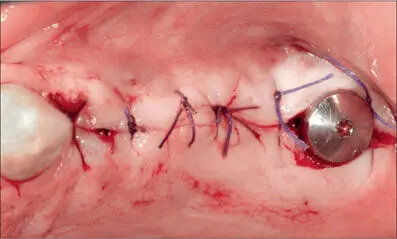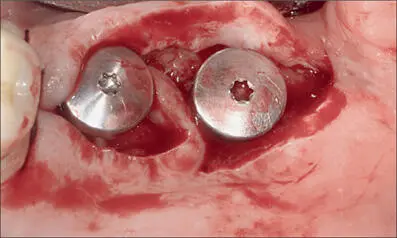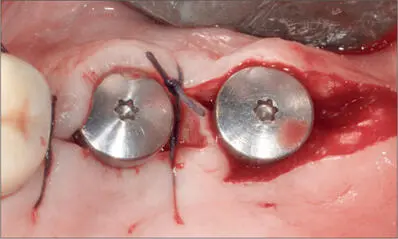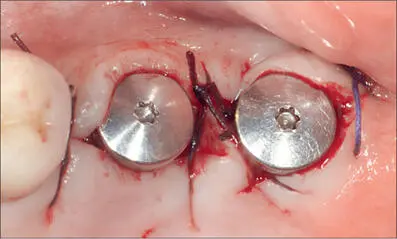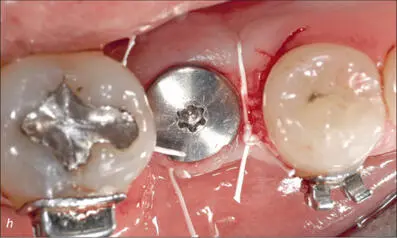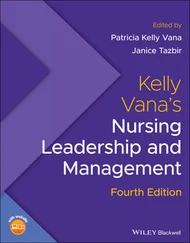
Fig 4h Semi-submerged healing in the anterior grafted area; non-submerged healing with close adaptation of the flap around the collar of the distal implant.

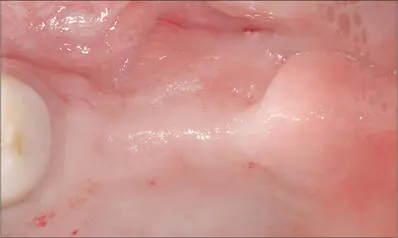
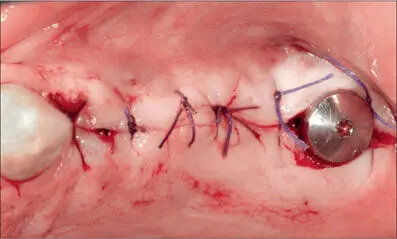
Fig 4i Optimal adaptation of the soft tissues around both implants six weeks after implant placement.

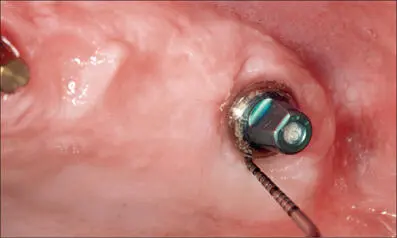
Fig 4j Solid abutments, 4 mm in height, connected eight weeks after implant placement.

Fig 4k Four-unit cemented metal-ceramic bridge in situ.
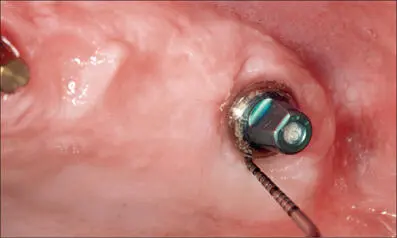
Fig 4l One-year follow up. Healthy peri-implant soft tissues with minimal probing depth (< 4 mm) and no bleeding after removing the provisionally cemented ceramic bridge.
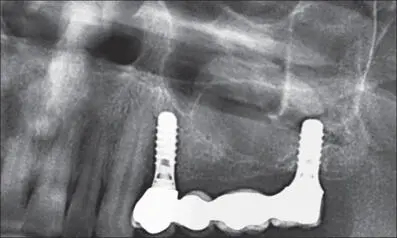
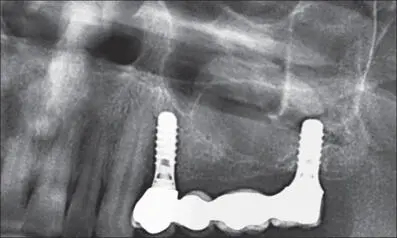
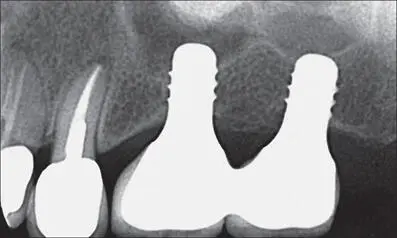
Fig 4m Radiograph at the five-year follow-up. Stable interproximal bone levels.
One of the challenges in optimal flap design around non-submerged implants is the circumferential closure around the implant collar, especially when the soft tissues present anatomical irregularities. Figures 5a-kshow an example of soft-tissue management for non-submerged tissue-level implants in the posterior maxilla with an irregular soft-tissue morphology.

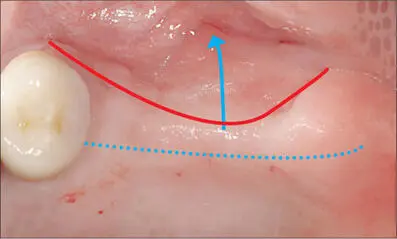
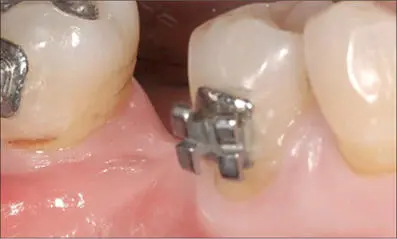
Fig 5a Preoperative situation.
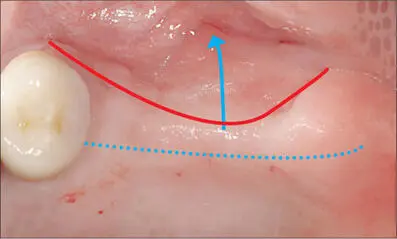
Fig 5b Incision placed slightly palatally to move keratinized tissue onto the buccal side.
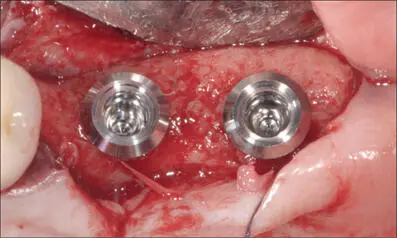
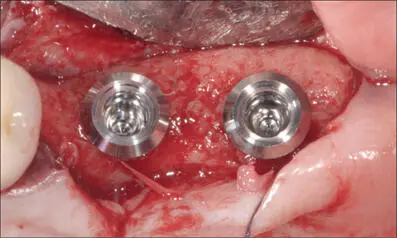
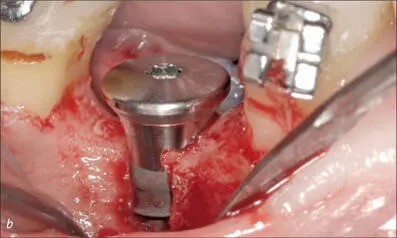
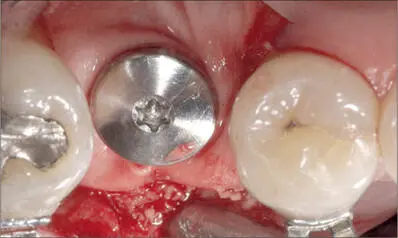
Fig 5c Two wide-neck implants placed at sites 26 and 27 (SP, WNI SLActive, diameter 4.8 mm, length 10 mm; Institut Straumann AG).
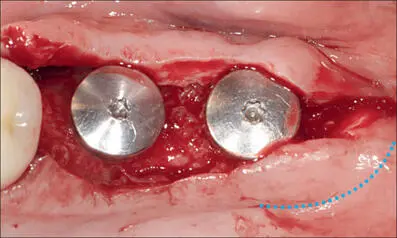
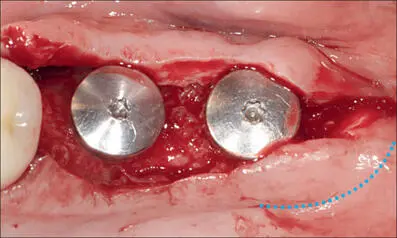
Fig 5d Incision on the distal portion of the palatal flap.
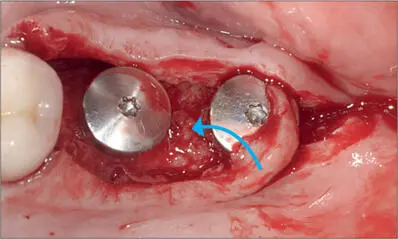
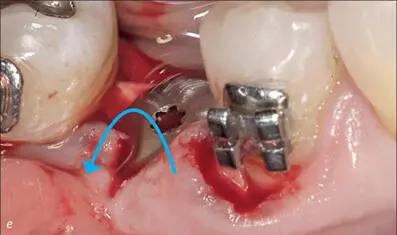
Fig 5e The pedicle flap was rotated counterclockwise.
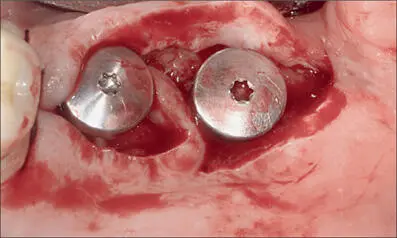
Fig 5f Pedicle inserted between the two implants.
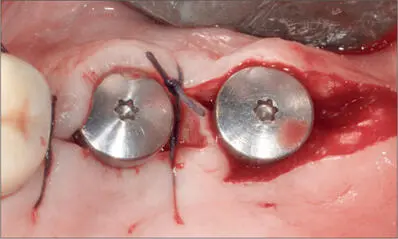
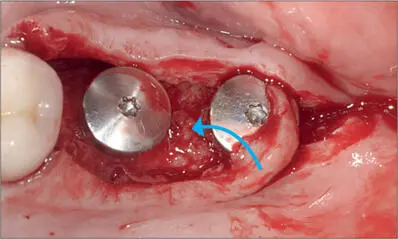
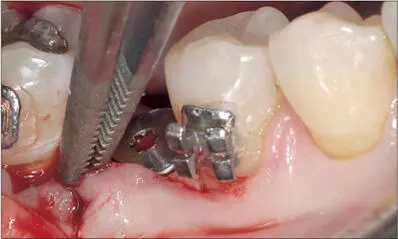
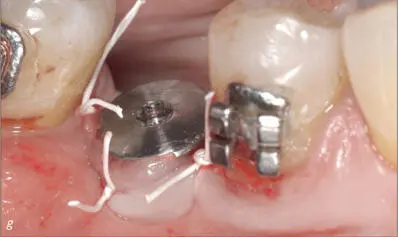
Fig 5g The pedicle was adapted with a 4-0 Vicryl vertical mattress suture between the 2 implants.
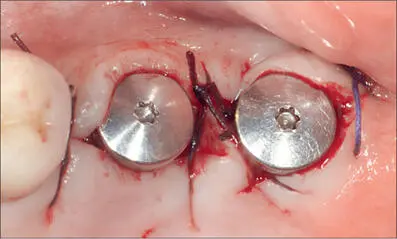
Fig 5h Final suture, distally to the distal implant.
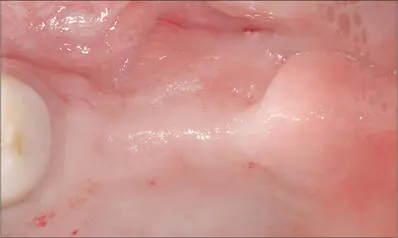
Fig 5i Preoperative occlusal view.

Fig 5j Postoperative occlusal view.
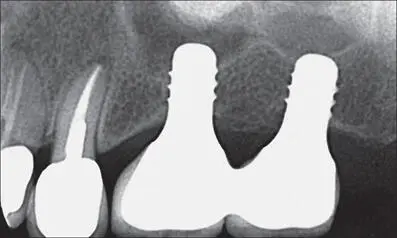
Fig 5k Periapical radiograph at eighteen months after implant placement. Favorable interproximal bone levels.
Creating an optimal flap for ideal transmucosal healing becomes even more difficult if no keratinized mucosa is present at all. In these circumstances, a free gingival graft may be advised, especially if bone regeneration is required, as discussed in Chapter 4.1.
Often, a small quantity of keratinized tissue will be sufficient to create a soft-tissue cuff around the implant collar, provided the tissue is properly surgically managed. Figures 6a- Ishow an example of soft-tissue management around a tissue-level implant in conjunction with bone regeneration in a case where there does not appear to be any keratinized tissue available.
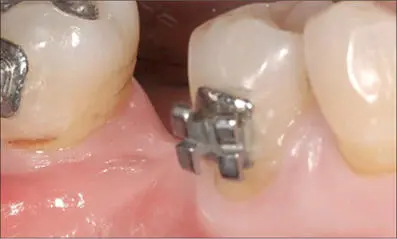
Fig 6a Preoperative view of site 46, at the end of orthodontic treatment. Limited crestal width and no keratinized mucosa.
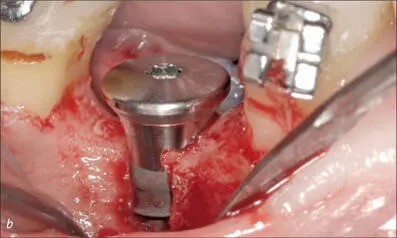
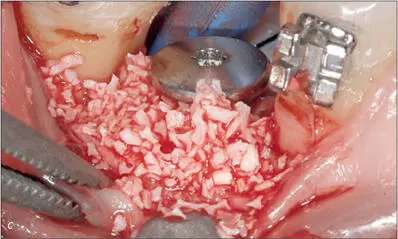
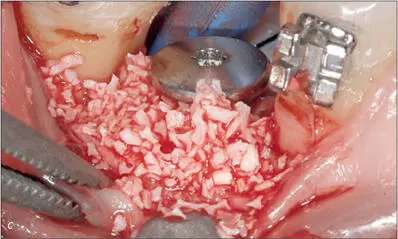
Fig 6b-c Once the implant was placed (S, SLA, diameter 4.1 mm, length 12 mm; Institut Straumann AG), the dehiscence on the facial bone was covered with autologous bone and a DBBM graft.
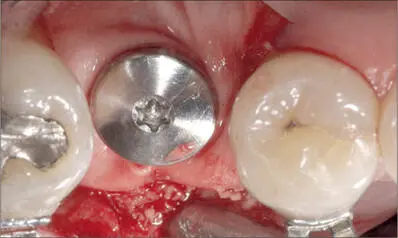
Fig 6d Resorbable collagen membrane prepared with a punched hole, placed over the graft, and secured with a healing cap.
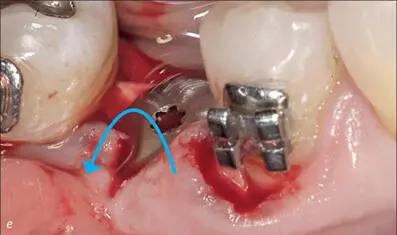
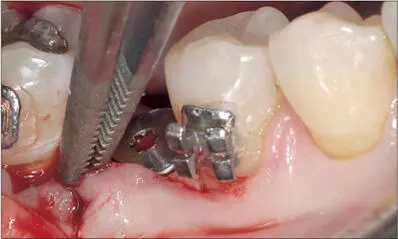
Fig 6e-f The mesial papilla rotated 90° counterclockwise and sutured to the distal papilla to provide a wide band of keratinized tissue buccally to the implant.
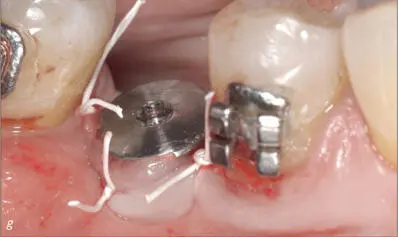
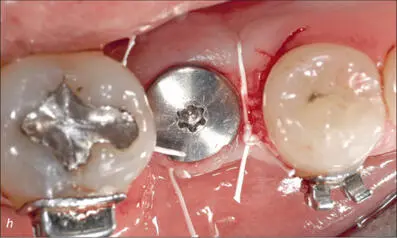
Fig 6g-h e-PTFE sutures, buccal and occlusal views.
Читать дальше