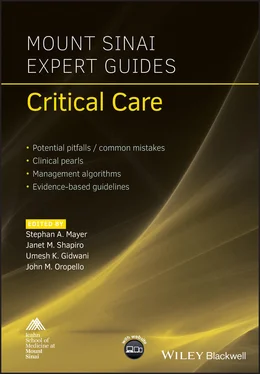
Mount Sinai Expert Guides
Здесь есть возможность читать онлайн «Mount Sinai Expert Guides» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Mount Sinai Expert Guides
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Mount Sinai Expert Guides: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Mount Sinai Expert Guides»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Mount Sinai Expert Guides — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Mount Sinai Expert Guides», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
OVERALL BOTTOM LINE
Critically ill patients have increased metabolic demands and are vulnerable to developing malnutrition.
Nutritional support should be started early to minimize morbidity and mortality.
Both under‐ and overfeeding have deleterious effects on the patient’s health.
Enteral nutrition is preferred over parenteral nutrition where possible.
Nutritional support requires a dedicated team and close monitoring to avoid infectious and metabolic complications.
Background
Patients in the ICU are faced with unique challenges predisposing them to a malnourished state. This includes systemic infections, pronounced blood loss, mechanical ventilator support, multiorgan failure, limitation to volitional intake, and prolonged bed rest.
Critically ill patients present with a hypermetabolic state, which is marked by increased energy requirements, simultaneous protein synthesis and breakdown, increased lipolysis, and increased insulin resistance.
There has been a direct link between poor nutritional status and worse hospital outcomes including wound healing, iatrogenic infections, prolonged ventilator dependence, renal insufficiency, and endocrine dysfunction.
These factors have to be kept in mind while assessing and supporting the patient’s nutritional needs. Enteral nutrition refers to the administration of nutrients through the gastrointestinal tract. Parenteral nutrition refers to the intravenous administration of nutrients.
Goals of nutrition in the critically ill
Caloric requirements during critical illness are increased. If these are unmet by the dietary intake it will lead to a catabolic state with breakdown of a patient’s protein and lipid reserves.
Overfeeding is as harmful as underfeeding as it leads to excess production of CO2, potentially exacerbating respiratory failure and fatty deposition in the liver and other organs.
A patient’s response to nutritional support is altered by the underlying stress of illness. Care needs to be taken to ensure that metabolic derangements such as hyperglycemia or hypertriglyceridemia are not precipitated or worsened.
Micronutrients including minerals, vitamins, and trace elements are essential components of nutritional therapy in critically ill patients. Their deficiency can present with systemic disorders.
Enteral nutrition
Nutrition provided via the gastrointestinal tract is the preferred route for nutritional support. Its benefits include a more physiologic preparation, less cost, and fewer associated metabolic complications.
Enteral nutrition allows for preservation of mucosal integrity and stimulation of protective gut functions including immunomodulatory and endocrine effects.
Enteral nutrition has associated potential risks of aspiration, malabsorption, gut ischemia, and variable tolerance to administered feeds.
In the absence of contraindications, enteral nutrition should be started within 48–72 hours of ICU admission. Early feeding is associated with lower gut permeability, smaller energy deficits, and concomitant reductions in morbidity and mortality.
For initiating enteral feeds a temporary enteral access is secured via a nasogastric feeding tube. In patients with anticipated prolonged inability to swallow, a percutaneous endoscopic gastrostomy (PEG) tube can be utilized.
In patients with gastric distension, poor motility, or concern for aspiration, post pyloric feeding tubes can be used instead of gastric feeding tubes.
Enteral nutrition formulation
Enteral formulas are premixed solutions with a fixed ratio of non‐protein calories to protein. They are designed to provide an energy density of 1–1.5 kcal/mL of solution. The total volume of feed over 24 hours is calculated by dividing the calories required (25 kcal/kg/day) by the energy density of the feeding.
The protein component in formulary feeds can be either whole protein (soy/casein), peptides, or elemental amino acids depending on the patient’s ability to digest and absorp protein.
The use of supplements such as arginine, glutamine, antioxidants, and omega‐3 polyunsaturated fatty acids has been studied with the aim of reducing inflammation and modulating immune response. While animal and in vitro studies have been promising, there is currently inadequate clinical evidence to recommend their widespread adoption.
Volume loss and hypernatremia can be corrected by supplying free water along with the enteral feeds.
Total parenteral nutrition
TPN formulations are designed to intravenously provide all necessary macronutrients and micronutrients through one solution. It enables consistent and predictable provision of nutritional intake to the patient.
Macronutrients include carbohydrates and lipids which serve as the primary source for calories. Protein in the TPN solution is designed to meet the body’s requirement for increased synthetic function as well as a source for energy.
Micronutrients include electrolytes (sodium, potassium, magnesium, calcium, chloride, selenium, chromium), buffers (phosphate, acetate), and other compounds (vitamins, insulin, famotidine).
The total volume of the formulation is adjusted in accordance with the patient’s volume status as well as to meet their daily fluid requirements.
TPN formulations need to be compounded daily to avoid degradation and microbial contamination.
Indications for TPN
Diseases of the gastrointestinal system that preclude all enteral feeding for prolonged periods of time:Trauma, bowel perforations, surgical resections, fistulae, and diversions.Inflammatory disorders including severe necrotizing pancreatitis, appendiceal abscess, and gangrenous cholecystitis.Immune disorders including bowel transplant rejection and graft versus host disease.Infections including severe Clostridium difficile infections, infected peritonitis, and intra‐abdominal abscesses.Malabsorptive disorders including short gut syndrome and inflammatory bowel disease.Neoplastic disorders including obstructive tumor growth, radiation‐ and chemotherapy‐induced mucositis, fistulae, and strictures.Vascular disorders including bleeding and ischemic bowel disease.
Disease conditions that preclude adequate intake of enteral nutrition:Profoundly cachectic patients with poor nutritional reserves.Inability to obtain or maintain enteral access.Enteral nutritional meeting <50% of nutritional requirements.Worsening signs of gastrointestinal tolerance.
Continuation of ongoing parenteral nutrition.
Energy and macronutrient dosing calculations
Daily energy requirements are calculated based on the patient’s ideal body weight (IBW) (Table. 7.1). Adjusted body weight is used if the patient’s weight exceeds IBW by 20%. If the patient’s weight is less than 90% of IBW then the actual weight is utilized.
The estimated daily energy consumption used to determine total energy requirements is 25 kcal/kg/day. In obese patients with a body mass index (BMI) >30, energy requirements are decreased to 22 kcal/kg/day.
The amount of protein is determined by factors including severity of illness, surgical trauma, and organ system failure ( Table 7.2). This allows the protein intake to be matched to the body’s synthetic requirements. At the same time, the calories contributed by the proteins are counted towards the total energy requirements, to minimize the risk of overfeeding.
Half the total caloric requirements are supplied by carbohydrate. The remaining half of caloric requirements is divided between lipids and proteins in a ratio determined by the patient’s protein requirement. The amount of each component is calculated using the energy equations ( Tables 7.3and 7.4).
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Mount Sinai Expert Guides»
Представляем Вашему вниманию похожие книги на «Mount Sinai Expert Guides» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Mount Sinai Expert Guides» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.