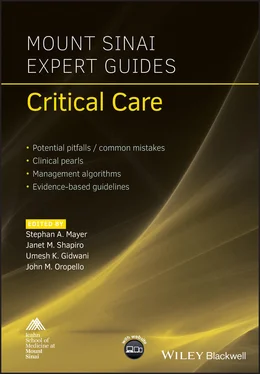
Mount Sinai Expert Guides
Здесь есть возможность читать онлайн «Mount Sinai Expert Guides» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Mount Sinai Expert Guides
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Mount Sinai Expert Guides: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Mount Sinai Expert Guides»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Mount Sinai Expert Guides — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Mount Sinai Expert Guides», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Clinical diagnosis
History
Symptoms depend on both glucose level and duration of hyperglycemia:
Cardiovascular: myocardial injury, electrolyte imbalances causing arrhythmia.
Constitutional: lethargy.
Gastrointestinal: nausea, vomiting.
Neurologic: mental status changes, encephalopathy, seizures, chorea, and other involuntary movements.
Renal: polyuria, acute kidney injury.
Physical examination
Depending on the cause of hyperglycemia, some physical exam findings may be present. In stress‐induced hyperglycemia, however, arguably the commonest cause in the critically ill patient, the physical exam may not be very revealing.
Physical exam findings may include acanthosis nigricans in diabetes mellitus and Cushingoid features in Cushing’s disease.
Laboratory diagnosis
Blood gas analyzers are considered accurate, making them the ideal test in the critical care unit. Blood gas analysis requires arterial blood draws, and monitoring via an arterial line would be preferred to provide adequate glucose control. Despite being invasive, it is the consensus recommendation for glucose monitoring of severely ill patients.
Non‐invasive point‐of‐care (POC) glucose testing devices utilizing fingerstick or tiny amounts of blood obtained via an indwelling vascular line are the most widely used tests for hyperglycemia. These provide rapid results in critically ill patients where glucose fluctuations are unpredictable. POC testing, however, is inaccurate, sometimes differing by as much as 20% from reference values.
Continuous glucose monitoring systems of the glucose in the interstitial space every 10 seconds is a promising test providing an average glucose value every 5 minutes.
The glucose trend may be more useful than the absolute glucose value when using less accurate blood glucose monitors such as POC and continuous interstitial glucose monitors.
Stress‐related hyperglycemia in the ICU is acute and therefore would not usually cause an elevation in hemoglobin A1c, making this a method to potentially differentiate between stress‐induced hyperglycemia and long‐standing diabetes.
Potential pitfalls/common errors made regarding diagnosis of disease
The diagnosis of diabetes mellitus in the ICU is commonly missed given the incidence of hyperglycemia due to secondary causes. One study showed that 26% of diabetic patients were undiagnosed during their admission to the ICU. These patients had a higher likelihood of requiring an insulin infusion, higher average blood glucose, an increased percentage of hyperglycemia and hypoglycemia (i.e. higher glycemic variability), and increased mortality. These findings suggest that a high suspicion of diabetes in order to anticipate insulin requirement might be beneficial.
Due to glycemic variability in the critically ill patient, routine monitoring, sometimes continuous, is recommended. A patient who is normoglycemic on admission may not remain so throughout their ICU stay and may even require an insulin infusion at some point depending on the degree of hyperglycemia. Therefore routine glucose measurements are recommended during critical illness with strict guidelines on initiation of insulin therapy.
Treatment
Much controversy surrounds the idea of what constitutes ideal blood glucose targets in the critically ill patient. Multiple trials have yielded contradictory results. Initially, stringent glucose level control was advocated; however this recommendation was challenged because of the recognition that hyperglycemia was the body's way of adapting to stress. In the early 2000s, the Leuven surgical trial concluded that intensive glucose control decreased mortality. Despite the faults of this trial, it created a movement for strict glucose goals of around 120 mg/dL.
However, the subsequent NICE‐SUGAR trial, targeting a glucose level less than 180 mg/dL, showed decreased mortality and less hypoglycemia compared with intensive glucose control. Despite the contradicting evidence, the consensus at this time is to target a glucose level of 140–180 mg/dL.
There is no universally accepted insulin regimen for glycemic control in critically ill patients. However, to avoid prolonged hypoglycemia, which may be harmful, insulin infusions and intermittent short‐acting insulin are typically used until the patient is stable enough to be transitioned to subcutaneous insulin.
No oral agents are used in the ICU for glucose control given the unpredictability of the metabolism in critically ill patients.
Depending on the glucose level, insulin can be given intravenously or subcutaneously. If there is a reading above 220 mg/dL or two consecutive readings above 180 mg/dL, the intravenous route is preferred. If the glucose reading is between 160 and 179 mg/dL, subcutaneous insulin is given. The options in subcutaneous insulin include short‐acting insulin, sliding scale insulin, NPH insulin, and long‐acting insulin.
Preferred route of insulin administration
| Glucose level (mg/dL) | Route |
| 160–179 | Subcutaneous |
| 180–219 | Subcutaneous |
| >220 | Intravenous |
| Two consecutive readings of >180 | Intravenous |
Monitoring of glucose level
When on intravenous insulin, glucose is checked every hour until it remains within goal for over 4 hours, after which it can be checked every 2 hours. If there is any change in clinical condition, insulin infusion rate, or nutritional support, switching back to hourly glucose checks is advised. When on subcutaneous insulin, glucose can be checked every 2–4 hours initially, then with meals and at bedtime once glucose is within target for over four readings.
Transitioning from intravenous to subcutaneous insulin
The last 24 hour insulin requirement is calculated by multiplying the requirement in the last 6 hours of insulin infusion, dividing by 6 and multiplying by 20; this will be the total insulin given in a day.
40% of the total daily units are given as long‐acting insulin and 60% are given as short‐acting insulin three times a day.
If giving NPH insulin, the total dose is divided by 4 and given every 6 hours.
If a patient is on less than 2 units of insulin per hour while on the drip, consider starting on short‐acting insulin.
Discontinue intravenous insulin 60 minutes after giving subcutaneous insulin.
Nutrition and insulin
For PO feeds, long‐acting insulin and short‐acting insulin are preferred.
For continuous feeds, consider NPH insulin.
If feeds are held, give basal insulin and hold rapid‐acting insulin.
If continuous feeds are held, hold NPH and long‐acting insulin and give short‐acting insulin or add D10 at previous rate of feeds.
Management of complications
The commonest complication of glucose control in the ICU is hypoglycemia which is defined as blood glucose less than 80 mg/dL. The association between mortality and glucose level is 'J‐shaped' meaning that there is increased mortality at both extremes making it important to avoid hypoglycemia.
Blood glucose 90–120: hold insulin infusion and repeat blood glucose in 1 hour.
Blood glucose 71–89: hold insulin infusion and repeat glucose in 30 minutes.
Blood glucose 51–70: give 12.5 g of 50% dextrose and repeat glucose in 15 minutes.
Blood glucose <50: give 25 g of 50% dextrose then confirm reading with arterial blood if possible and repeat glucose in 15 minutes.
Treatment/management
Интервал:
Закладка:
Похожие книги на «Mount Sinai Expert Guides»
Представляем Вашему вниманию похожие книги на «Mount Sinai Expert Guides» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Mount Sinai Expert Guides» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.