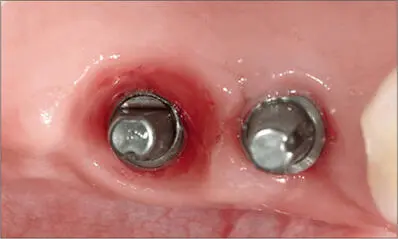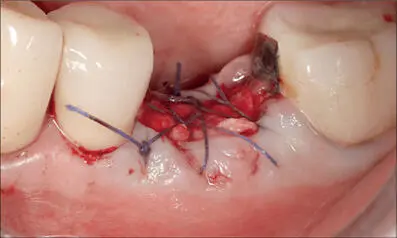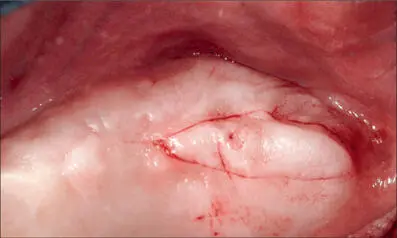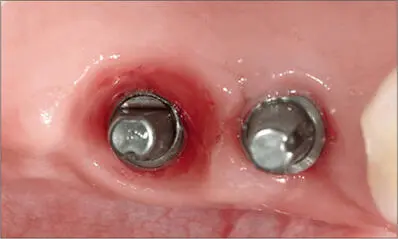
Fig 2a The distal implant was placed at the level of the bone crest without considering the thickness of the soft tissue, resulting in a deep mucosal tunnel.

Fig 2b Residual resin-based cement around the distal Wide Neck Implant. The deep mucosal tunnel does not allow complete removal of the excess cement. Screw-retained restorations would have been preferable in both cases.
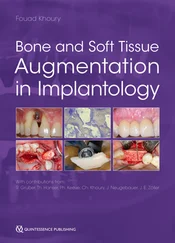
The ideal implant position for optimal soft-tissue integration should be planned before removing the teeth. Ridge preservation is one of the treatment options after tooth extraction, particularly in situations where one or more socket walls are missing (Roccuzzo and coworkers 2014c; Mardas and coworkers 2015). The rationale for this approach is that the maintenance of the ridge contour often facilitates subsequent treatment steps and limits the risk of an improper position of the implant collar, creating an ideal soft-tissue seal (MacBeth and coworkers 2017). Figures 3a-ishow an example of long-term soft-tissue stability after implant placement following ridge preservation. The correct positioning of an implant, with a shallow peri-implant sulcus, could be particularly difficult in areas where the mucosa is too thick. Here an appropriate flap design is mandatory, especially if cemented restorations are planned. Figures 4a-hshow an example of implant positioning in the posterior maxilla where a tissue excess needed to be removed.
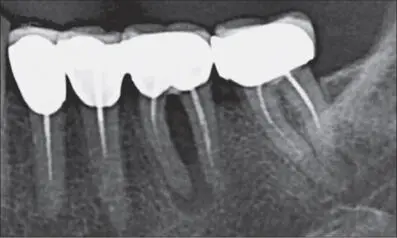
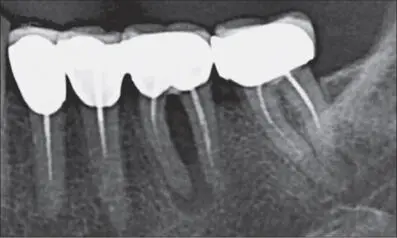
Fig 3a Radiograph of a first molar with a severe endo-perio lesion. A large post-extraction bone defect with reduced bone levels near the adjacent teeth was anticipated, and therefore ridge preservation was planned.
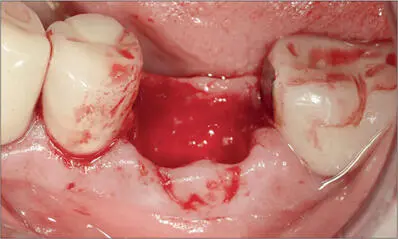
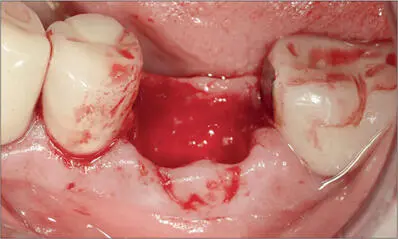
Fig 3b After tooth extraction and careful removal of inflamed epithelium around the socket border, the marginal mucosa appeared mobile due to the lack of buccal bone.
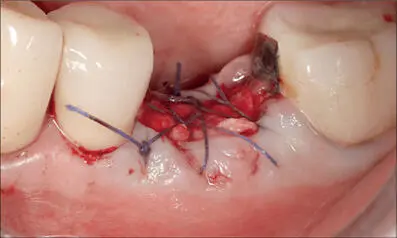
Fig 3c Deproteinized bovine bone mineral (DBBM) with 10% collagen (Bio-Oss Collagen; Geistlich, Wolhusen, Switzerland) was inserted to fill the decontaminated socket and covered with a double layer of collagen membrane (Bio-Gide; Geistlich) secured with 4-0 Vicryl (Ethicon; Johnson & Johnson International) resorbable sutures.

Fig 3d After eight weeks of healing, a thick band of keratinized mucosa was visible.

Fig 3e After four months, the dimensions of the ridge were adequate to insert a fixture in the proper position, with no need for further augmentation.
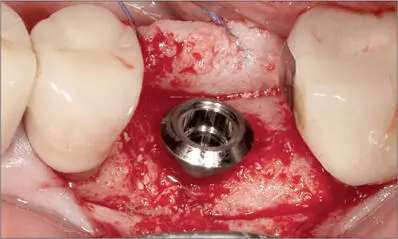
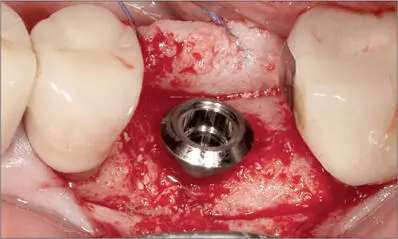
Fig 3f A chemically modified titanium implant was placed (S, WNI SLActive, diameter 4.8 mm, length 12 mm; Institut Straumann AG, Basel, Switzerland).
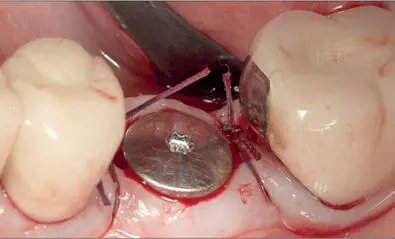
Fig 3g The soft tissues were circumferentially adapted around the smooth collar of the implant for ideal non- submerged suturing.
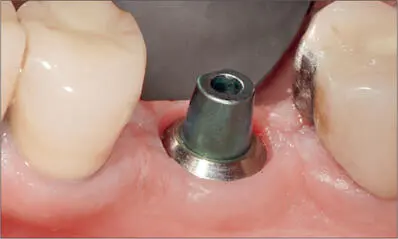
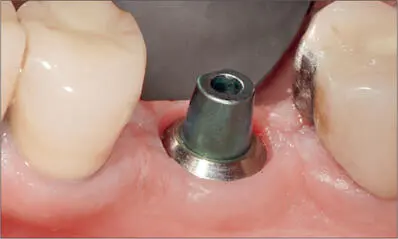
Fig 3h Three months after placement, the implant was surrounded by a firm collar of keratinized tissue.

Fig 3i Good stability of the peri-implant soft tissues seven years after placement despite some buccal recession on the adjacent natural premolar.

Fig 4a Part of a panoramic radiograph. Large cyst in the maxillary left sinus. After consultation with an ENT surgeon, who did not suggest any specific treatment, it was decided to place implants without interfering with the sinus.

Fig 4b The left posterior maxilla. The probe used for bone sounding indicated the presence of very thick mucosa in the area of the second molar.
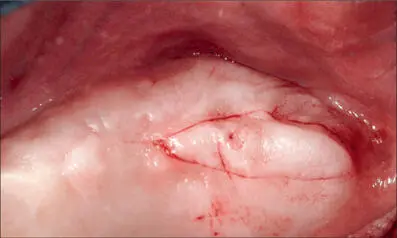
Fig 4c Primary incision lines.

Fig 4d Left posterior maxilla after removal of the excess tissue, which was later used as a graft in the anterior area.
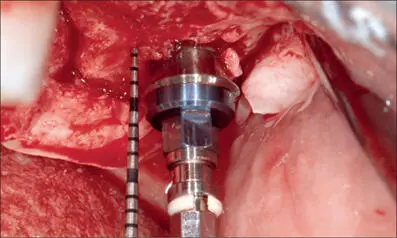
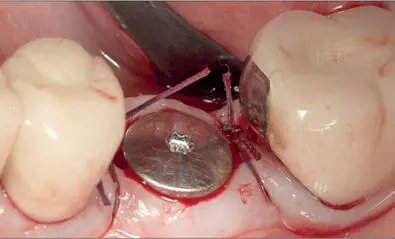
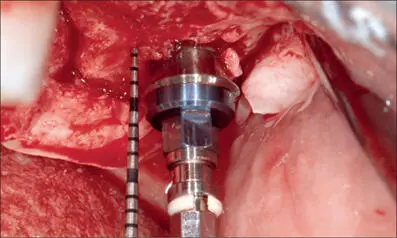
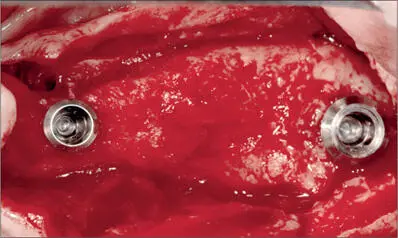
Fig 4e Titanium implant at site 27 with a chemically modified surface (S, WNI SLActive, diameter 4.8 mm, length 10 mm; Institut Straumann AG). The standard implant with a 2.8-mm smooth collar was considered ideal for bringing the margin of the restoration to a more coronal level.
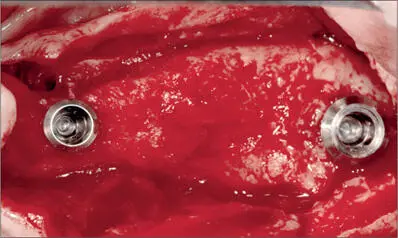
Fig 4f Intraoperative view following the placement of implant 24 (SP, WNI SLActive, diameter 4.1 mm, length 12 mm; Institut Straumann AG). The implant with a 1.8-mm collar was selected to reduce the risk of future soft-tissue dehiscences. The bone concavity on the buccal aspect of the mesial implant is a risk factor for dehiscence.
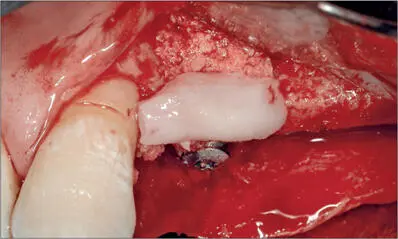
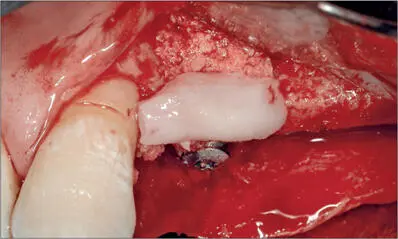
Fig 4g Autologous bone chips on the buccal aspect of the implant. The connective-tissue graft taken from the posterior area was adapted to protect the bone chips and to increase the width of the crest.
Читать дальше