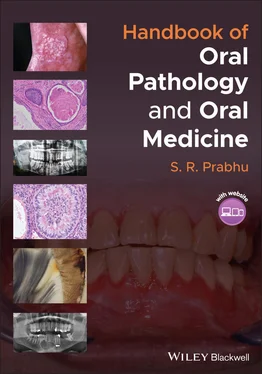
S. R. Prabhu - Handbook of Oral Pathology and Oral Medicine
Здесь есть возможность читать онлайн «S. R. Prabhu - Handbook of Oral Pathology and Oral Medicine» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Handbook of Oral Pathology and Oral Medicine
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:5 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 100
- 1
- 2
- 3
- 4
- 5
Handbook of Oral Pathology and Oral Medicine: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Handbook of Oral Pathology and Oral Medicine»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Discover a concise overview of the most common oral diseases in a reader-friendly book Handbook of Oral Pathology and Oral Medicine
Handbook of Oral Pathology and Oral Medicine
Handbook of Oral Pathology and Oral Medicine — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Handbook of Oral Pathology and Oral Medicine», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
3.2 Pulpitis
3.2.1 Definition/Description
Pulpitis refers to inflammation of the dental pulp. Types include:Reversible pulpitis: pulpal inflammation resolves once the aetiology is removedIrreversible pulpitis: pulpal inflammation does not resolve once the aetiology is removedChronic hyperplastic pulpitis (pulp polyp)
3.2.2 Frequency
Prevalence varies from country to country. Ranges from 27%‐54% of the population
Irreversible pulpitis is more common in females
3.2.3 Aetiology/Risk Factors
Caries
Traumatic exposure of the pulp
Fracture of the crown or cusp
Cracked tooth
Thermal or chemical irritation
3.2.4 Clinical and Radiographical Features
Reversible pulpitis:Pain from cold test does not linger for longer than 30 secondsNo percussion sensitivityNo spontaneous painNo heat sensitivity
Irreversible pulpitis:Pain from cold test lingers for longer than 30 secondsMay get pain from heat testMay have spontaneous painMay be percussion sensitiveSleep or work is affectedA patient may have difficulty locating the tooth from which the pain originatesRadiographically or clinically, deep caries may be visible
Chronic hyperplastic pulpitis:Presence of a pink fleshy mass filling a carious cavity (pulp polyp; Figure 3.1)Usually single, rarely involving multiple teethNon‐tender or mildly tenderBleeds readily on probing
3.2.5 Microscopic Features
Acute pulpitis:Pulpal hyperaemiaFocus of acute inflammatory cell infiltrate Figure 3.1 Chronic hyperplastic pulpitis (pulp polyp) presenting as a fleshy mass in the carious cavity (white arrow).Destruction of odontoblastsFormation of an abscess in some cases
Chronic pulpitis:Mononuclear cell infiltrate (chronic inflammatory cells)Focus of pulp necrosisAbscesses and pus formationWall of granulation tissue
Chronic hyperplastic pulpitis:Mass composed of granulation tissueRich vasculatureChronic inflammatory cell infiltrateStratified squamous epithelial lining covers the surface of granulation tissue
3.2.6 Differential Diagnosis
Periodontal pain
Dentin hypersensitivity
Cracked tooth syndrome
Dental trauma
Idiopathic orofacial pain
Pain from restorative procedures
Pain of non‐odontogenic origin
3.2.7 Diagnosis
Based on history, clinical examination and testing
Radiography detects carious lesions causing pulpitis
Thermal tests
Radiographical examination for clinically visible and non‐visible caries and for recurrent carries under restorations, lamina dura and periodontal ligament (PDL) space
3.2.8 Management
3.2.8.1 Reversible Pulpitis
Remove the irritant or repair tooth structure (caries, exposed dentin, defective restoration)
Continue to monitor the patient's symptoms
Advise patient to return if symptoms persist or worsen
Pain management with analgesics (ibuprofen and paracetamol)
Antibiotics are not required
3.2.8.2 Irreversible Pulpitis
Pulpectomy of the offending tooth: complete removal of the pulp
Root canal treatment
Pain management with analgesics
Antibiotics are not recommended
Extraction if tooth cannot be saved
3.2.8.3 Chronic Hyperplastic Pulpitis
Extraction of the tooth
3.3 Apical Periodontitis and Periapical Granuloma
3.3.1 Definition/Description
Apical periodontitis refers to inflammation of the PDL surrounding the apex of the tooth caused by infection, bacterial products, or other irritants through the apex of the root. Usually, this occurs due to acute inflammation (acute apical periodontitis)
Periapical granuloma, also known as chronic apical periodontitis, refers to formation of granulation tissue surrounding the apex of a non‐vital tooth arising in response to pulpal necrosis
3.3.2 Frequency
Prevalence of apical periodontitis shows variation
Prevalence increases with age; by 50 years of age, one in two individuals will experience apical periodontitis
In individuals over 60 years of age, the prevalence rises to 62%
3.3.3 Aetiology/Risk Factors
Bacterial invasion from the pulp
Occlusal trauma from the high spots of restorations
Irritants and inflammatory mediators from the necrotic pulp
Endodontic procedures (iatrogenic)
Gingival infection
3.3.4 Clinical Features
Apical periodontitis:Acute form is commonPain and tenderness of the tooth on slight touchMinutely extruded toothNo changes with hot and cold drinks or foodSequelae: may proceed to dental abscess or chronic apical periodontitis
Periapical granuloma:Most cases are asymptomaticTooth involved is non‐vitalTooth is slightly tender to percussion
3.3.5 Radiographical Features
Apical periodontitis:Usually, no significant changes seenOccasionally, lamina dura may show haziness or slightly wide periodontal space
Periapical granuloma:Presents as a radiolucent lesionA radiolucent lesion of a few millimetres in size is usually indistinguishable from a periapical cystAn affected tooth typically reveals loss of the apical lamina duraRoot resorption is not uncommonA radiolucent lesion associated with the root apex often has fuzzy borders ( Figure 3.2a) Figure 3.2 Periapical granuloma. (a) Radiolucent lesion of periapical granuloma at the root apex of the non‐vital lateral incisor. (b) Photomicrograph showing apical connective tissue (black star) with chronic inflammatory cells and proliferating epithelial cells. Microscopic features demonstrate an evolving periapical cyst arising from periapical granuloma(source: by kind permission of Associate Professor Kelly Magliocca, Department of Pathology and Laboratory Medicine, Winship Cancer Institute at Emory University, Atlanta, GA, USA).(c) This photomicrograph shows cholesterol clefts and multinucleated giant cells in a mature periapical granuloma. These features are similar to those of periapical cyst.
3.3.6 Microscopic Features
Apical periodontitis:Engorged blood vesselsIntense infiltration of neutrophils
Periapical granuloma:Chronically inflamed granulation tissue around apex of a non‐vital tooth shows:Lymphocytes, macrophages, and plasma cells intermixed with neutrophils and proliferating epithelial cells (cell rests of Malassez) within the granulation tissue ( Figure 3.2b)Cholesterol clefts with multinucleated giant cells, red blood cells, and areas of hemosiderin pigment ( Figure 3.2c)Uninflamed layers of fibrous tissue at the peripheryPresence of osteoclasts
Sequelae of periapical granuloma:Acute exacerbation can cause rapid enlargement of the lesion and may progress to abscess formationProliferation of the epithelial cell rests of Malassez associated with the inflammation may lead to the development of an inflammatory radicular cyst
3.3.7 Differential Diagnosis
Cracked‐tooth syndrome and acute periapical abscess to be differentiated from acute apical periodontitis
Periapical lesions presenting as radiolucent lesions in the apical region of the roots (e.g. periapical cyst, chronic periapical abscess) to be differentiated from periapical granuloma
Sometimes nasopalatine duct cyst (in maxillary anterior teeth) presents radiographical features mimicking those of periapical granuloma
3.3.8 Diagnosis
History
Clinical examination
Radiography
3.3.9 Management
Интервал:
Закладка:
Похожие книги на «Handbook of Oral Pathology and Oral Medicine»
Представляем Вашему вниманию похожие книги на «Handbook of Oral Pathology and Oral Medicine» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Handbook of Oral Pathology and Oral Medicine» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.