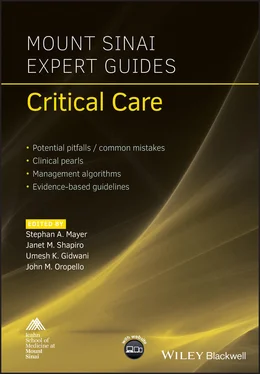
Mount Sinai Expert Guides
Здесь есть возможность читать онлайн «Mount Sinai Expert Guides» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Mount Sinai Expert Guides
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Mount Sinai Expert Guides: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Mount Sinai Expert Guides»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Mount Sinai Expert Guides — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Mount Sinai Expert Guides», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Hyperglycemia can occur as a result of increased parenteral carbohydrate availability along with concomitant insulin resistance. This can be avoided by gradual titration to the patient’s carbohydrate goal as well as regular glucose monitoring. Goal blood glucose should be between 140 and 180 mg/dL.
Hypertriglyceridemia can occur as a result of lipids infusion, the underlying stress hormone production, and renal insufficiency. In severe cases (triglycerides >1000 mg/dL) this can lead to precipitation of acute pancreatitis. Lipids should be removed from TPN if the plasma triglyceride concentration exceeds 400 mg/dL.
Hepatic steatosis and cholestasis are known complications of long‐term parenteral nutrition. More often seen in children, the exact etiology of fatty liver remains unclear. In the absence of enteral nutrition it is also common for development of cholestasis and biliary sludge. Early resumption of enteral feeding is the definitive treatment. Experimental use of ursodeoxycholic acid and cholecystokinin have shown mixed results.
Refeeding syndrome can occur when TPN is introduced to patients who are severely malnourished. A rapid intracellular shift of potassium phosphorous and magnesium can precipitate rhabdomyolysis heart failure and cardiac arrhythmias. Careful monitoring and timely replacement of electrolytes can help avoid this complication.
Intestinal mucosal atrophy can occur in the absence of enteral nutrition. There is risk for bacterial overgrowth and translocation of bacteria in the setting of mucosal denudation and impaired local immunity. The early initiation of trophic feeds helps reduce the risk of infection and translocation. The role of antibiotic agents such as neomycin to inhibit bacterial growth remains poorly defined.
Reading list
1 Hartl WH, Jauch KW, Parhofer K, Rittler P. Complications and monitoring – guidelines on parenteral nutrition, chapter 11. Ger Med Sci. 2009; 7:Doc17.
2 Neuman T, Kohli‐Seth R, Wilson S, Bassily‐Marcus A. Total parenteral nutrition in the ICU: the Mount Sinai Hospital experience. ICU Director 2010; 1(4):203–9.
3 Plauth M, et al. ESPEN Guidelines on Parenteral Nutrition: hepatology. Clin Nutr 2009; 28(4):436–44.
4 Singer P, Pichard C. Reconciling divergent results of the latest parenteral nutrition studies in the ICU. Curr Opin Clin Nutr Metab Care 2013; 16(2):187–93.
5 Thibault R, Pichard C. Parenteral nutrition. World Rev Nutr Diet 2013; 105:59–68.
Additional material for this chapter can be found online at:
www.wiley.com/go/mayer/mountsinai/criticalcare
This includes multiple choice questions. 
CHAPTER 8 Glycemic Control
Amira Mohamed1 and Adel Bassily‐Marcus2
1Albert Einstein College of Medicine, New York, NY, USA
2Icahn School of Medicine at Mount Sinai, New York, NY, USA
OVERALL BOTTOM LINE
Intravenous insulin is recommended in hyperglycemic patients in the ICU.
When on intravenous insulin infusion, glucose should be checked every hour until it is at goal for at least 4 hours.
Once stable, patients on PO diet should be started on long‐acting and meal time insulin; patients on continuous feeds should be started on NPH insulin every 6 hours.
When converting to long‐acting insulin, total insulin dose is calculated using the insulin requirement in the last 6 hours of insulin infusion.
Background
The last decades have witnessed great changes in the definition of glycemic control in the ICU. In the 1990s, stringent glucose control was encouraged. However, later studies have reported the complications of hypoglycemia.
After the NICE‐SUGAR trial demonstrated increased mortality with intensive control, current guidelines recommend a more lenient approach with a target blood glucose level of approximately 140–180 mg/dL. The prevalence of diabetes in the USA has greatly increased to an astonishing 23.9% of the population, 40% of whom are still undiagnosed. The prevalence of diabetes in hospitalized patients appears to be as high as 25%. However, because inpatient diabetes studies are not routinely performed this number is likely underestimated. It is estimated that about 3160 dollars per patient are saved in health care costs as a result of decreased ICU length of stay, sepsis, renal failure, and even mechanical ventilation.
The causes of hyperglycemia in the ICU are complex and not limited to diabetes but are also caused by the impact of stress hormones such as cortisol including both stress‐induced or iatrogenic increases in steroid levels. Differentiation between the causes of hyperglycemia is challenging which is why the exact incidence of each is not yet known.
Pathogenesis
There is a substantial amount of evidence to suggest that stress‐induced hyperglycemia or hospital‐related hyperglycemia is an independent risk factor for increased morbidity and mortality when compared with hyperglycemia in diabetic patients.
Multiple factors contribute to hyperglycemia in the critically ill non‐diabetic patient such as stress hormones and inflammatory mediators causing insulin resistance and an increase in the rate of gluconeogenesis. Nonetheless, the question that remains unanswered is whether the resultant hyperglycemia is a direct cause of mortality or simply an indicator of the severity of illness.
The effects of hyperglycemia in the critically ill patient include leukocyte dysfunction, increased oxidative stress, and hypercoagulability and have also been associated with myocardial injury and increase in stroke size.
Recent evidence has suggested that stress‐induced hyperglycemia and hyperglycemia secondary to diabetes do not have the same mortality risk. Stress‐induced hyperglycemia is associated with worse outcome, including increased risk of infection and increased length of stay compared with diabetic hyperglycemia.
Risk factors for hyperglycemia
Diabetes mellitus.
Medications including exogenous glucocorticoids, vasopressors, lithium, and beta‐blockers.
Inflammatory conditions including sepsis.
Overfeeding, intravenous dextrose, commonly used parenteral nutrition.
Dialysis solutions, antibiotic solutions.
Insufficient insulin.
Volume depletion can cause hyperglycemia.
Bed rest.
Prevention of hyperglycemia
In order to potentially reduce the adverse effects of hyperglycemia, it has to be recognized early with the necessary management implemented immediately. However, other than early detection and management, there is no evidence of any means of preventing hyperglycemia prior to its occurrence.
Diagnosis
Differential diagnosis of hyperglycemia in the ICU
| Differential diagnosis | Features |
| Diabetes mellitus | Elevated hemoglobin A1c, weight loss, polyuria, polydipsia |
| Hormonal disorders such as Cushing's disease or acromegaly | Elevated cortisol/growth hormone, weight gain, Cushingoid features |
| Drug such as steroids, sympathomimetic drugs | History of medication use |
Typical presentation
Critically ill patients with hyperglycemia present differently compared with otherwise healthy diabetic patients. In a critically ill patient, polyuria, polydipsia, and other common symptoms of hyperglycemia may not be present. Patients may present with acute kidney injury and decreased urine output. Due to the severity of illness, including delirium and mechanical ventilation, patients may not be able to communicate their symptoms. Moreover, given the acuity of glucose change, the physical exam may be equivocal and therefore routine blood tests are essential for diagnosis.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Mount Sinai Expert Guides»
Представляем Вашему вниманию похожие книги на «Mount Sinai Expert Guides» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Mount Sinai Expert Guides» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.