Bedside tracheostomy can be done in the ICU with the aid of bronchoscopic visualization.
Common complications
Pre‐procedure
From anesthetic: laryngospasm, bronchospasm.
From sedative: hypotension, bradycardia (propofol).
Laryngospasm or bronchospasm.
Hypoxemia.
Fever.
Hemoptysis.
Management of complications
| Complication |
Treatment |
| Hypotension |
Fluids, vasopressors |
| Laryngospasm |
Lidocaine (topical) |
| Bronchospasm |
Bronchodilators |
| Hypoxemia |
If patient is not on 100% O 2increase O 2If on 100% O 2, remove bronchoscope until saturation increases |
| Hemoptysis |
Usually minimal but for moderate hemoptysis use local epinephrine, tamponade, intubation of the non‐bleeding lung |
| Fever |
May occur for 24 hours post‐procedure; treatment is rarely needed but antipyretics can be given |
A CXR is generally not required after airway clearance, visualization, and lavage, but is often done to assess the efficacy of treatment for atelectasis.
1 Foster WM, Hurewitz AN. Aerosolized lidocaine reduces dose of topical anesthetic for bronchoscopy. Am Rev Respir Dis 1992; 146(2):520–2.
2 Gonlugur U, et al. Major anatomical variations of the tracheobronchial tree: bronchoscopic observation. Anat Sci Int 2005; 80:111–15.
3 Jin F, MU D, Chu D, et al. Severe complications of bronchoscopy. Respiration 2008; 76:429.
4 Jose R, Shaefi S, Navani N. Sedation for flexible bronchoscopy: current and emerging evidence. Eur Respir Rev 2013; 22(128):106–16.
5 Langmack EL, Martin RJ, Pak J, Kraft M. Serum lidocaine concentrations in asthmatics undergoing research bronchoscopy. Chest 2000; 117(4):1055–60.
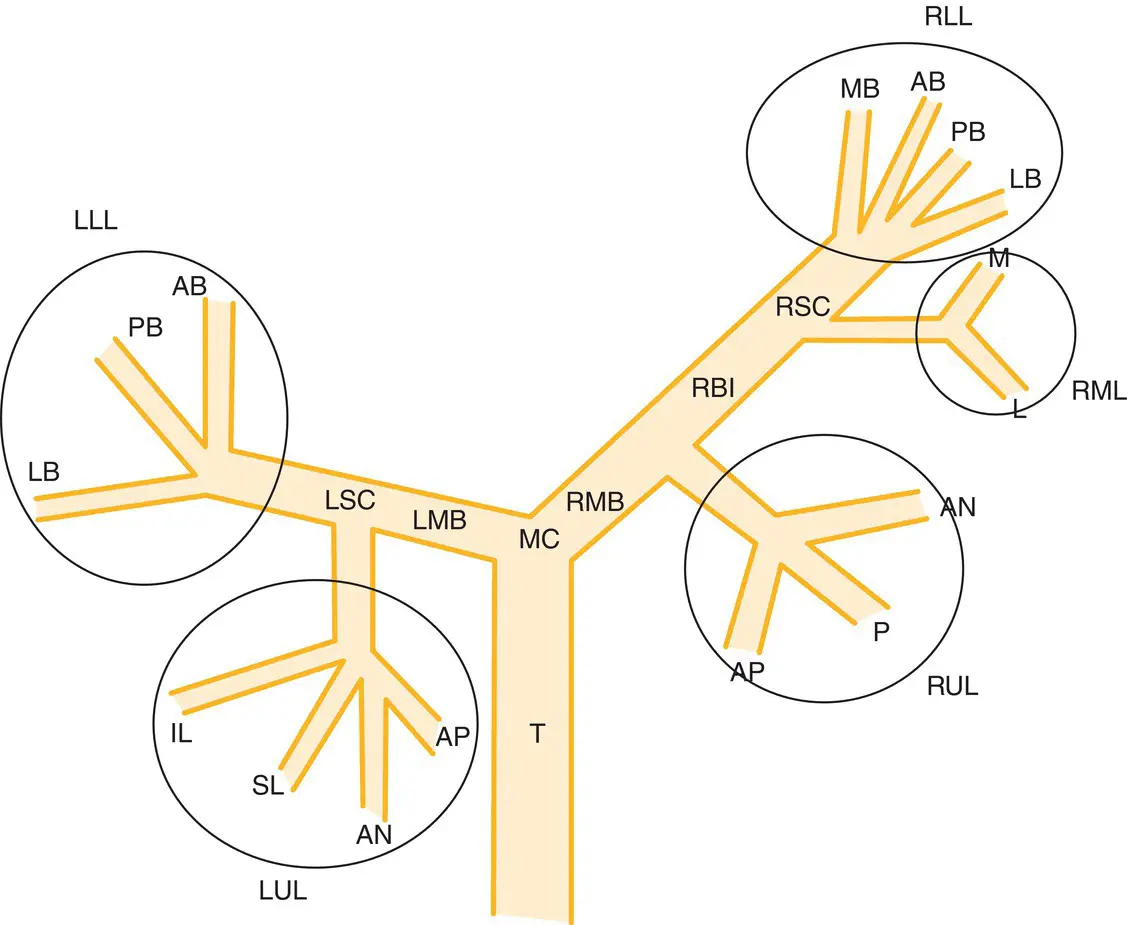
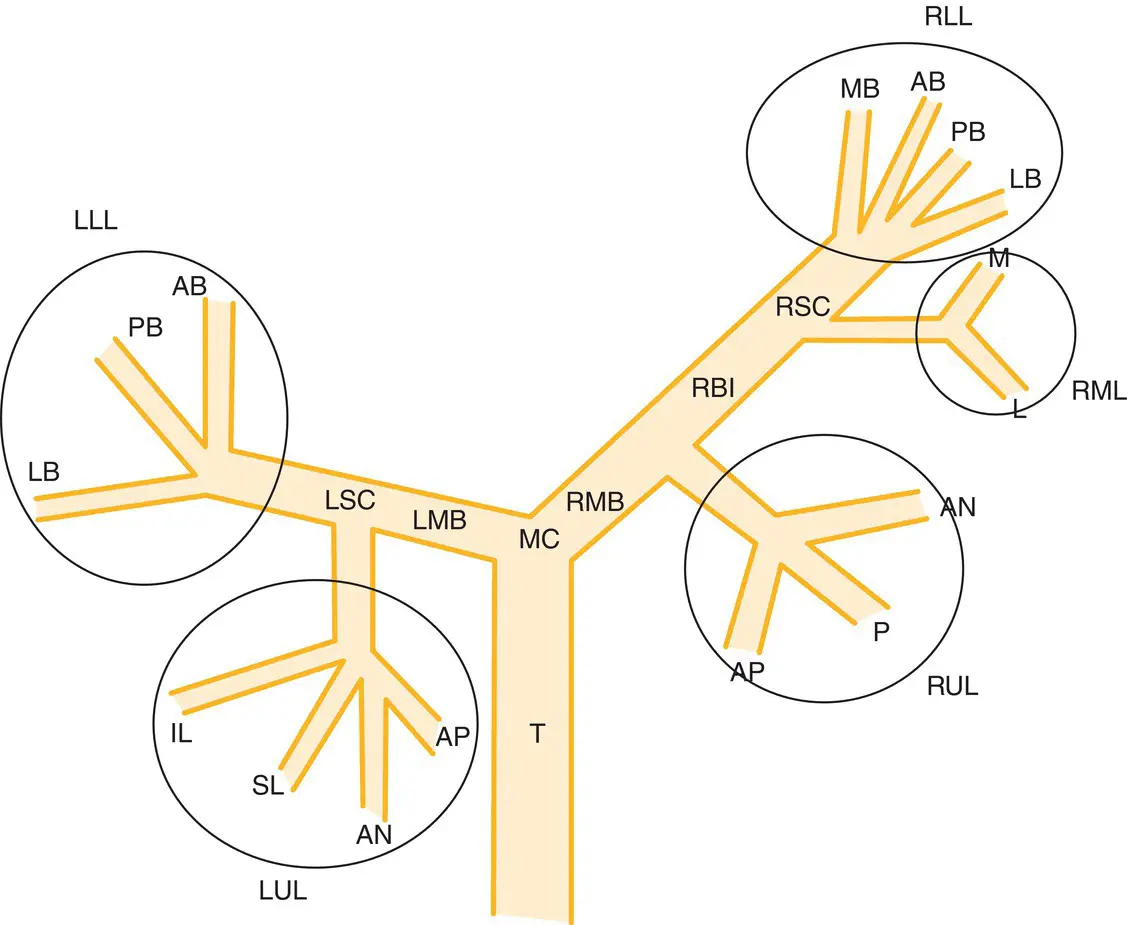
Figure 5.1 Simplified diagram of the bronchial tree (not drawn to scale), which is easily visualized by the bronchoscopist standing at the head of the bed, behind the patient. T, trachea; MC, main carina. Right bronchus : RMB, right mainstem bronchus; RBI, right bronchus intermedius; RSC, right secondary carina; RUL, right upper lobe: AN, anterior; AP, apical; P, posterior; RML, right middle lobe: L, lateral; M, medial; RLL, right lower lobe: AB, anterior basal; LB, lateral basal; MB, medial basal; PB, posterior basal. Left bronchus : LMB, left mainstem bronchus; LSC, left secondary carina; LUL, left upper lobe: AN, anterior; AP, apico‐posterior; IL, inferior lingula; SL, superior lingual; LLL, left lower lobe: AB, anterior basal; LB, lateral basal; MB, medial basal.
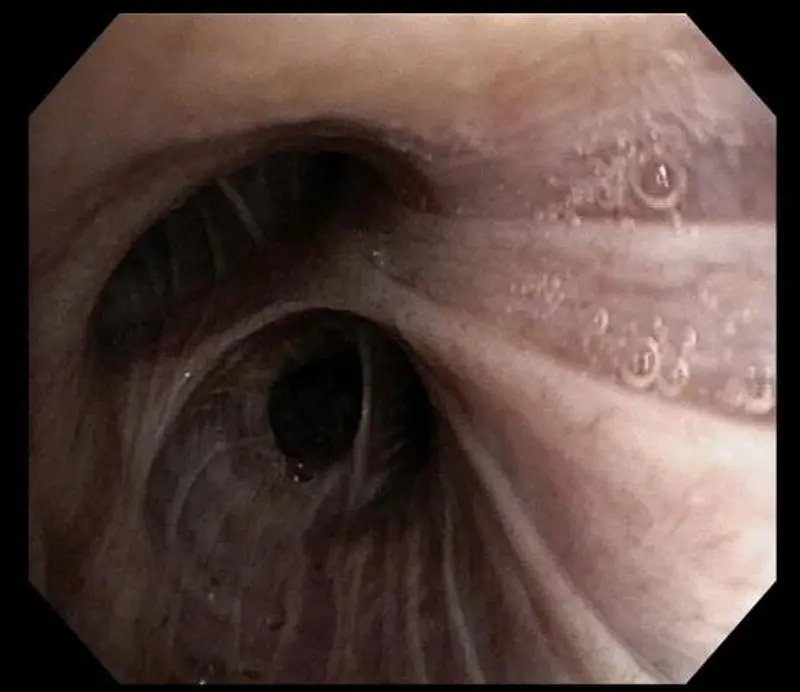
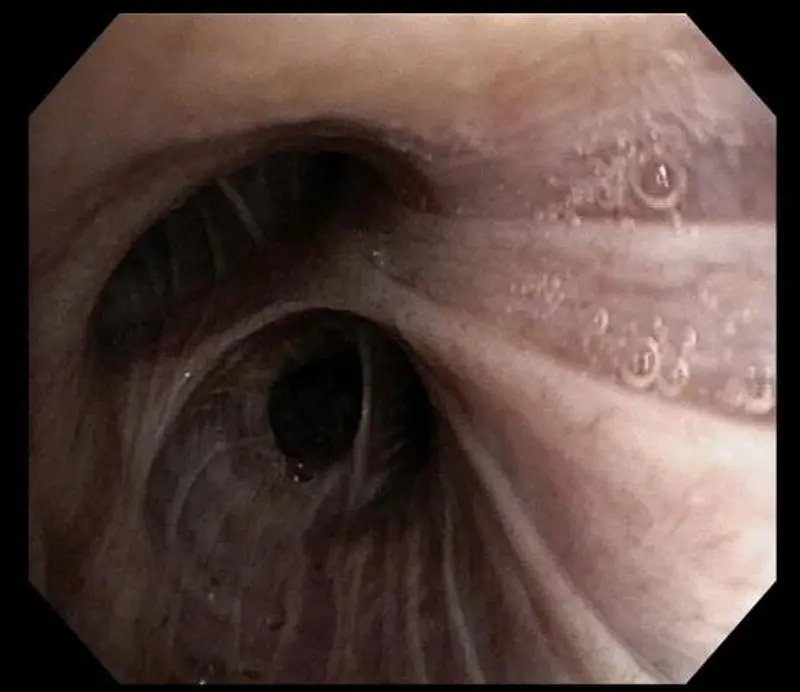
Figure 5.2 Right upper lobe.
Additional material for this chapter can be found online at:
www.wiley.com/go/mayer/mountsinai/criticalcare
This includes multiple choice questions and Videos 5.1, 5.2 and 5.3. The following image is available in color: Figure 5.2. 
CHAPTER 6 Bedside Percutaneous Dilational Tracheostomy
George Coritsidis1 and Viren Kaul2
1Icahn School of Medicine at Mount Sinai, New York, NY, USA
2Crouse Health, Syracuse, NY, USA
The bedside percutaneous dilational tracheostomy (PDT) with a minimal tracheostomy incision utilizes the Seldinger technique and gradual dilation to insert the tracheostomy.
PDT is a safe procedure in the critical care setting and should be first choice when available. Its use is more cost‐effective and trends towards fewer complications compared with open surgical tracheostomy.
Proper selection of the bedside candidate requires a hemodynamically stable patient with no bleeding diatheses and normal neck anatomy.
PDT is associated with less bleeding than open tracheostomy. Patients on anticoagulation or with severe derangements of INR or platelet count may either be supplemented with the appropriate blood products or deferred until stable for the procedure.
Bronchoscopic guidance is often used during bedside tracheostomy procedures, but is not routinely required since it has not demonstrated better outcomes. Those not routinely using a bronchoscope may reserve its use for difficult cases.
Surgical tracheostomy has been performed since 1909.
Percutaneous tracheostomy using the Seldinger technique allows tracheostomy placement at the bedside in the ICU.
Tracheostomy benefits ( Table 6.1)
Tracheostomy is considered for the patient who is expected to require a prolonged course of mechanical ventilation or requires an artificial airway for obstruction or secretion clearance.
For patients requiring mechanical ventilation for more than 2 weeks, it is believed that tracheostomy may be beneficial in avoiding continued injury to the vocal cords.
Tracheostomy may be better tolerated and allow a reduction of sedation. As a consequence it facilitates physical therapy, nursing care, and transfer of the ventilated patient out from the ICU setting.
Weaning from mechanical ventilation is also expedited due to the decreased work of breathing from a reduction of airway resistance and dead space.
Other benefits include patient comfort such as the initiation of oral intake, communication, and mobility, and possibly fewer respiratory infections.
Table 6.1 Risks and benefits of tracheostomy.
| Benefits |
Risks |
| Secure airway Expedite weaning or transfer from ICU Facilitate nursing care Communication Patient comfort and eating Mobility/physical therapy |
Pneumothorax Tracheo‐innominate artery fistula |
Early versus late tracheostomy
Early tracheostomy is variably defined, and generally performed within 4 days of intubation.
Earlier tracheostomy is considered if the likelihood of intubation is recognized to be prolonged beyond 2 weeks.
Patient discomfort secondary to translaryngeal intubation and multiple failed extubation attempts may also support earlier tracheostomy.
The benefits for earlier intervention are not clear. In some studies, such as in patients with traumatic brain injury or subarachnoid hemorrhage, reductions in length of stay (LOS) and pulmonary infections have been seen. However, in these neurosurgical populations, patients are often considered for earlier tracheostomy due to mental status issues and fear of weaning. A review and meta‐analysis also indicated early tracheostomy placement reduced the duration of mechanical ventilation and hospital stay.
There is no definitive mortality benefit for early tracheostomy.
In general, the decision for tracheostomy should begin with an evaluation of the patient within a week of intubation as to the likelihood of extubation in the upcoming week. The first week’s course is often predictive of ventilator dependency.
Читать дальше