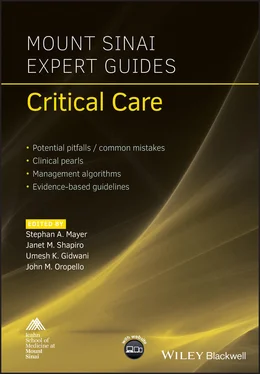
Mount Sinai Expert Guides
Здесь есть возможность читать онлайн «Mount Sinai Expert Guides» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Mount Sinai Expert Guides
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Mount Sinai Expert Guides: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Mount Sinai Expert Guides»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Mount Sinai Expert Guides — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Mount Sinai Expert Guides», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Open surgical tracheostomy versus bedside PDT
Bedside approaches are performed either as open, cut‐down procedures or via PDT using the Seldinger method. The Seldinger method is essentially a blind procedure done at the bedside.
The primary advantages to the bedside approach are the more efficient use of OR time and the consequent cost savings, which include those of patient transportation and general anesthesia.
Further advantages of PDT include smaller incisions, decreasing the likelihood for poor wound healing, scarring, and peristomal bleeding, and reduced local site infections. The procedure can also be more timely.
LOS in the ICU as well as time to placement of the tracheostomy is significantly shortened with PDT, suggesting further cost savings when using bedside procedures.
Most importantly, major complications and mortality are similar between PDT and open surgical tracheostomy. This is regardless of whether the bedside procedure is PDT or open.
Risk factors
Consent for procedure includes the risks of: pneumothorax (PTX), tracheo‐innominate artery fistula, airway damage and stenosis, bleeding, infection, and death.
Mortality of this procedure is less than 1%, while major morbidity is 5–10%.
Bleeding with PDT is minimal. Prior ultrasonography of the trachea assesses for any smaller crossover veins, which are uncommon but may cause bleeding.
PTX is a serious complication that can be fatal if not immediately recognized and treated. It presents with difficulty in ventilation, hypotension, and/or oxygen desaturation due to tension PTX, and often within minutes of the tracheotomy. Chest tube kits should be readily available during these procedures.
Innominate artery fistula can either be a relatively early or late event, and is a surgical emergency. A surgeon should immediately assess any bleeding from the tracheostomy site since any manipulation of the tube may undo the (possibly life‐saving) tamponade effect on the fistula.
Tracheal stenosis and tracheomalacia can be late complications at the tracheostomy site.
Selection of candidates for bedside PDT
Patient’s history and clinical status
Indication for tracheostomy: failed weaning/extubation, relief of airway obstruction or secretions.
Review surgical history for prior neck surgery, tracheostomy, or radiotherapy to the anterior trachea/neck.
Hemodynamic stability, stable cardiac condition.
Lack of bleeding, intact coagulation profile (preferably INR <1.5 and platelet count >50 000).
Absent severe sepsis.
In making the decision for PDT, it is important to keep in mind that this is an otherwise elective procedure so care must be taken to avoid potential complications.
Examination of candidates
The ideal patient for PDT has a well‐defined anatomy – a long thin neck, with palpable tracheal spaces that can be hyperextended safely. The first criterion safeguards the anatomy for this essentially blind procedure: namely that the tracheotomy is done between the third and fourth tracheal cartilage. The splaying of the cartilage rings is key in the proper positioning of the patient for PDT. In general, patients with recent neck injuries, morbidly obese necks, and previous tracheostomy or neck irradiation are contraindicated for bedside PDT. Anterior infection or burns of the neck, as well as goiter or masses, are also contraindications. Such patients are better relegated to an open surgical procedure.
If cervical spinal injury is present, PDT is contraindicated, and if in question, neurosurgical or neurological clearance for hyperextension would be necessary. Patients whose neck cannot be hyperextended such as patients with cervical osteoarthritis are also better treated in the OR. Note: PDT is not meant for acute emergency tracheotomies where the more cephalad cricothyroid membrane is the anatomy of choice for the tracheotomy.
The physical exam concentrates on identifying adenopathy, burns, infection, masses, scars (previous surgery or old tracheostomy scar), trauma, and thyromegaly (goiter). Review the skin surface for small veins to avoid lacerating during the procedure. If available, US examination can assist in identifying any aberrant vasculature or other anomalies that may defer PDT to an operative procedure.
Assess the extent of neck hyperextension. Is the neck short and thick? Is extension not possible due to cervical arthritic changes? Inability to palpate the tracheal anatomy due to obesity or short neck length, and/or inability to hyperextend allowing at least two finger breaths above the sternal notch would contraindicate the procedure.
Patients with obese necks may have successful PDT although they may require bronchoscopic assistance, cut down, and longer tracheostomy tubes. The patient must be hemodynamically stable as significant sedation and/or paralysis may be needed for the procedure. The most common reason to prolong the PDT procedure is sedation‐related hypotension necessitating intravenous fluids or vasopressors. Assessing the degree of hyperextension earlier will require full sedation, indicating the need for fluid resuscitation prior to the procedure. Also be aware that bradycardia due to vagal effects may worse.
The patient should have satisfactory gas exchange, not requiring high PEEP.
Relative contraindications
Anatomic:Previous tracheostomy, surgery.Skin infection or burns.Short obese neck, goiter, adenopathy, mass.Spinal injury, lack of hyperextension.
Physiology:Bleeding diathesis.High O2 requirements (high PEEP).Hemodynamically unstable.Poor nutrition status.
PDT procedure
The procedure (Video 6.1) can be performed in a critical care unit with continuous monitoring.
Patient must be NPO for at least 6 hours and subcutaneous heparin is withheld prior to the procedure.
All appropriate sterile precautions must be employed, using sterile gowns, masks, gloves, and drapes along with the PDT kits.
Procedure without bronchoscopic guidance
Start by providing appropriate sedation. Fentanyl and propofol are given to the patient, ideally as an infusion, and titrated so the patient is motionless, without cough or gag, when palpating the trachea. If hypotension develops, the decision to provide fluids, vasopressors, and to continue the procedure are made jointly between the surgeon and anesthesiologist. Paralysis is not a requirement for this procedure and is reserved for those patients with movement despite adequate sedation.
After sedation is achieved, a roll is placed midline under the scapula to facilitate hyperextension of the neck ( Figure 6.1). The head is ideally hanging in air unless you place a pillow underneath. This positioning may arouse the patient if they are not adequately sedated.
Prepare the PDT kit ( Figure 6.2): test the tracheostomy tube (TT) cuff for patency, and remove all air after testing; adequately lubricate the TT and trochanter; prepare the guidewire; fill the subcutaneous and catheter syringes with 1% lidocaine/epinephrine; and hydrate the dilator with saline flush.
Increase the oxygen to 100% FiO2; suction the endotrachea (ET) and mouth for secretions; clean the anterior neck and inject lidocaine/epinephrine subcutaneously two fingers above the sternal notch and midline. The respiratory therapist then deflates the ETT cuff while increasing the tidal volume to compensate for creating a leak (add 100 mL to the tidal volume).
Palpate your needle puncture point at two fingers above the sternal notch and two cartilage rings below the cricoid cartilage. The needle is advanced in a perpendicular position midline on the trachea.At the midline position of the trachea there is no muscle or vasculature. The sternocleidomastoid, sternohyoid, and sternothyroid are lateral. A puncture too high will result in difficulties with the cartilage; too low may result in erosion of the tracheostomy tube into the innominate artery creating a fistula.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Mount Sinai Expert Guides»
Представляем Вашему вниманию похожие книги на «Mount Sinai Expert Guides» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Mount Sinai Expert Guides» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.