Suggested course of action
Incisional biopsy to assess for dysplasia or carcinoma or referral to an oral and maxillofacial surgeon.
If only premalignant changes are seen on the biopsy, a wide local excision together with skin grafting the defect is accomplished. If invasive carcinoma is identified on the biopsy, a wide local excision and ipsilateral neck dissection is accomplished together with flap reconstruction.
Dyskeratosis Congenita
Nature of disease
A very rare autosomal dominant disorder involving mutations in six genes that code for telomerase, thereby increasing a cell’s life span. Forty percent of oral lesions gradually progress to invasive squamous cell carcinoma.
Begins in childhood. No sex or racial predilection is known.
Oral lesions of the labial and buccal mucosa will appear white and are frequently thick. Lesions become thicker with age. Skin telangiectasias are common as well as a smooth dorsal tongue surface from loss of filiform papillae. Atrophic nail beds may also be seen.
Radiographic presentation
None.
In younger individuals, hereditary benign intraepithelial dyskeratosis, white sponge nevus, and pachyonychia congenita are considerations. In adults, lichen planus and squamous cell carcinoma are added to these.
In early lesions, acanthosis and hyperkeratosis are seen. As lesions age, epithelial dysplasia and squamous cell carcinoma may be seen.
Suggested course of action
Close follow-up observing for clinical suggestions of premalignant or malignant changes (ie, ulceration, induration, pain, increase in size, lymphadenopathy, etc). Biopsy as necessary, or refer to an oral and maxillofacial surgeon.
Excision of lesions as they show signs of malignant transformation.

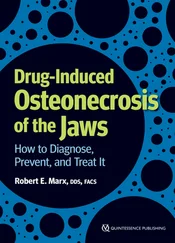
 Erythroleukoplakia representing carcinoma in situ.
Erythroleukoplakia representing carcinoma in situ.
Epithelial Dysplasia/Carcinoma in Situ
Nature of disease
Premalignant alterations in the epithelium from genetic alterations in the basal cell layer due to either carcinogens, human papillomaviruses, heredity, or errors in cellular division.
Mostly seen in adults but may be rarely seen in patients with congenital dysplastic syndromes. No sex or racial predilection is known. More commonly seen on the lateral border of the tongue or floor of the mouth.
A white or red-white surface lesion without induration. Pain is not usually present. Ulceration is not present unless a focal area of invasive carcinoma exists within the lesion.
Radiographic presentation
None.
Benign hyperkeratosis, lichen planus, and candidiasis should be considered along with invasive squamous cell carcinoma.
The basement membrane should be intact, and a variable degree of inflammation is seen beneath the basement membrane. The epithelium will show varying degrees of nuclear pleomorphism and cell size and a lack of cellular maturation from the basement membrane to the surface. Mitotic figures and individual cell keratinization may also be seen.
Suggested course of action
Suspicious lesions should be biopsied or referred to an oral and maxillofacial surgeon for evaluation, biopsy, and treatment.
After confirmation by biopsy, a wide local excision with frozen section assessment of margins is accomplished. If multiple sections of the main specimen identify an area of invasive squamous cell carcinoma, the area is re-treated with a re-excision and a neck dissection is considered after a metastatic workup is accomplished.

 Striaform lichen planus.
Striaform lichen planus.
Hypertrophic and Striaform Lichen Planus
Nature of disease
A mild T cell–mediated autoimmune disease that attacks the basal cell layer and basement membrane at the interface between the epithelium and the subjacent connective tissue.
Adults over 40 years of age. No sex or racial predilection is known. Mostly seen on the buccal mucosa but may also be seen on the tongue and attached gingiva.
The striaform type presents as asymptomatic, lacy white lines referred to as Wickham striae . The hypertrophic type presents as an asymptomatic, irregular white hyperkeratotic patch.
Radiographic presentation
None.
The striaform type is distinctive but may resemble hereditary benign intraepithelial dyskeratosis or candidiasis. The hypertrophic type appears most like clinical leukoplakia, and therefore epithelial dysplasia, carcinoma in situ, proliferative verrucous leukoplakia, verrucous carcinoma, and invasive squamous cell carcinomas should be considered.
Both will show acanthosis with hyperkeratosis and a bandlike infiltrate subjacent to the basement membrane consisting of mostly (≥90%) lymphocytes as well as a disrupted basement membrane.
Suggested course of action
Clinically apparent striaform lichen planus requires reassurance to the patient of the usual mild and nonprogressive nature of the disease as well as its nonpremalignant biology. Hypertrophic lichen planus requires an incisional or excisional biopsy to rule out more serious diseases.
No specific treatment is required.

 Mucous patches from secondary syphilis.
Mucous patches from secondary syphilis.
Secondary Syphilis (Mucous Patches)
Nature of disease
The systemic second phase of an infection caused by Treponema pallidum .
In adults, secondary syphilis is a systemic progression from a primary syphilis lesion known as a chancre . In newborns, secondary syphilis arises from transplacental transmission from an infected mother to the fetus, and thus the child is born with secondary syphilis. No sex or racial predilection is known.
In adults, the lesions will appear as asymptomatic, flat, red-white lesions or patches of erythema with a pale peripheral ring. In newborns and children, T pallidum usually causes developmental disturbances such as the classic triad of mulberry molars, notched incisors, and tapered incisors (screwdriver teeth) known as Hutchinson’s triad . Additionally, saber-shaped shins, rhagades, interstitial keratitis, and a saddle nose deformity may variably be seen.
Читать дальше

 Erythroleukoplakia representing carcinoma in situ.
Erythroleukoplakia representing carcinoma in situ.