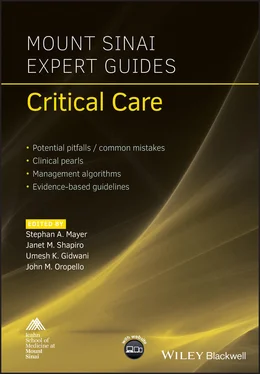
Mount Sinai Expert Guides
Здесь есть возможность читать онлайн «Mount Sinai Expert Guides» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Mount Sinai Expert Guides
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Mount Sinai Expert Guides: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Mount Sinai Expert Guides»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Mount Sinai Expert Guides — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Mount Sinai Expert Guides», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Identify following normal lung findings ( Figure 4.5and Video 4.1):Pleural line: shimmering echogenic line at top of screen.Lung sliding: periodic movement of pleural line; represents movement of visceral and parietal pleura relative to chest wall.A‐lines: repetitive horizontal artifact resulting from reverberation of US waves between skin and pleural surface; space between A‐lines equal to distance between probe head (on skin surface) and pleural line.Seashore sign: graphical visualization of lung sliding in M‐mode; often described as ‘waves on a sandy beach’ (waves represent motionless chest wall, sandy beach represents air‐filled lung).B‐lines: vertical artifact arising from pleural surface; appears like laser beam that effaces A‐lines and projects to bottom of screen. Usually do not see B‐lines anteriorly; may see a few (1–3) posteriorly in dependent regions in normal scans.
Slide probe vertically down chest wall to examine adjacent interspaces.
Repeat this process in systematic fashion along anterior, lateral, and posterior chest wall.
Clinical application
Assess for pneumothorax:
Absence of lung sliding plus absence of B‐lines (Video 4.2).
Barcode or stratosphere sign: parallel horizontal lines indicating absence of lung sliding in M‐mode ( Figure 4.6).
Lung point sign: transition point – between border of pneumothorax and normal pleural interface – where intermittent lung sliding is visualized. It is pathognomonic and helpful in estimating size of pneumothorax. Table 4.4 Features of cardiogenic pulmonary edema and non‐cardiogenic lung injury.Cardiogenic pulmonary edemaNon‐cardiogenic lung injuryHomogenous B‐line distributionSmooth pleural lineAbsence of A‐line patternNon‐homogenous B‐line distributionIrregular pleural surface
Assess for pleural effusion:Effusion appears as anechoic area usually in dependent areas; important to examine posterior chest wall in supine patient.Lung flapping or jellyfish sign: collapsed lung floating in pleural effusion ( Figure 4.7).
Assess for pulmonary edema and consolidation ( Table 4.4):Diffuse B‐lines (more than three in single field) is abnormal ( Figure 4.8).Consolidated lung appears isoechoic with liver, referred to as ‘hepatization’ ( Figure 4.9).Sonographic air bronchograms appear as punctuate hyperechoic foci.
BOTTOM LINE/CLINICAL PEARLS
Do not mistake chest wall for pleural line.
While absence of lung sliding suggests pneumothorax, it can occur in a variety of other situations such as pulmonary fibrosis and contusions, bullous emphysema, mainstem intubation, and pleurodesis.
Routinely check for lung sliding before and after any transthoracic procedure to evaluate for iatrogenic pneumothorax, e.g. central venous access.
Examining for pleural effusion with head of bed elevated may improve sensitivity as fluid will accumulate above diaphragms.
Abdomen
Probe selection and orientation
Use phased array ‘cardiac’ probe or curvilinear probe.
Point probe indicator toward patient’s right side or head (general radiology convention).
Scanning technique
Morison’s pouch with hemothorax view. Position probe with indicator pointing toward patient’s head at the right mid‐axillary line near the lower intercostal spaces. Identify the liver and kidney. Slide probe cephalad to look for pleural fluid and caudal to look for intraperitoneal free fluid ( Figure 4.10).
Splenorenal recess with hemothorax view. Position probe with indicator pointing toward patient’s head at the left posterior–axillary line near the lower intercostal spaces. Identify the spleen and kidney. Slide probe cephalad and caudal similar to Morison’s pouch view.
Bladder view. Position probe just above pubic bone and angle caudally. Point indicator toward patient’s right side to obtain transverse view and toward head to obtain sagittal view. Rock the probe to scan entire bladder and look for free fluid ( Figure 4.11).
Renal view. Locate right and left kidneys using same landmarks as Morison’s pouch and splenorenal recess views, respectively. Rock the probe to scan entire kidney.
Abdominal aorta view. Position probe high in the epigastrium with indicator pointing toward patient’s right to obtain transverse view. Identify the aorta on patient’s left and IVC on patient’s right side. Scan aorta starting in the epigastrium and towards the umbilicus until the iliacs come into view. Obtain at least three transverse views and measure aortic diameter using calipers. Point probe toward patient’s head to obtain sagittal view from celiac to illiacs.
Clinical application
Assess for intraperitoneal free fluid:Morison’s pouch is the most dependent area in the upper peritoneum when a patient is supine.The pelvis is the most dependent area of the peritoneum and the most likely place to see free fluid.
Assess the urinary tract:To evaluate anuria/oliguria, perform a renal and bladder scan to look for urinary tract obstruction.Hydronephrosis appears as an anechoic area or ‘bear paws’ at center of kidney.Degree of hydronephrosis is related to degree of urinary tract obstruction.Distended, fluid‐filled (anechoic) bladder indicates bladder outlet obstruction.Bilateral hydronephrosis with normal/empty bladder indicates compression of both ureters.
Assess for aortic aneurysm:Abdominal aortic aneurysm is defined as aortic diameter >3.0 cm.
BOTTOM LINE/CLINICAL PEARLS
Scan thoroughly in multiple windows to evaluate for intraperitoneal free fluid.
Do not mistake renal cysts for hydronephrosis. Cysts are generally located at the periphery of the kidney.
Aneurysms often contain thrombi. Measure aorta from outer wall to outer wall to avoid mistaking thrombus for aortic wall and obtaining a falsely decreased aortic diameter measurement.
Leg vein ultrasonography
Probe selection and orientation
Use linear array ‘vascular’ probe.
Point probe indicator toward patient’s right side (general radiology convention).
Scanning technique
To optimize patient positioning, slightly abduct and externally rotate hip.
Start by placing probe in transverse position along inguinal crease and locating common femoral vein (CFV).
Compress vein firmly with transducer. If vein does not completely collapse despite applying enough pressure to deform the artery, a clot is likely present.
Scan down medial thigh toward bifurcation of the CFV into the superficial and deep femoral veins. Compress every centimeter to systematically evaluate for clot.
Lastly, place probe behind knee in popliteal fossa and locate popliteal vein which lies superficial to the artery. Compress vein firmly to assess for clot.
Clinical application
Assess for leg vein thrombosis ( Figure 4.12).
BOTTOM LINE/CLINICAL PEARLS
Elevate head of bed or place patient in reverse Trendelenburg to maximize venous distension of lower extremities.
Do not assume an anechoic lumen is a patent lumen. An acute clot may be anechoic.
Baker’s cyst or lymph nodes may be mistaken for clot.
Table 4.5 RUSH exam protocol.
| RUSH exam | Hypovolemic shock | Cardiogenic shock | Obstructive shock | Distributive shock |
|---|---|---|---|---|
| Pump | Hyperconstractile heart Small heart size | Hypoconstractile heart Dilated heart size | Pericardial effusion RV strain Hyperconstractile heart | Hyperconstractile heart (early sepsis) Hypoconstractile heart (late sepsis) |
| Tank | Flat IVC Flat IJV Peritoneal fluid Pleural fluid | Distended IVC Distended IJV Lung rockets Pleural effusions, ascites | Distended IVC Distended IJV Absent lung sliding (PTX) | Normal/small IVC Normal/small IJV Pleural fluid (empyema) Peritoneal fluid (peritonitis) |
| Pipes | AAA Aortic dissection | Normal | DVT | Normal |
Management/treatment algorithm
Интервал:
Закладка:
Похожие книги на «Mount Sinai Expert Guides»
Представляем Вашему вниманию похожие книги на «Mount Sinai Expert Guides» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Mount Sinai Expert Guides» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.