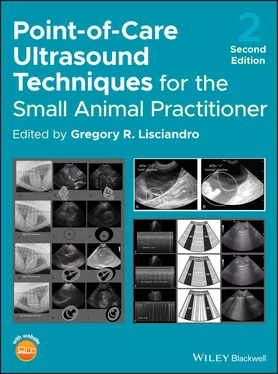
Lastly, AFAST was never meant to be a “flash exam,” meaning that it was never meant to only answer a single binary question of whether free fluid was present or absent ( Table 6.3). AFAST provides much more clinical information by:
Table 6.3. What clinical questions are answered using AFAST? Binary? Qualitative‐quantitive?.
Source: Reproduced with permission of Dr Gregory Lisciandro, Hill Country Veterinary Specialists and FASTVet.com, Spicewood, TX.
|
Binary |
Qualitative‐quantitive |
aSensitivity (Se) aSpecificity (Sp) |
| Does the patient have free fluid in the abdominal cavity? |
√Yes or no |
√Use AFAST‐applied fluid scoring system (1–4) |
Se – HighSp – High |
| Does the patient have free fluid in the retroperitoneal space? |
√Yes or no |
√Trivial, mild, moderate, severe |
Se – High to variableSp – High |
| Does the patient have any obvious AFAST target organ abnormalities? |
√Yes or no |
√ |
Se – Variable, operator dependentSp – High |
| Does the patient have pleural effusion? |
√Yes or no |
√Trivial, mild, moderate, severe via its DH view |
Se – HighSp – High |
| Does the patient have pericardial effusion? |
√Yes or no |
√Trivial (<0.5 cm), nild (>0.5 and <1.0 cm), moderate (>1.0 and <2 cm), severe (>2 cm) via its DH view (Candotti and Arntfield 2015) |
Se – HighSp – High |
| Does the patient have lung pathology along the pulmonary–diaphragmatic interface? |
√Yes or no |
√Vet BLUE B‐line scoringVet BLUE 6 lung ultrasound signs (Lisciandro 2014b,c; Lisciandro and Fosgate 2017) |
Se – Unknown, operator dependentSp – Likely high |
| What is the patient's volume status? |
√Unremarkable or abnormal |
√Characterizing the dynamic changes in height of caudal vena cava (bounce, fluid responsive; FAT, fluid intolerant; or flat, hypovolemic) (see Figures 36.7, 36.10–36.12); coupled with hepatic venous characterization (presence or absence of the “tree trunk sign” – see Figure 36.8); and absolute maximum CVC height measurements (see Table 36.3) |
aHypervolemia Se – Likely high Sp – Likely high aHypovolemia Se – Likely variable Sp – Likely high aEuvolemia Se – Variable Sp ‐ Variable aIntegrating TFAST echo and Vet BLUE pulmonary information likely improves both Se and Sp |
| What is the patient's urine production? |
|
√Length (cm) × width (cm) × height (cm) × 0.625 = volume estimation (mL) |
Unknown |
aClinical experience, limited veterinary studies, human studies.
having a fluid scoring system
looking cranial to the diaphragm into the thorax at the DH view for pleural and pericardial effusion and lung conditions
examining the gallbladder wall for signs of intramural edema
characterizing the caudal vena cava and its associated hepatic venous system
observing the urinary bladder for its expected rounded contour and measuring it (when applicable) for bladder volume estimation and urine output
calculating the AFS to better make sense of the volume of blood in hemorrhaging small animals
serving as monitoring tool for any and all effusive conditions
taking advantage of its target organ approach.
In other words, an AFAST not only provides a highly sensitive and specific means to detect intraabdominal and retroperitoneal effusions, but also serves as an abdominal soft tissue screening test for obvious target organ pathology. Patient information is acquired rapidly during AFAST (<3–4 minutes) with low patient impact (minimal restraint, no shaving) and point of care (Lisciandro et al. 2009; Lisciandro 2012, 2016a; Boysen and Lisciandro 2013; McMurray et al. 2016).
Abbreviations and terminology are listed in Table 6.4.
POCUS abdominal, thoracic, ocular, neurological, and musculoskeletal examinations are more extensively described in their respective chapters; however, the POCUS approach should always include minimally an AFAST, with its target organ approach, and AFS, and, much better, the Global FAST approach, as an extension of your physical exam for best practice. Global FAST has been advocated by the author as an extension of the physical examination for virtually any small animal patient since 2005 (Lisciandro 2011, 2012, 2014a–c, 2016a,b; Lisciandro et al. 2019), with a similar approach more recently advocated in human medicine (Lichtenstein 2010; Narasimhan et al. 2016).
Can detect free fluid in small amounts superior to physical examination and abdominal radiography and comparable to the gold standard of computed tomography (CT).
Can detect clinically significant pleural and pericardial effusions in most cases by imaging past or cranial to the diaphragm at the AFAST DH view.
Can detect retroperitoneal effusion when imaging at the AFAST spleno‐renal (SR) and hepato‐renal (HR) views and the HR5th and SR5th bonus views.
Can anticipate degree of anemia in different patient subsets by using its easily applied abdominal fluid scoring system.
Can be used to screen for canine anaphylaxis through the detection of sonographic striation of the gallbladder wall as the “double rim effect” or “halo effect” or “halo sign” at the AFAST DH view, referred to as the “anaphylactic gallbladder,” coupled with the finding of a flat caudal vena cava (CVC) (see Figure 36.9).
Can be used to screen for right‐sided congestive heart failure through the detection of sonographic striation of the gallbladder wall as the “double rim effect” or “halo effect” or “halo sign” at the AFAST DH view, referred to as the “cardiac gallbladder,” coupled with the finding of a FAT CVC (see Figure 36.7).
Can be used to assess volume status and right‐sided cardiac function by evaluating CVC size and for the presence of hepatic venous distension, the “tree trunk sign,” at the AFAST DH view (see Figure 36.8).
Can screen for concurrent target organ injury or pathology for basic soft tissue conditions of the liver, gallbladder, kidneys, urinary bladder, spleen, and gastrointestinal tract.
Can assess urinary bladder integrity at the AFAST cysto‐colic (CC) view especially when there are concerns regarding rupture in trauma cases.
Can noninvasively estimate urinary bladder volume and thus urine output at the AFAST CC view using the formula of length (L) × width (W) × height (H) (cm) × 0.625 = estimation of urinary bladder volume (mL) (Lisciandro and Fosgate 2017).
Cannot sonographically characterize fluid, thus sample acquisition via abdominocentesis is required when fluid is safely accessible; and fluid analysis should be performed.
In penetrating trauma, AFAST lacks sensitivity (in contrast to blunt trauma where it has high sensitivity) but likely is highly specific for intraabdominal and retroperitoneal injury similar to human studies (Udobi et al. 2001).
In penetrating trauma, AFAST should always be repeated post resuscitation as long as necessary until assured that the patient is not a surgical candidate by repeating at 2–4 hours post admission as standard of care and then continued at eight hours, 12 hours, 24 hours, two days, three days, five days, etc. post trauma at any time the patient is not doing well, for example to detect a septic abdomen or pyothorax that would otherwise be missed. Table 6.4. Abbreviations and terminology. As lengthy as the list seems, the abbreviations and terminology allow for more rapid communication verbally and in medical records.Source: Reproduced with permission of Dr Gregory Lisciandro, Hill Country Veterinary Specialists, FASTVet.com, Spicewood, TX.Terminology for standardized ultrasound examsAbdominal FASTAFASTThoracic FASTTFASTVeterinary Bedside Lung Ultrasound ExamVet BLUEGlobal FASTAFAST, TFAST and Vet BLUE combined as a single ultrasound examinationComplete Detailed Abdominal UltrasoundComplete Detailed EchocardiographySerial ExaminationRepeating the standardized protocol and recording your findings. Serial examinations have also been referred to as “secondary examinations.” We prefer the term “serial” (Blackbourne et al. 2004; Lisciandro et al. 2009)Ultrasound signs and characterizations used during AFASTAFAST views:DH view = diaphragmatico‐hepatic viewSR view = spleno‐renal viewHR view = hepato‐renal viewCC view = cysto‐colic viewHRU view = hepato‐renal umbilical viewSRU view = spleno‐renal umbilical viewHR5th bonus view = the final view of small animals when in right lateral recumbency imaging the right kidney and adjacent right liver (not part of the abdominal fluid scoring system)SR5th bonus view = the final view of small animals when in left lateral recumbency imaging the left kidney and adjacent spleen (not part of the abdominal fluid scoring system)CC pouch = most gravity‐dependent region where free fluid would accumulate at the CC viewHRU (SRU) pouch = most gravity‐dependent region where free fluid would accumulate at the HRU (SRU) viewPouch = most gravity‐dependent region at that acoustic windowGallbladder “halo sign,” also called “halo effect,” “double rim effect”Occurs with the presence of intramural gallbladder edema, recognized as sonographic striation, and supports the diagnosis of canine anaphylaxis (along with acute collapse and gastrointestinal signs and a flat CVC) versus right‐sided heart failure/generalized systolic dysfunction, pericardial effusion (along with a FAT CVC) versus right‐sided volume overload (FAT CVC) in collapsed, weak, hypotensive dogs (see Figures 36.7 and 36.9). There are other causes for gallbladder wall edema (see Table 7.5and Chapter 8), however, canine anaphylaxis and heart conditions present more emergently with acute weakness or collapse in a previously healthy dog (Lisciandro 2014a)Caudal vena cava (CVC) characterization by assessing maximum heights in the longitudinal orientation at the FAST DH viewBounce: expected ~35–50% dynamic respirophasic changes in CVC height during the respiratory cycle; also called a “fluid‐responsive CVC”; an expected maximum height in longitudinal at the DH view is available for dogs of various weights and cats (see Tables 7.6and 36.3 and Figures 36.9–36.12).Flat: lacks respirophasic dynamic change (<10%) in CVC maximum height and having an abnormally small maximum height; also called “hypovolemic CVC” or “fluid starved CVC”; maximum heights of <0.25 cm, <0.35 cm, <0.50 cm for dogs weighing <9 kg, >9 kg, <15 kg and >15 kg, respectively (modified by Lisciandro from Darnis et al. 2018).FAT: lacks respirophasic dynamic change (<10%) in CVC diameter during inspiration and expiration having an abnormally large maximum height (Ferrada et al. 2012a,b); also called a “fluid‐intolerant CVC”; maximum heights of >1.0 cm and >1.5 cm for dogs weighing <9 kg and >9 kg, respectively (modified by Lisciandro from Darnis et al. 2018).Cardiac bumpObservation at the FAST DH view where the muscular apex of the heart is beating and often indenting along the diaphragm; helps rule in and rule out pericardial effusion through presence or absence of the “racetrack sign” (Lisciandro 2014a,b, 2016a) (see Figures 7.13, 7.14and 39.5)Racetrack signSign indicative of pericardial effusion at the FAST DH view through the observation of free fluid rounding the apex of the heart being contained within the pericardial sac (Lisciandro 2014a,b, 2016a) (see Figure 7.13)Tree trunk signObservation of distended hepatic veins as they drain into a distended (FAT) caudal vena cava (abnormal finding); represents conditions impeding blood flow from the liver to the right heart, most commonly right‐sided failure, pericardial effusion, and dilated cardiomyopathy (DCM), and right‐sided volume overload during fluid resuscitation (Lisciandro 2014a,b; Nelson et al. 2010) (see Figure 36.8)Urinary bladder volume estimation formula (mL)Length (cm) × width (cm) × height (cm) × 0.625 (Lisciandro and Fosgate 2017)
Читать дальше