an early time point (15 minutes), significantly higher numbers of GFs were released from PRP when compared to L-PRF or A-PRF, whereas both PRF groups had higher release at later time points and also total release of GFs. From 3 days and onward, the GF release of PRF far exceeded that of PRP. 12
Читать дальше