Evolution of Platelet Concentrates
Contributors
Richard J. Miron
Chapter Highlights
Evolution of PRF and the reasons for its discovery
Discussion of PRP vs PRGF vs PRF vs L-PRF, A-PRF, etc
Biologic background of key steps involved during wound healing

 Video 1-1
Video 1-1
Platelet concentrates were derived more than 20 years ago following the discovery that platelets themselves act as key regulators during the wound healing process. Initial attempts were first made to concentrate these cells using anticoagulants and a centrifugation device; the resulting biomaterial was called platelet-rich plasma (PRP). Shortly thereafter, protocols were developed with the aim of avoiding the use of anticoagulants altogether, because clotting is a pivotal step during the wound healing cascade; the resulting biomaterial was called platelet-rich fibrin (PRF). Today, platelet concentrates have become incredibly relevant worldwide, with their use spanning across nearly every field of regenerative medicine. Furthermore, one of the main growth factors (GFs) found in platelets—platelet-derived growth factor (PDGF)—has been commercialized as a ready-made laboratory recombinant protein under the trade name GEM 21S (Lynch Biologics). Thus, as medicine has continued to evolve and progress, an obvious and clear trend favoring GF use has been established. Furthermore, by modifying centrifugation devices and spin protocols of PRP/PRF, a greater ability to concentrate not only platelets but also leukocytes became possible, further favoring tissue regeneration. This chapter takes a deep look at the years of research leading to the significant advancement that has been made in this field. The evolution from PRP to PRF, including pioneering concepts such as the low-speed centrifugation concept and horizontal centrifugation, are discussed in terms of their ability to favor higher cell content, GF concentration, and ultimately better wound healing.
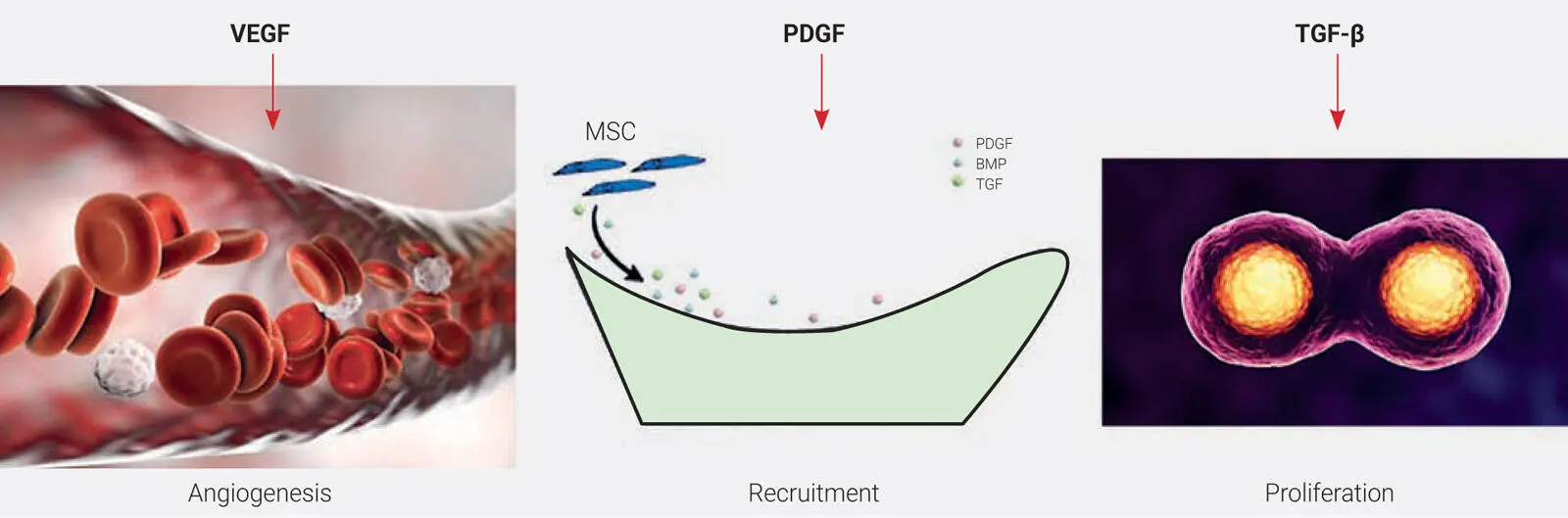
Platelet concentrates have been utilized in medicine for over two decades because of their ability to rapidly secrete autologous GFs and ultimately speed wound healing. They have gained tremendous momentum as a regenerative agent derived from autologous sources capable of stimulating tissue regeneration in a number of medical fields. 1,2Many years ago, it was proposed that by concentrating platelets using a centrifugation device, GFs derived from blood could be collected from a platelet-rich plasma layer and later utilized in surgical sites to promote local wound healing. 1,2Today, it has been well established that platelet concentrates act as a potent mitogen capable of the following ( Fig 1-1):
Speeding the revascularization of tissues (angiogenesis)
Recruiting various cells including stem cells
Inducing the prompt multiplication of various cell types found in the human body (proliferation)
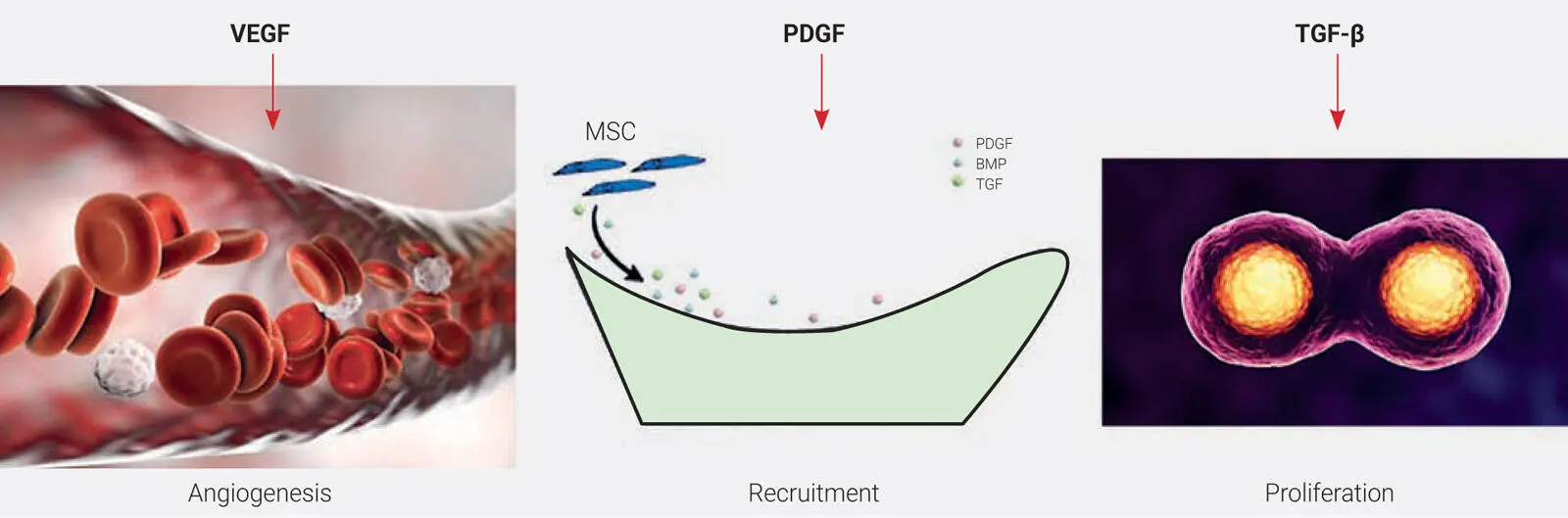
Fig 1-1The three main GFs that are released from PRF include VEGF, a known inducer of angiogenesis; PDGF, a known inducer of cell recruitment; and TGF-β1, a known stimulator of cell proliferation. MSC, mesenchymal stem cell.
Wound healing is a complex biologic process whereby many cell types interact with one another as well as their local extracellular matrix (ECM) in order to repair and regenerate damaged tissues. 3–6While many regenerative agents currently exist on the market to help speed tissue regeneration, it is important to note that the majority are derived from other human sources (allografts) and animal byproducts. These naturally create a foreign body reaction when implanted into host tissues. While the majority of such biomaterials do certainly favor improved healing, it has generally been recognized and accepted that the gold standard for the majority of tissue-regenerative procedures in basically every field of medicine has been the use of autogenous tissues.
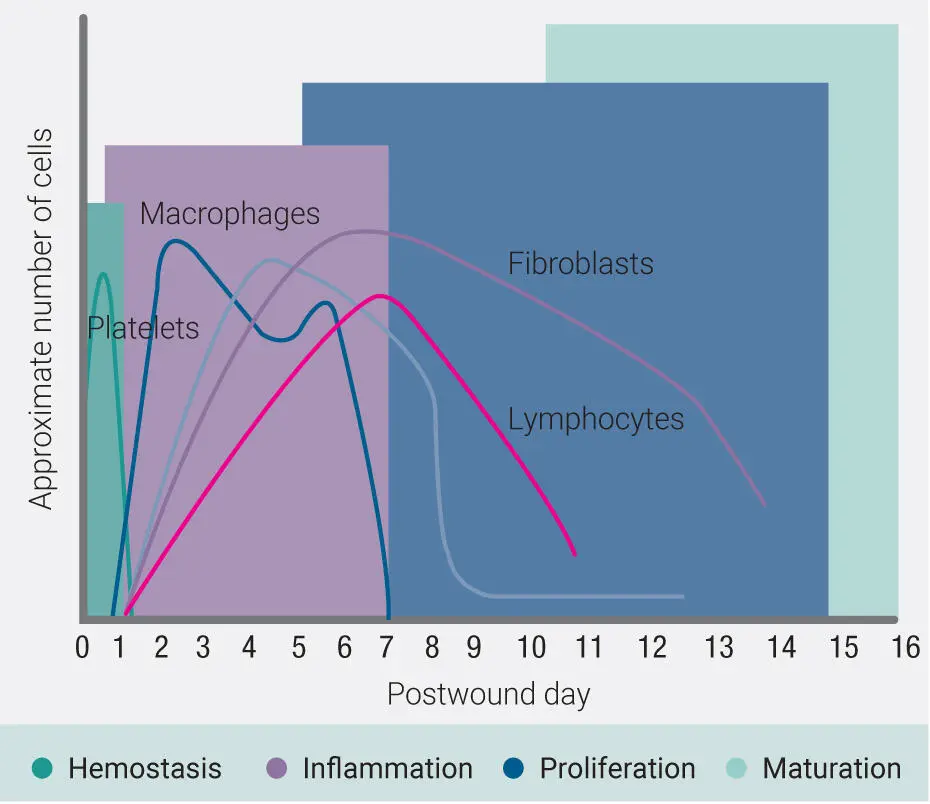
Specifically in dentistry, platelet concentrates were introduced over 20 years ago by Robert E. Marx and colleagues with the aim of concentrating blood proteins as a natural source of GFs that would stimulate vascularization (angiogenesis) and tissue ingrowth based on the fact that blood supply is pivotal for tissue regeneration of all tissues. 7Wound healing has been described as a four-step process that includes (1) hemostasis, (2) inflammation, (3) proliferation, and (4) maturation 8–10( Fig 1-2). Each phase overlaps one another and encompasses various microenvironments, including different cell types that assist in wound healing. Noteworthy are the implications of immune cells during biomaterial integration. In a study titled “OsteoMacs: Key players around bone biomaterials,” osteal macrophages were discussed as being key and pivotal cells during the wound healing process. 11Thus, as tissue biology has continued to evolve, platelet concentrates have also seen significant advancement with respect to their ability to favor healing by incorporating immune cells (leukocytes). Various systematic reviews from multiple fields of medicine have now demonstrated their ability to support tissue regeneration across many tissue types and cell types. This chapter reviews the evolution of platelet concentrates.
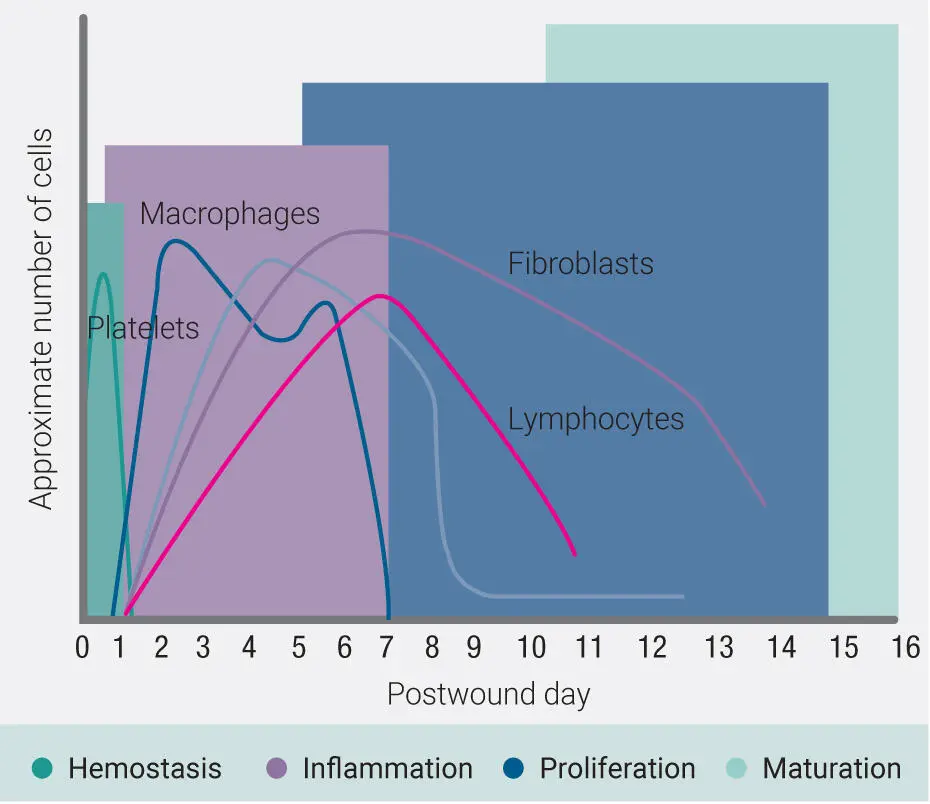
Fig 1-2Four phases of wound healing: (1) hemostasis, (2) inflammation, (3) proliferation, and (4) maturation. Noteworthy are the overlaps between each of the phases and the population of cells found in each category. Whereas lymphocytes typically arise at 7 days, the ability of PRF to introduce a high number at day 0 acts to speed the regenerative phase during this process.
PRP (1990s)
The use of platelet concentrates has slowly and gradually gained popularity over time, with a dramatic increase being observed in the past 5 to 10 years. This parallels precisely the massive increase in research articles being published on the topic. Despite this, it is important to review and highlight the pioneering work conducted by Marx and colleagues over 20 years ago, without which none of this textbook would exist. 12–14
Platelet-rich plasma (PRP), as its name implies, was designed to accumulate platelets in supraphysiologic doses within the plasma layer following centrifugation. The main aim of PRP was to isolate and further concentrate the highest quantity of platelets and their associated GFs for regenerative purposes, thereafter reimplanting this specialized supraconcentrate at sites of local injury. This concept has been the basis of thousands of research articles, with their protocols being utilized to favor wound healing in millions of patients.
Initial protocols typically ranged in duration from 30 minutes to 1 hour based on the centrifugation/collection systems and protocols utilized. The original concept was pioneered by Harvest Technology, where it was shown that over 95% platelet concentration could be accumulated, having the potential to help favor the regenerative phase of many cell types including soft tissues, epithelial cells, periodontal ligament cells, and bone cells. 15,16Because these initial protocols were lengthy, anticoagulants were added to the blood collection tubes. These typically were various forms of concentrated bovine thrombin or sodium citrate.
Читать дальше

 Video 1-1
Video 1-1