The presence of granulomas is helpful in diagnosing esophageal involvement by Crohn’s disease, but they are uncommon. Eosinophils may also be admixed with neutrophils and lymphocytes, and involvement of other parts of the GI tract is typically present.
Infections are recognized by the identification of viral inclusions (such as HSV), and fungal or parasitic organisms. Mixed inflammation with neutrophils may also be present. Rare cases of HSV esophagitis occurring in a background of EOE have been described.
Table 2.4 Endoscopic and histologic features of the major causes of infectious esophagitis.
| Organism |
Endoscopic features |
Morphological features |
Ancillary studies |
| Candida |
Focal or confluent white plaques |
Parakeratosis with neutrophils Colonization of ulcers Budding yeast, pseudohyphae, occasional septate hyphae Superficial invasion typical |
PAS‐diastase, GMS stains |
| Herpes simplex |
Superficial ulcers, multiple |
Edge of ulcer—inclusions in squamous cells and/or squamous debris of ulcer slough Multinucleation, ground glass nuclei, dense eosinophilic nuclear inclusions (Cowdry type A) |
IHC |
| CMV |
Single deep ulcer, linear ulcers |
Base of ulcer—inclusions in endothelial and stromal cells Intranuclear (“owl's eye”) and granular cytoplasmic inclusions Atypical inclusions common |
IHC |
Table 2.5 Conditions associated with esophageal eosinophilia in the differential diagnosis of EOE.
| GERD |
| PPI‐responsive esophageal eosinophilia |
| Eosinophilic gastrointestinal diseases |
| Crohn's disease |
| Infection ( Candida , HSV, parasites) |
| Hypereosinophilic syndrome |
| Achalasia |
| Drug hypersensitivity injury |
| Vasculitis |
| Pemphigus |
| Connective tissue diseases |
| Graft versus host disease (GVHD) |
In drug‐induced esophageal eosinophilia, there is a temporal relationship and resolution when the offending agent is withdrawn.
Ancillary Studies (if Applicable)
IHC for virus (HSV) and/or special stains for fungi (GMS, PAS‐diastase) are indicated if infection is suspected.
Prognosis, Evolution, and Clinical Management
EOE is initially treated with proton pump inhibitors. There is emerging evidence that PPIs affect specific inhibition of the chemokine, eotaxin, which blunts eosinophil infiltration. It may be difficult to distinguish GERD‐associated eosinophilia from EOE in this subgroup. For those that do not respond to PPI, options include identification and avoidance of food antigens (typically through a Six Food Elimination Diet; SFED) or suppression with topical corticosteroids, which can be from a swallowed metered dose inhaler, or from peroral viscous budesonide. For late‐stage, fibrotic disease, repeated, carefully monitored esophageal dilation is effective.
Lymphocytic Esophagitis
Definition, General Features, Predisposing Factors
This uncommon and poorly characterized condition is histologically defined as the presence of dense lymphocytic infiltrates involving the esophageal mucosa without concomitant evidence of significant active inflammation. It is described in approximately 1/1000 esophageal biopsies, predominantly affecting older females (median age 63 years). This controversial entity lacks clearly defined clinical associations in adults, and likely represents a nonspecific reaction pattern to a wide variety of mucosal insults ( Table 2.6), including GERD, medications, infection, motility disorders, and other immune‐mediated disorders. In the pediatric population, lymphocytic esophagitis has been described in association with Crohn’s disease and celiac disease.
Clinical and Endoscopic Characteristics
About 75% of patients present with esophageal symptoms, most commonly dysphagia or odynophagia, which may raise the suspicion of eosinophilic esophagitis. Similarly, the endoscopic impression may suggest eosinophilic esophagitis, with the presence of rings, furrows, plaques, and strictures.
Table 2.6 Conditions associated with esophageal lymphocytosis (lymphocytic esophagitis).
| GERD |
| Medications |
| Infection |
| Motility disorders |
| Immune‐mediated disorders (e.g. CVID) |
| Lichen planus/lichenoid esophagitis |
| Crohn's disease (pediatric) |
| Celiac disease (pediatric) |
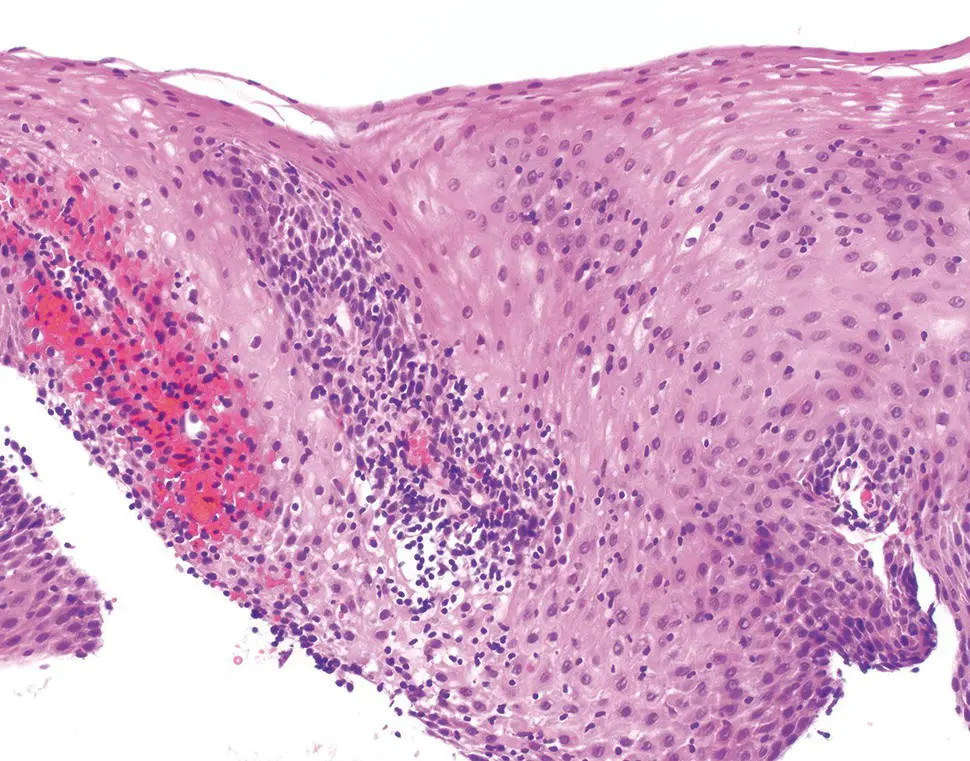
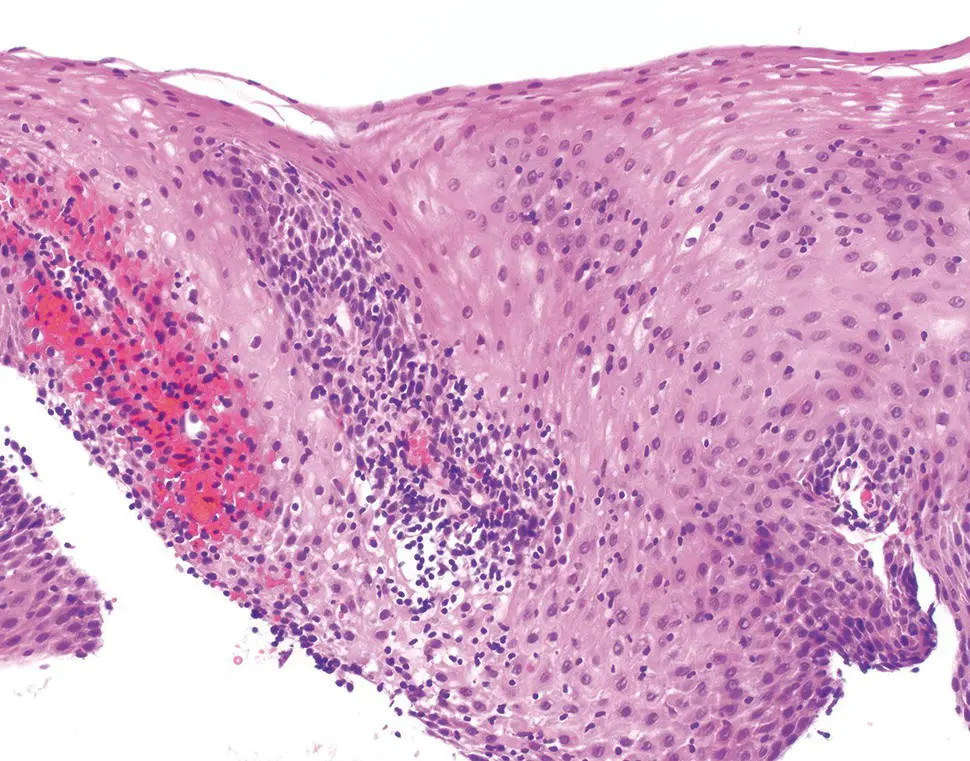
Figure 2.14 Characteristic histology of lymphocytic esophagitis.
Recently proposed histologic criteria include the presence of dense lymphocytic infiltrates involving esophageal squamous mucosa with marked spongiosis in the absence of significant numbers of neutrophils or eosinophils ( Figure 2.14). The findings are most pronounced in the peripapillary epithelium. There is no required or established “minimum” count or density of intraepithelial lymphocytes, and the pattern and distribution of the lymphocytic epithelial injury is most important.
Immunohistochemical Studies and Molecular Features
Ancillary testing, including the subtyping of the intraepithelial CD3, CD4, and CD8 T cells is generally noncontributory and not required for the diagnosis. A subset of cases with CD4 predominant T cells and dysmotility has been reported.
The clinical and endoscopic differential diagnosis includes EOE, although by definition eosinophils are rare or absent. If neutrophils are present, special stains for candida may be warranted. Intraepithelial lymphocytes may be prominent in lichen planus esophagitis/lichenoid esophagitis, although the additional presence of a band‐like lymphocytic infiltrate in the lamina propria and necrotic keratinocytes is a distinguishing feature. Characteristic direct immunofluorescence findings of lichen planus DIF may or may not be demonstrated. Lymphocytosis may also be associated with esophageal involvement by Crohn’s disease in children, although other histologic and clinical features of Crohn’s disease are typically present, particularly elsewhere in the gut.
Follow‐up clinical and biopsy data are limited, although in some patients sequential biopsies have demonstrated persistent lymphocytosis, suggesting a chronic process.
Drug‐Induced Esophagitis
Definition, General Features, Predisposing Factors
Medication‐related injury to the esophageal mucosa (“pill esophagitis”) is an increasingly recognized complication of orally administered drugs. Mucosal injury is typically caused by prolonged direct contact and local caustic effects of the offending agent, although mechanisms of toxicity may be complex and multifactorial. Numerous drugs have been implicated ( Table 2.7). Most cause a nonspecific injury pattern, and the diagnosis is suggested by the clinical history.
Elderly patients and women are most commonly affected. The elderly often have multiple underlying risk factors, and the female predominance is attributed to the more common use of certain medications in this group, such as iron supplements and bisphosphonates. Risk factors include pills taken with little or no water or while recumbent, underlying disorders of esophageal motility (e.g. diabetes, strictures, achalasia) and disorders of local anatomy causing external compression (enlarged left atrium, aortic aneurism). However, many patients do not exhibit abnormal esophageal function or other risk factors.
Читать дальше