Clinical and Endoscopic Characteristics
Typically, there is a temporal relationship between the onset of symptoms and ingestion of a potentially injurious drug. Common symptoms include sudden‐onset chest pain, odynophagia and/or dysphagia that occur within a few hours or days after taking the medication. Severe reflux injury is often an initial diagnostic concern. The chest pain may be pleuritic in nature, mimicking a pulmonary embolism, or may suggest an acute cardiac syndrome. Hematemesis and perforation are rare complications.
Table 2.7 Medications implicated in causing esophagitis and histologic features.
| Medication |
Histologic features |
| NSAIDs |
Nonspecific, ± crystalline debris |
| Antibiotics (e.g. tetracyclines/doxycycline, clindamycin) |
Doxycycline—vascular injury |
| Potassium chloride |
Nonspecific |
| Iron |
Bluish‐brown crystalline debris, Fe stain + |
| Bisphosphonates (e.g. alendronate) |
Nonspecific, ± crystalline debris and multinucleated squamous cells |
| Quinidine |
Nonspecific |
| Resins (e.g. kayexalate, bile acid sequestrants) |
Kayexalate: Basophilic crystals with “fish scales,” AFB (black), PAD, Diff‐quick bile acid sequestrants:Orange‐black crystals, lack “fish scales,” AFB (yellow) |
| Mycophenolate |
Increased apoptosis (GVHD‐like) |
| Taxanes |
Mitotic arrest, ring mitoses |
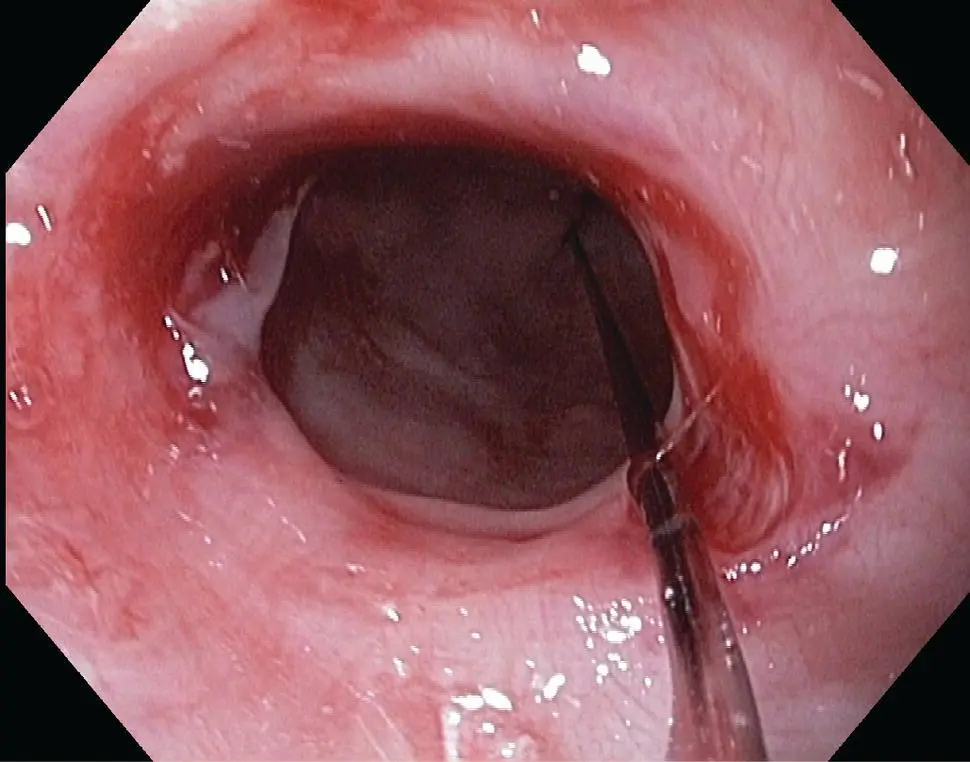
Endoscopically, most lesions occur in the middle third of the esophagus, at the level of the aortic arch, although any level may be involved. Findings include erythema, erosions, ulcers (including “kissing” ulcers), and strictures. Discrete erosions in this region, away from the Z‐line, are an important clue suggesting a drug‐related etiology ( Figure 2.15). Occasionally, a diffuse mucosal sloughing pattern has been described.
Microscopic Features ( Table 2.7)
Biopsies most commonly show nonspecific esophagitis characterized by erosions, ulcers, active inflammation with neutrophils and occasionally eosinophils, surface epithelial damage, and granulation tissue. Adjacent mucosa is relatively normal. A careful search of the exudate and ulcer bed for refractile or polarizable foreign material is warranted, which may be an important diagnostic clue. However, in most cases the clinical history is necessary to make the diagnosis.
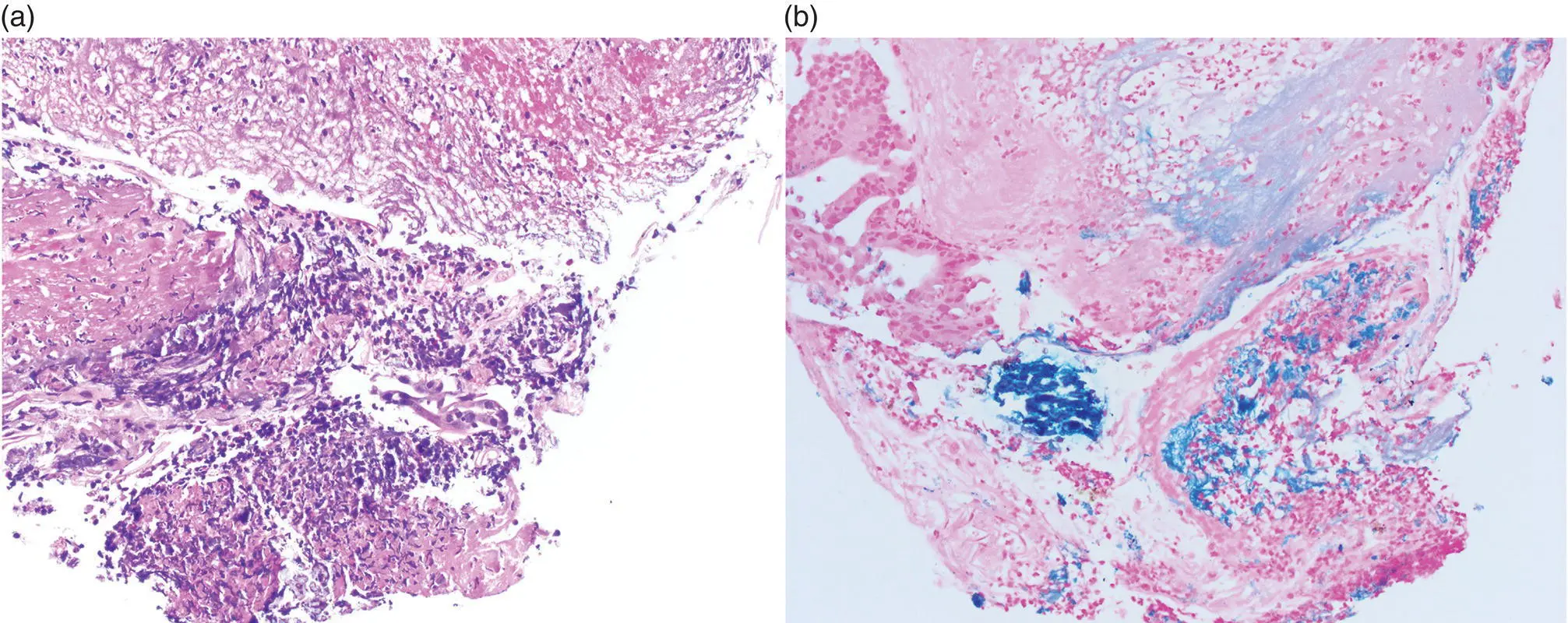
Some medications are associated with additional characteristic histologic features. Erosions and ulcers associated with doxycycline injury often exhibit a distinct capillary/vascular injury with degenerative changes and possible fibrin thrombi. In iron pill‐associated mucosal injury, bluish‐brown crystalline iron debris is found adjacent to the surface epithelium, admixed with the inflammatory exudate, or within granulation tissue ( Figure 2.16). The iron can be highlighted by a Prussian Blue stain, which may also demonstrate crystalline debris in the lamina propria or underlying vessels. Although iron is well recognized as a caustic agent in the esophagus and elsewhere in the GI tract, some cases may represent secondary deposition in preexisting lesions. Alendronate has been associated with multinucleated squamous cells, in addition to the presence of polarizable crystalline material.
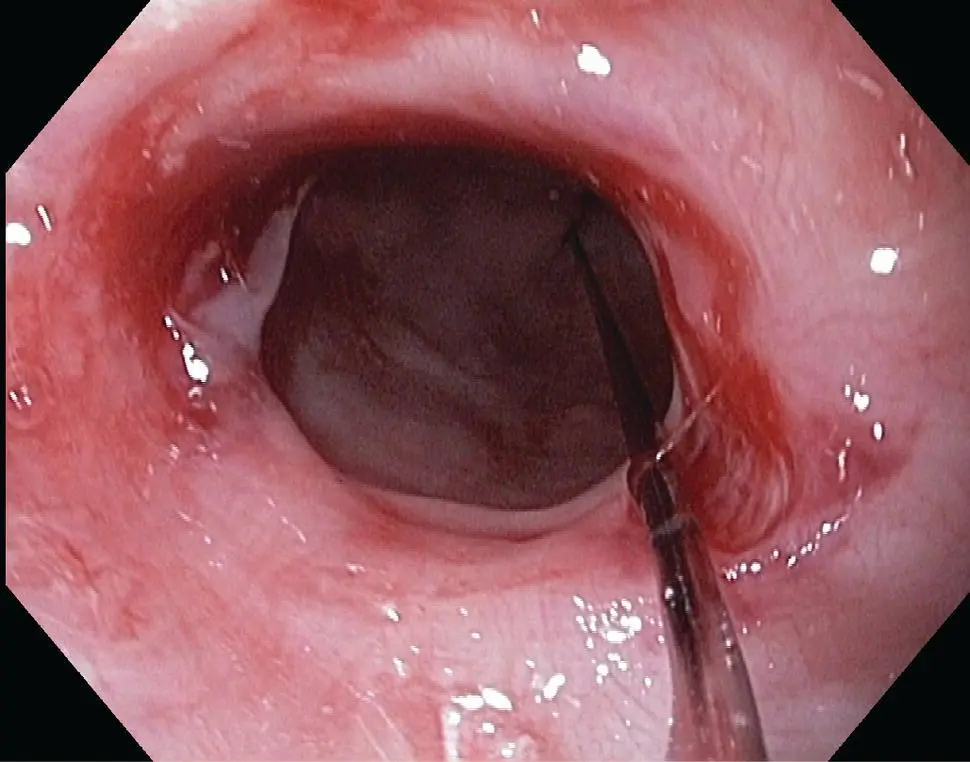
Figure 2.15 Endoscopic appearance of inflammatory stricture of the esophagus with sloughing mucosa.
Kayexalate (sodium polystyrene sulfonate) in sorbitol can be recognized by the presence of characteristic lightly basophilic, refractile, nonpolarizable crystals that display a mosaic pattern that resembles fish scales. The crystals can be highlighted by acid fast (black), PAS/Alcian blue and Diff‐Quik stains. Bile acid sequestrants (e.g. colestipol, colesevelam, cholestyramine) may be recognized by their orange‐black crystals, which lack a striated, fish‐scale appearance and may appear pale yellow on acid fast stain.
Mycophenolate, used in solid organ transplantation, is associated with increased apoptosis of esophageal squamous epithelial cells, resembling GVHD. Taxane‐based chemotherapy leads to striking mitotic arrest with ring mitoses, along with epithelial necrosis or ulceration.
The major histologic differential diagnostic consideration is infection, particularly fungal ( Candida ) or viral (HSV, CMV), which may need to be excluded with appropriate histochemical and immunohistochemical stains or recognized by characteristic viral cytopathic effect. In rare cases, exuberant granulation tissue and excessive exudates mimic the gross appearance of a neoplasm. If eosinophils are prominent, reflux or eosinophilic esophagitis may enter into the differential diagnosis. GVHD should be excluded if prominent apoptosis is present, such as with mycophenolate injury. Finally, lichen planus involvement of the proximal esophagus with stricture formation can also mimic drug injury. In all of these considerations, the clinical context is critical to the evaluation of the histopathologic findings.
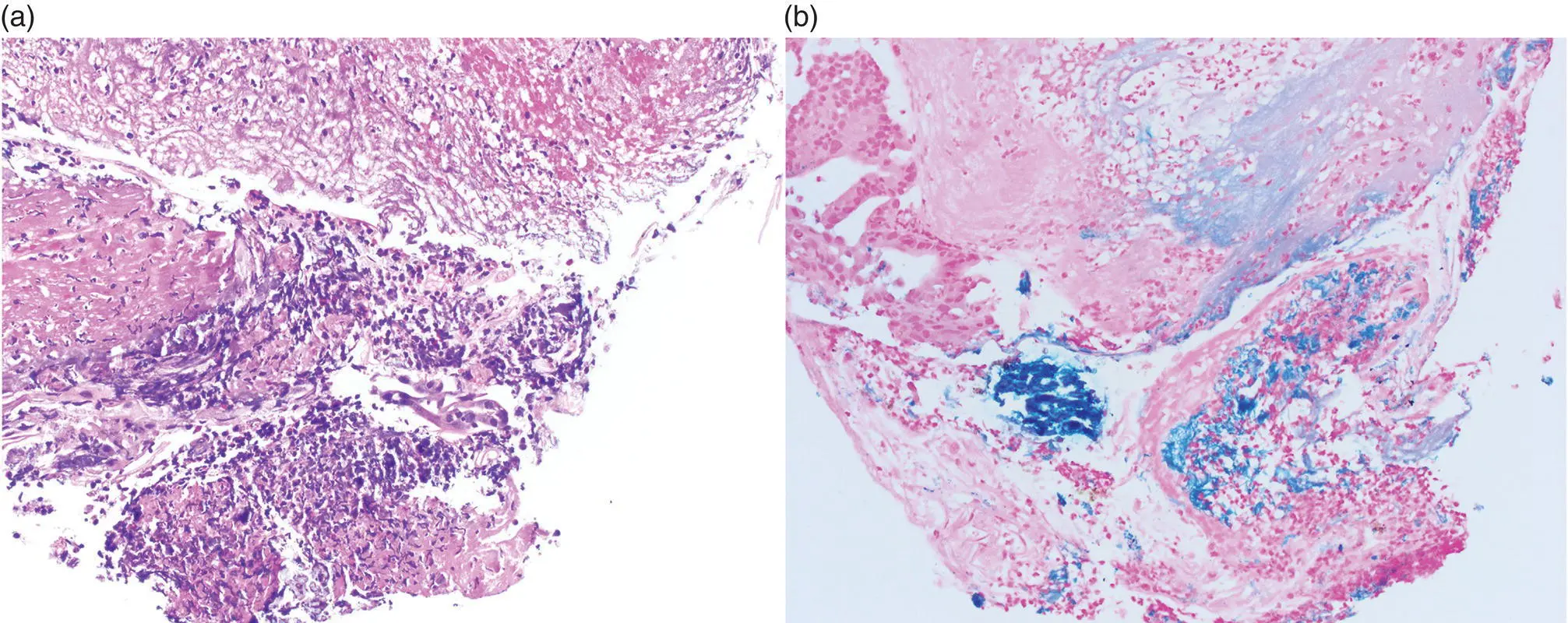
Figure 2.16 (a) Iron tablet erosive esophagitis with fibrinopurulent debris. (b) The Prussian Blue iron stain is diagnostic.
Prognosis, Evolution and Clinical Management
Most cases are self‐limited and resolve without complications. Discontinuing the suspected caustic agent and supportive management, such as PPI therapy, hydration, sucralfate, or topical anesthetics, typically results in an uneventful recovery. Local epinephrine may be needed for active bleeding. Dilatation may be required if strictures develop, and surgical management is rarely needed for severe complications such as perforation. Most patients can resume their medications with recommendations for proper administration, which will assist in avoiding recurrent injury.
Sloughing Esophagitis
Definition, General Features, Predisposing Factors
Sloughing esophagitis is characterized by extensive superficial squamous mucosal necrosis or desquamation, associated with endoscopic plaques imparting a sloughing appearance to the mucosa. Sloughing esophagitis has also been included under the terms esophagitis dissecans superficialis and acute necrotizing esophagitis, which includes broader inclusion criteria and more diverse causes of esophageal injury. It occurs in middle‐aged to older adults (median age 56 years), frequently with debilitating comorbidities and who are commonly on multiple medications, especially central nervous system depressants and drugs known to cause esophageal mucosal injury. It most likely represents a form of direct contact injury, rather than an ischemic injury, and may represent a unique pattern of drug‐induced esophagitis. Acute necrotizing esophagitis (“black esophagus”) is a rare condition that arises in debilitated patients with severe comorbidities such as hypoperfusion, sepsis, diabetic ketoacidosis, and malignancy, and results from the combining effect of ischemia and corrosive injury of gastric contents. A rare case occurring in a child who was associated with a history of vomiting has also been reported.
Clinical and Endoscopic Characteristics
Dysphagia, odynophagia, chest pain, heartburn, vomiting or cough are reported in 45% of patients, include. The mid‐distal esophagus is most commonly involved. Endoscopy reveals white plaques or membranes, and there may be sloughing of the epithelium as well as other nonspecific findings such as erythema, erosions, rings, or webs. In black esophagus, the sloughing necrotic membrane may appear blackened ( Figure 2.17). The clinical presentation is distinctive with bleeding and a characteristic diffuse circumferential black mucosal discoloration of the distal esophagus with an abrupt transition at the gastroesophageal junction.
Читать дальше