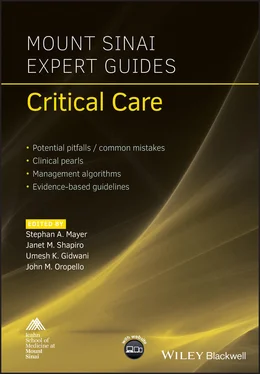
Mount Sinai Expert Guides
Здесь есть возможность читать онлайн «Mount Sinai Expert Guides» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Mount Sinai Expert Guides
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Mount Sinai Expert Guides: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Mount Sinai Expert Guides»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Mount Sinai Expert Guides — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Mount Sinai Expert Guides», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Table 7.1 Determining patients’ ideal body weight (IBW).*
| Males IBW = 48 kg for the first 5 feet of height + 2.7 kg for each inch taller |
| Females IBW = 45.5 kg for the first 5 feet of height + 2.2 kg for each inch taller |
| For patients with actual weight greater than 1.2 times IBW the adjusted body weight (ABW) is used ABW= ([actual weight – IBW] × 0.25) + IBW |
| For patients with actual weight less than 0.9 times IBW the actual body weight is utilized |
*G. J. Hamwi Formula (1964).
Table 7.2 Determining protein requirements (g/day).
| Physiologic stress, post‐surgery, or wound healing =1.2–2.0 g/kg/day × [weight in kg *] |
| Critical illness = 1.5 g/kg/day × [weight in kg] |
| Renal failure, not on renal replacement therapy = 0.8–1.2 g/kg/day × [weight in kg] |
| Hemodialysis = 1.2–1.4 g/kg/day × [weight in kg] |
| Continuous veno‐venous hemofiltration ≥1.5 g/kg/day × [weight in kg] |
*Weight determined from Table 7.1.
Table 7.3 Determining caloric and macronutrient requirements (g/day): carbohydrates.
| Total caloric requirement = [weight in kg] × 25 kcal/kg/day |
| ½ × Total caloric requirements = carbohydrates calories ½ × Total caloric requirements = protein + lipid calories |
| Carbohydrates in grams = carbohydrate calories/calories per gram carbohydrate *= ½ × total caloric requirements/calories per gram carbohydrate = 0.5 × [weight in kg] × 25 kcal/3.4 kcal/g = [weight in kg] × 3.67 g/kg/day |
*Carbohydrates = 3.4 kcal/g; lipids = 10 kcal/g; protein = 4 kcal/g.
Table 7.4 Determining caloric and macronutrient requirements (g/day): lipids and proteins.
| Lipid calories + protein calories = ½ × total caloric requirements |
| Protein calories = protein required (from Table 7.2) × calories per gram protein *= 1.5 g/kg/day × [weight in kg] (For critical illness) × 4 kcal/g |
| Lipids in grams = lipid calories/calories per gram lipid *= [(½ × total caloric requirements) – protein calories]/calories per gram lipid = [(½ × total caloric requirements) – protein calories]/10 kcal/g |
*Carbohydrates = 3.4 kcal/g; lipids = 10 kcal/g; protein = 4 kcal/g.
Micronutrients and other additives
Electrolytes are added to the TPN solution to maintain osmotic and electrolyte homeostasis. Sodium, potassium, magnesium, and calcium are added as either chloride, acetate, or phosphate salts.
Standard additions include thiamine, folate, multivitamin, and trace elements that include selenium, chromium, copper, and manganese.
Glycemic control is achieved by adding and titrating the amount of regular insulin in the TPN solution.
Certain other medications can be added to the TPN solutions depending on their solubility and stability. These include H2‐blockers and heparin.
A minimum of 150 mL of free water is required for dissolution of the additives in the TPN solution. This can be increased if the patient has additional free water deficits.
Administration
Parenteral nutrition needs to be infused via a secure central venous access. This avoids complications of phlebitis and injury from extravasation. To minimize infections we recommend maintaining one port dedicated to TPN infusion.
The total volume of TPN solution is infused at a fixed rate over a 24 hour period. In patients with severe cholestasis or hepatic dysfunction, TPN can be cycled over 12 hours instead.
While initiating TPN it is important to begin with a half strength solution to minimize complications such as electrolyte derangements, hyperglycemia, and refeeding syndrome. The solution can be advanced over 1–3 days if monitoring panels remain stable.
While weaning patients off TPN, the caloric strength of the solution should be reduced slowly by 50% before discontinuing the TPN completely.
Adaptation to special situations
Severe respiratory failure:In patients with respiratory failure or significant ventilator dependence, care should be taken to avoid overfeeding patients. Overfeeding shifts the body into lipid synthesis with concomitant elevation in arterial CO2 levels potentially lengthening ventilator support duration.For the production of the same amount of energy, the oxidation of lipid generates 25% less CO2 than carbohydrates. In patients with hypercapneic respiratory failure, a greater proportion of the caloric requirement should be met by lipids.
Renal failure:Renal failure leads to metabolic acidosis secondary to accumulation of numerous organic acids and increased loss of bicarbonate. TPN orders should be modified to provide additional bicarbonate (as acetate) and to avoid iatrogenic hyperchloremic acidosis.Continuous renal replacement therapies can result in up to 65 g/day loss of protein through the dialysate/ultrafiltrate process. Consequently, it is important to replenish the protein stores at a higher rate (≥1.5 g/kg/day).Volume overload is a common complication of renal failure and has adverse impacts on other organ systems including the heart and the lung. Minimizing the total volume of the TPN solution by concentrating the elements can be helpful in preventing this from arising.Electrolytes need to be carefully monitored in patients to avoid the risk of life‐threatening hyperkalemia and other electrolyte imbalances.
Liver failure:Patients have poor intrinsic synthetic function and may require greater protein replacement.Repletion of micronutrient reserves including water‐soluble vitamins requires special consideration.The use of branched chain amino acids in patients with hepatic encephalopathy has yielded mixed results and cannot be recommended as standard practice.If total bilirubin is >4, remove copper and manganese by omitting trace elements to avoid toxicities (these elements are dependent on bile for excretion).
Monitoring
Daily bedside clinical examination is important to assess vascular access site appearance, volume status, neurologic function, weight monitoring, and readiness for initiation of enteral nutrition.
Labs include daily monitoring of electrolytes, glucose, liver, and lipid panels.
For patients on prolonged TPN support, less frequently monitored parameters include TSH, PTH, vitamin D, transthyretin, and carnitine levels.
24 hour nitrogen balance has been a validated marker for improved outcomes. It is calculated by subtracting the total nitrogen removed (via urine and stool) from the total nitrogen consumed. Every gram of negative nitrogen balance reflects a loss of 6.25 g of protein or 30 g of muscle mass.
Indirect calorimetry allows for measurement of resting energy requirements and respiratory quotients (RQs) using measurements of oxygen consumed and carbon dioxide produced. While it requires considerable investment in specialized equipment and training, indirect calorimetry can also provide information on whether there is ongoing over‐ or underfeeding.
A RQ of <0.8 signifies a considerable catabolic state where fats and proteins are being utilized as the source of energy. Conversely, in patients with a RQ >1.0 this signifies overfeeding. The goal RQ for patients on TPN is between 0.8 and 1.0.
Complications
Catheter infections remain the major infectious complication of parenteral nutrition. Common pathogens include Staphylococcus epidermidis, Candida, and S. aureus. For patients on TPN, an established catheter monitoring and maintenance protocol is essential. In patients with suspected infection, replacement of the central catheter at a different site is necessary.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Mount Sinai Expert Guides»
Представляем Вашему вниманию похожие книги на «Mount Sinai Expert Guides» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Mount Sinai Expert Guides» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.