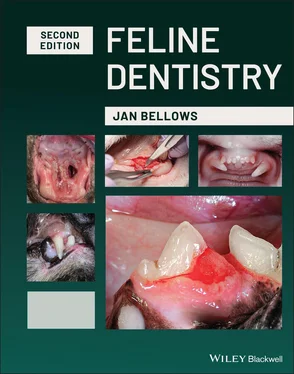
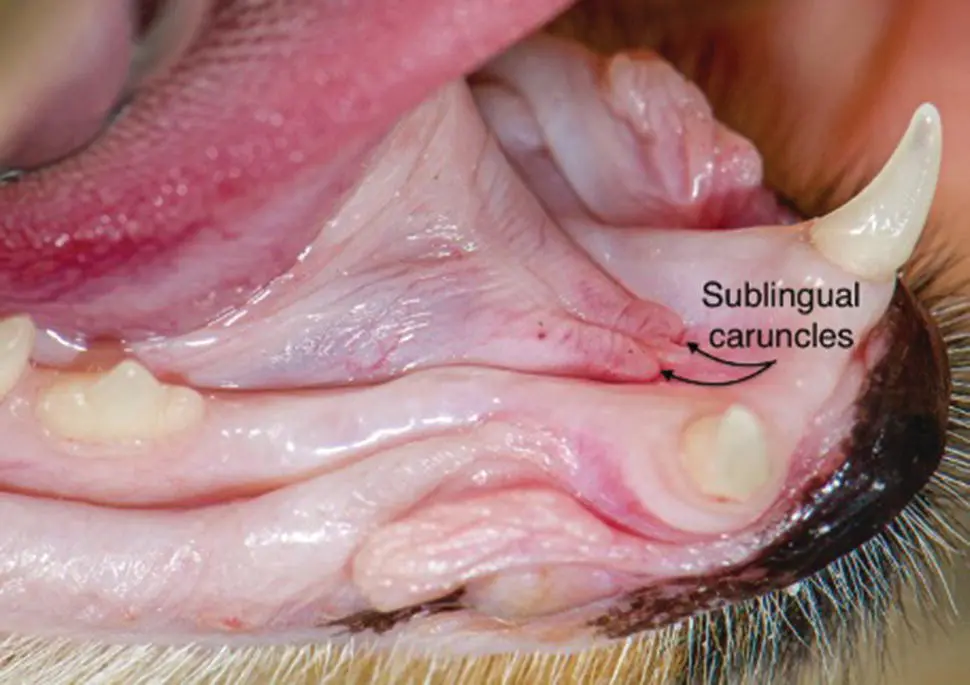
1 ...8 9 10 12 13 14 ...17 Saliva from the parotid gland exits at a papilla in the alveolar mucosa, just caudal to the maxillary fourth premolar. Saliva from the zygomatic gland exits at a papilla in the alveolar mucosa near the maxillary first molar. Saliva from the mandibular and sublingual glands enters the oral cavity through the sublingual caruncles located ventral and rostral to the base of the tongue ( Figure 1.4) ( Illustration 1.1).
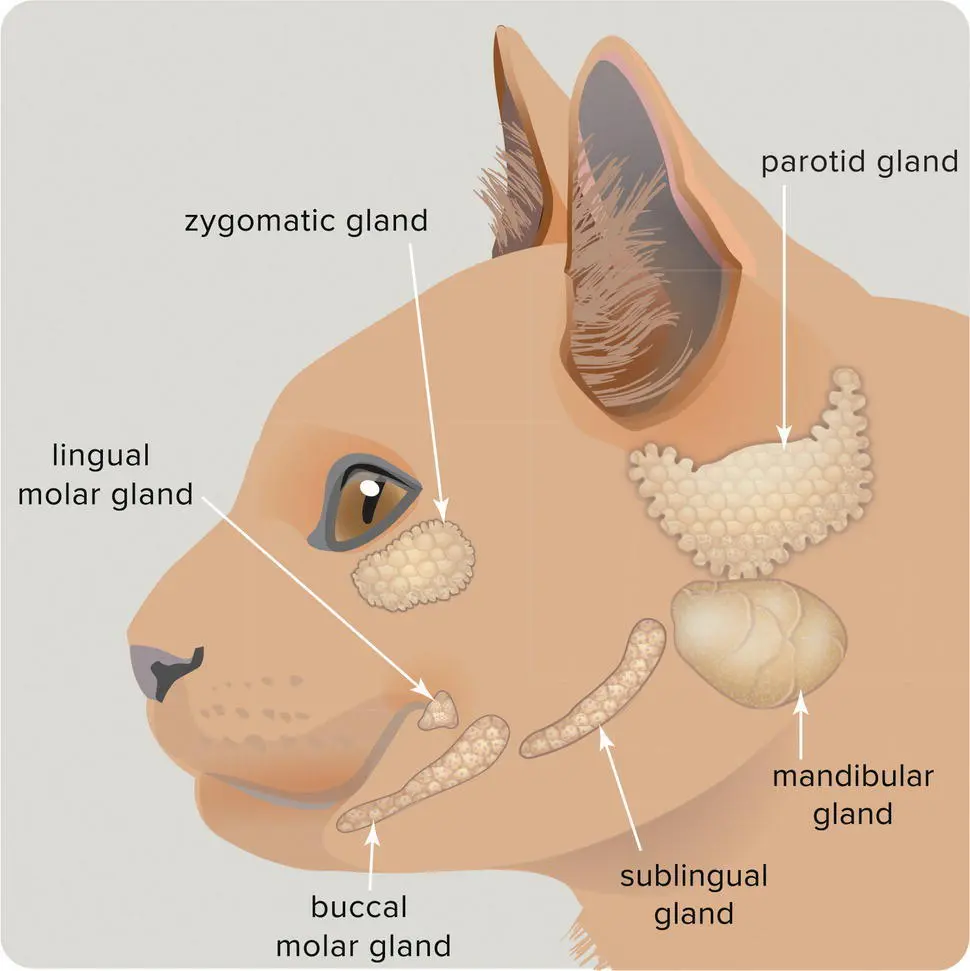
Cats have four molar salivary glands. The buccal molar glands empty into the oral cavity through several small ducts. The lingual molar glands are located in the membranous molar pad linguodistal to the mandibular first molar teeth ( Figure 1.5).
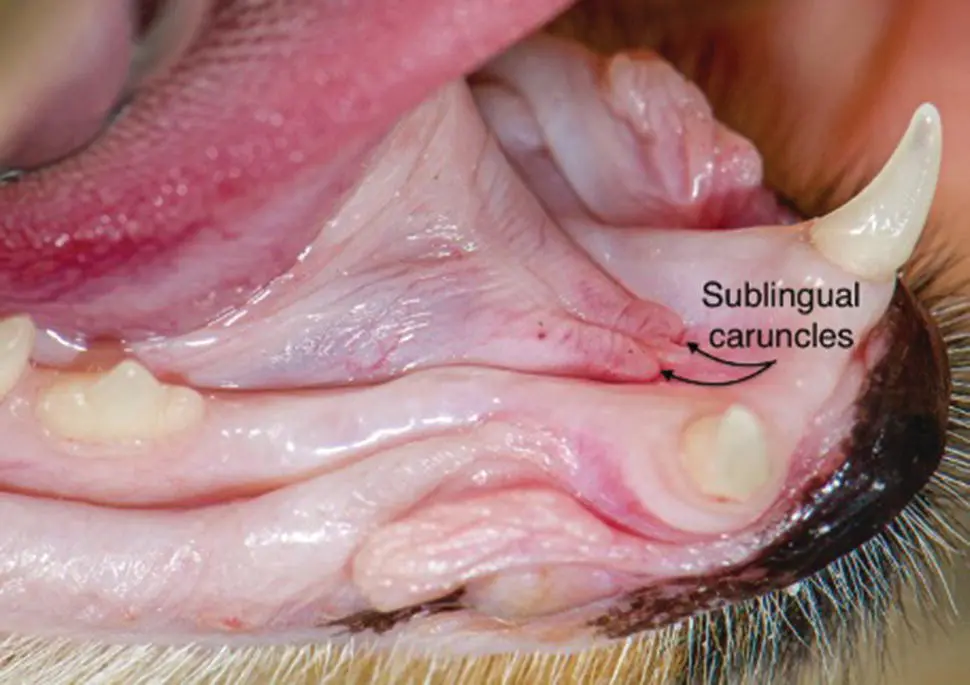
Figure 1.4 Sublingual caruncles.
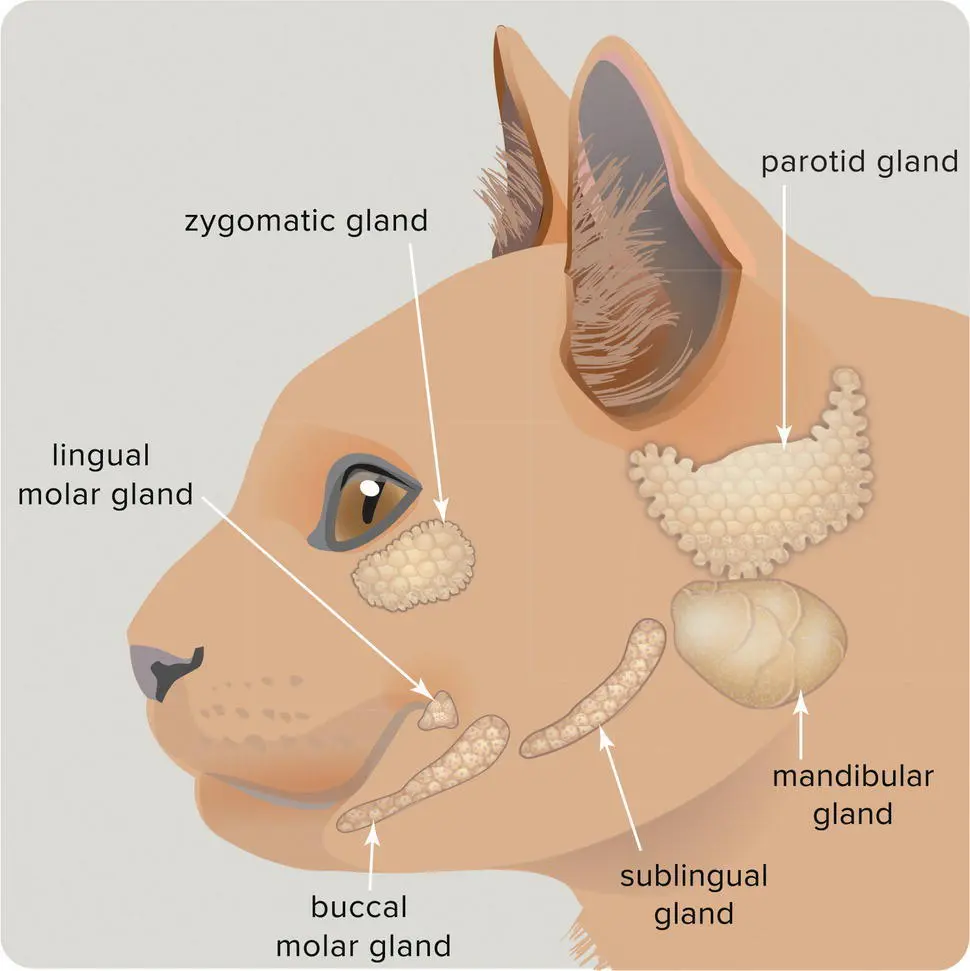
Illustration 1.1 Cat salivary glands.
Source: Image courtesy of Tamara Rees, Veterinary Information Network.
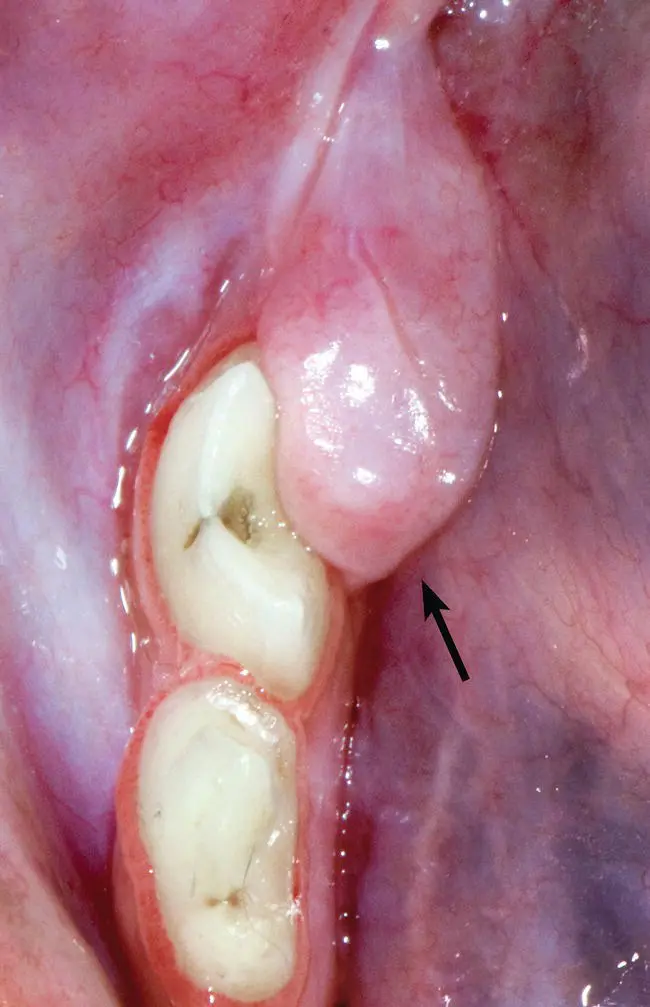
Figure 1.5 Membranous bulge linguodistal to the mandibular first molar tooth containing a minor salivary gland (lingual molar gland).
The term periodontium or periodontal apparatus is used to describe tissues that surround and support the teeth, including the gingiva, periodontal ligament, cementum, and alveolar bone.

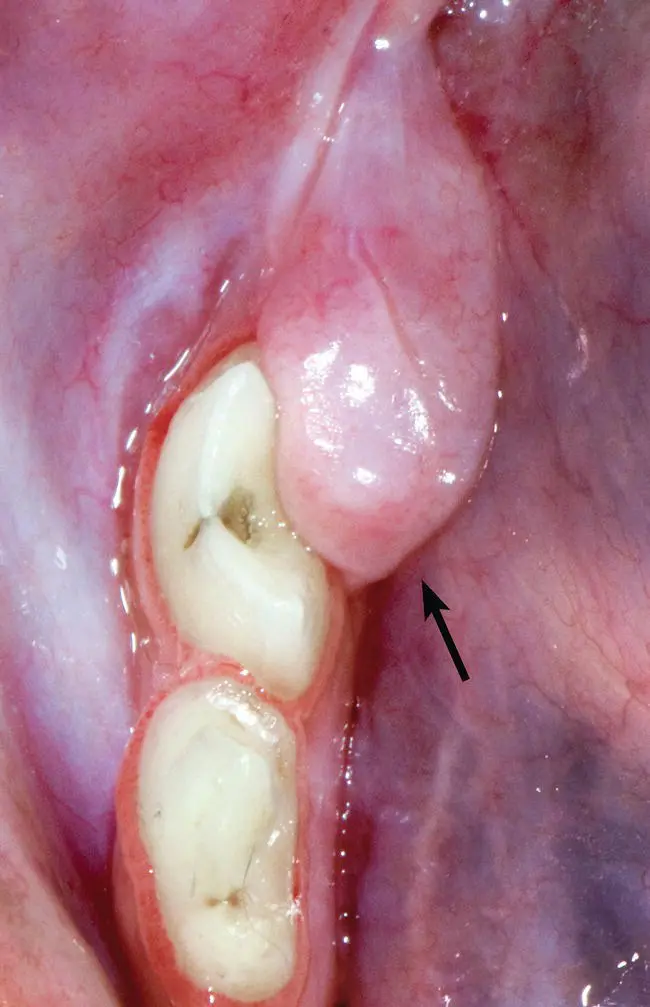
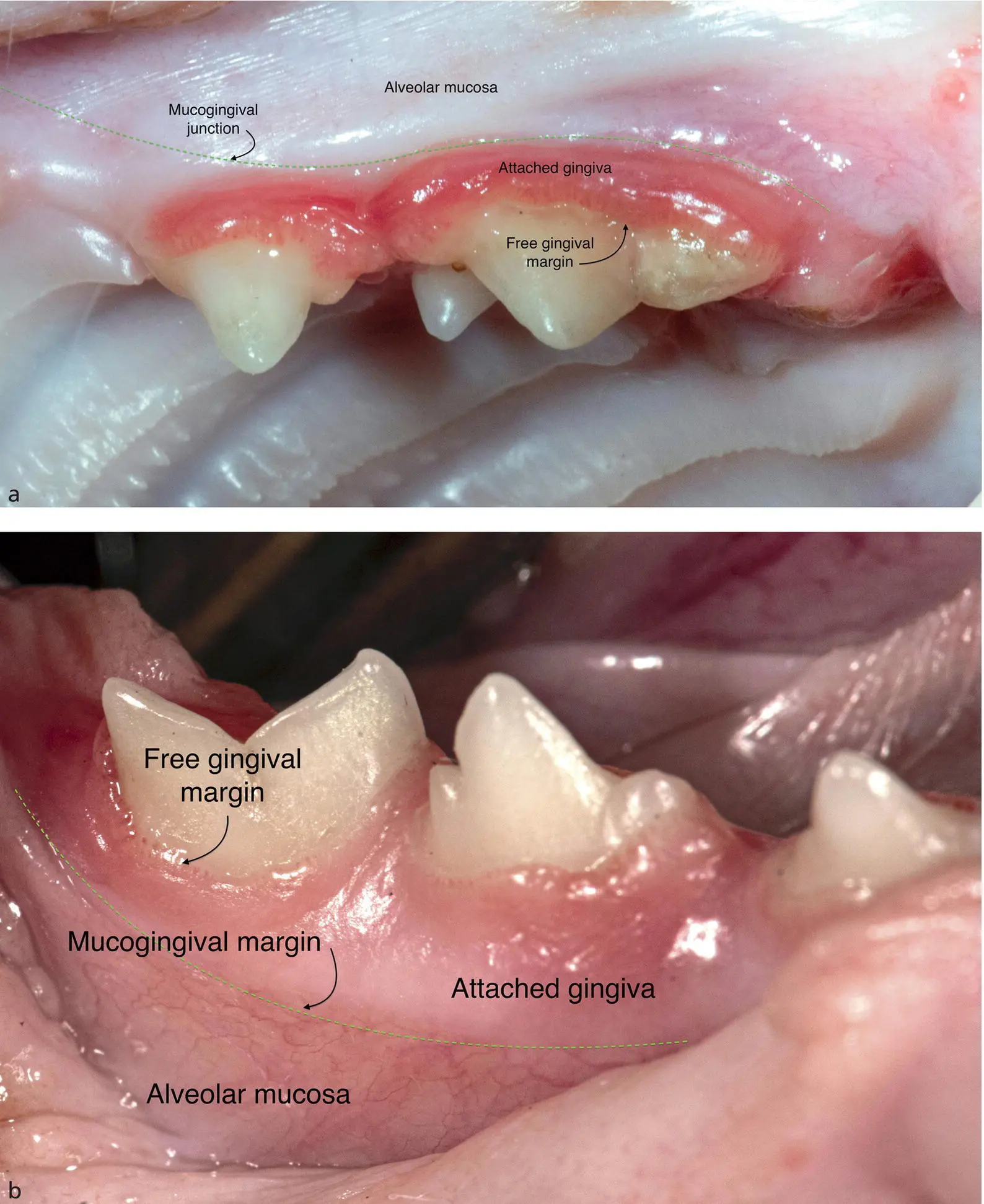
Figure 1.6 Oral mucosa in a patient with gingivitis, periodontitis, and caudal mucositis.
The cat's oral cavity is lined with keratinized and nonkeratinized stratified squamous epithelium. Gingiva refers to the keratinized oral mucosa that covers the alveolar process and surrounds the cervical portion of the tooth crowns. Unlike the epithelial lining of the digestive tract, the gingiva does not have absorptive capacity but acts as a physiologic permeable barrier that protects underlying structures from the invasion of microorganisms and other foreign substances ( Figure 1.6).
The gingival epithelium is composed of the following:
The oral epithelium, also called the outer gingival epithelium, is keratinized or parakeratinized and covers the oral surface of the attached gingiva and gingival papillae.
The sulcular epithelium is a nonkeratinized extension of the oral epithelium into the gingival sulcus. The bottom of the gingival sulcus in a periodontally healthy tooth should be slightly coronal to the cementoenamel junction.
The junctional epithelium attaches to enamel of the most apical portion of the crown by means of hemidesmosomes and lies at the floor of the sulcus, immediately coronal to or at the cementoenamel junction. The junctional epithelium and gingival connective tissue separate the periodontal ligament from the oral environment. The floor of the gingival sulcus is apically bounded by junctional epithelial cells.
Marginal gingiva is the most coronal (toward the crown) aspect of the gingiva that is not attached to the tooth but lies passively against it. When healthy, it appears coral‐pink and firm, with knife‐edged margins. Pigment may or may not be present. The space between the tooth and the marginal gingiva is the gingival sulcus (or crevice). The normal depth of the sulcus is less than 1 mm in cats.
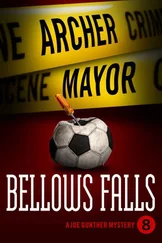
1.9.2 Free Gingival Margin
The free gingival margin is the coronal edge of the marginal gingiva. Marginal gingiva is demarcated from the attached gingiva by the gingival groove, a slight depression on the gingiva corresponding to the normal sulcus depth ( Figure 1.7a,b).
The healthy free gingival margin of premolars and molars lies 0.5–1 mm coronal to the cementoenamel junction, where root cementum meets the crown enamel.
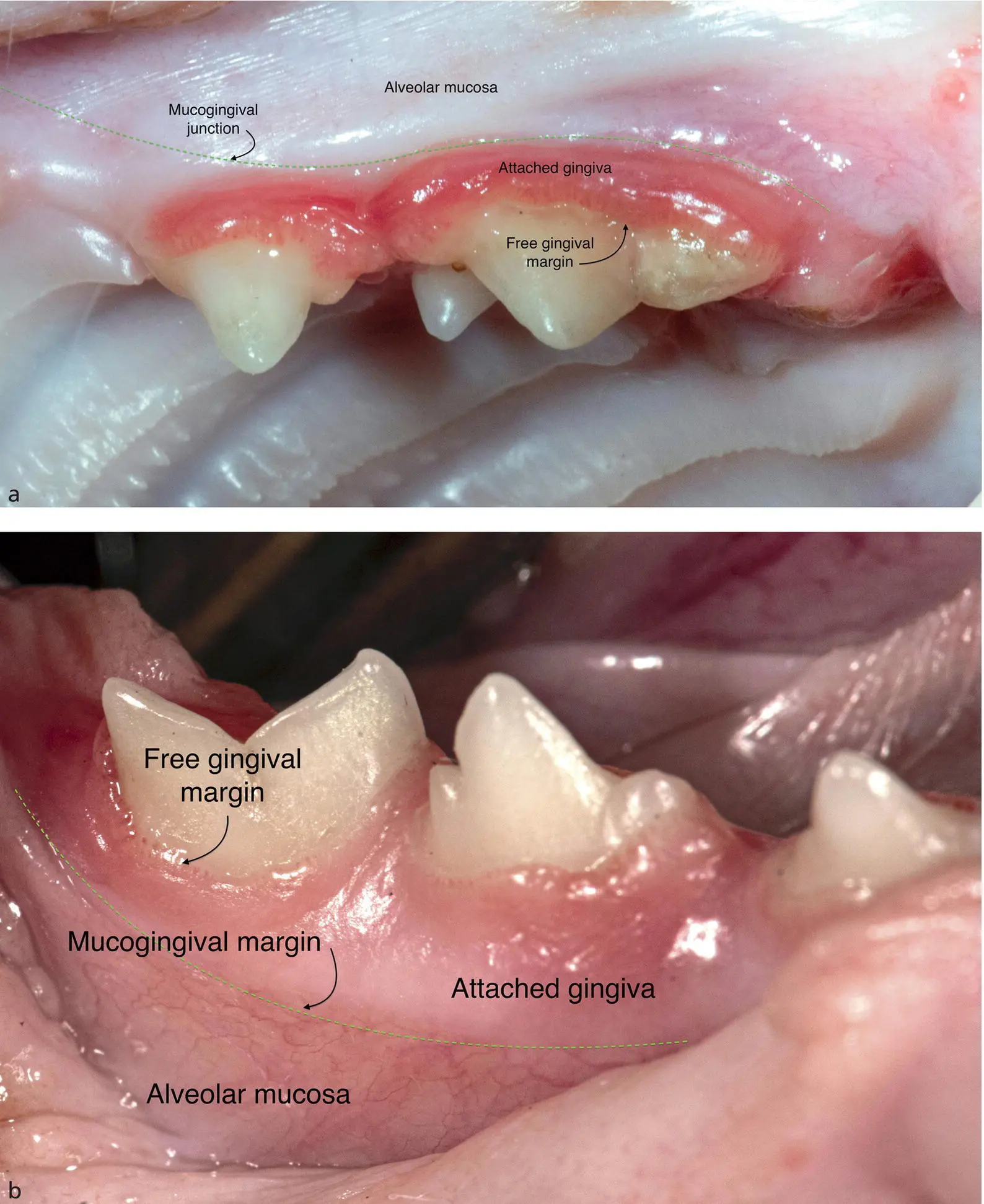
Figure 1.7 (a) and (b) Gingival structures surrounding the left maxillary (a) and right mandibular (b) cheek teeth.

Figure 1.8 Compressed air from an air/water syringe exposing the normal 0.5 mm sulcus surrounding the left maxillary fourth premolar.
The attached gingiva is located apical to the marginal gingiva and is normally tightly bound to the periosteum of alveolar bone. Attached gingiva is keratinized to withstand the stress of mastication. The width of the attached gingiva varies in different areas of the mouth. It is widest at the maxillary canines.
The firmly attached gingiva is contiguous with loose alveolar mucosa at the mucogingival junction, also referred as the mucogingival line. The mucogingival junction remains stationary throughout life, although the gingiva around it may change in height due to attachment loss or hyperplasia.
The gingival sulcus is a shallow space between the marginal gingiva and the tooth. The sulcus depth is generally under 1 mm but varies depending on the specific tooth and the size of the cat. In cases of periodontal disease, the abnormal sulcus is termed a pocket, which extends further apically due to destruction of the periodontium ( Figure 1.8).
1.10 Periodontal Ligament
The periodontal ligament is a dense, fibrous connective tissue that attaches the tooth root to the bony alveolus. The periodontal ligament also acts as a suspensory cushion against occlusal forces and as an epithelial attachment to keep debris from entering deeper tissues.
The blood supply to the periodontal ligament originates from the alveolar artery. Arterioles enter the ligament near the apex of the root and from lateral aspects of the alveolar socket and branch into capillaries within the ligament along the long axis of the tooth. Collagen fibers also run through these spaces. The blood vessels are closer to the bone than to the cementum. Venules drain the apex through apertures in the bony wall of the alveolus and into the marrow spaces. Cells commonly found in the periodontal ligament are fibroblasts, osteoblasts, cementoblasts, osteoclasts, cementoclasts, rest cells of Malassez, and undifferentiated mesenchymal cells (progenitor cells).
Nerve bundles enter the periodontal ligament through numerous foramina in the alveolar bone. They branch and end in small rounded bodies near the cementum. The nerves carry pain, touch, and pressure sensations and form an important part of the feedback mechanism of the masticatory apparatus.
The periodontal ligament has great adaptive capacity. It responds to chronic functional overload by widening to relieve the load on the tooth. Vascular communications between the pulp and periodontium form pathways for transmission of inflammation and microorganisms between the tissues ( Figure 1.9a,b).
Читать дальше