The correct matching of the .STL surface scan data with the CBCT data (as determined by gray-level differences) is crucial, as the accuracy of implant planning and placement depends on this step. Consequently, option 2 may be contraindicated in certain conditions. The presence of an insufficient number or distribution of remaining teeth or large metal or zirconia restorations in the arch to be treated can make it difficult to impossible to achieve accurate data matching 30. In these cases, option 1 (despite being more expensive) is the only way to proceed, hence, radiographic templates with reference structures have to be used during CBCT scanning. Once the clinician has gathered all the necessary information, the actual process of prosthetic-driven implant planning can begin. The cloud-based systems also have the advantage of enabling different colleagues to work on a case simultaneously, thus greatly simplifying coordination with the referring clinician. It is also possible to plan and save several versions without reimporting the data, which makes it possible to show different treatment options to the team and to the patient 16.
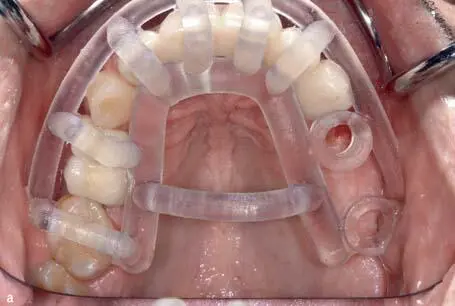
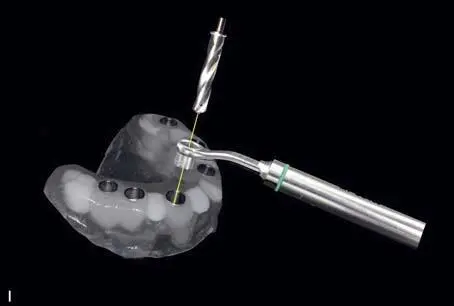
Once the final planning version has been approved, the drill guide can be fabricated directly in the dental laboratory or ordered from the service center (eg, SwissMeda, Baar, Switzerland). The splint module of the respective software package (SMOP, SwissMeda) used to design the drill guide also produces .STL datasets. With all systems currently on the market, the software contains details about all the relevant implant systems and the drill sleeves that go with them. The SMOP workflow in particular also an interesting feature: depending on which implant system is used, it may be possible to save the metal sleeve, which not only results in simplification of the manufacturing process and therefore savings, but also minimizes another source of error 31 , 32. Unfortunately, this software only supports the implant-planning program and cannot be used in the restorative treatment phase for virtual diagnostics or CAD of restorations. In other words, it cannot be used to plan temporary or final restoration superstructures (Fig 1-4-13).
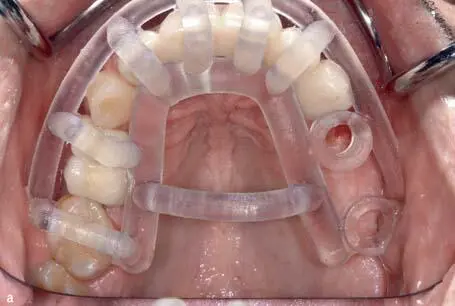
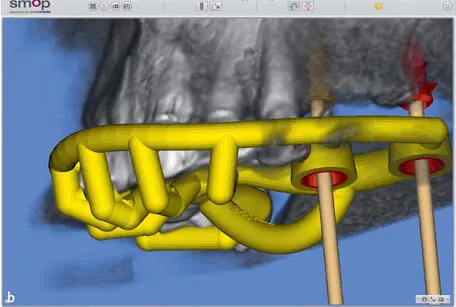

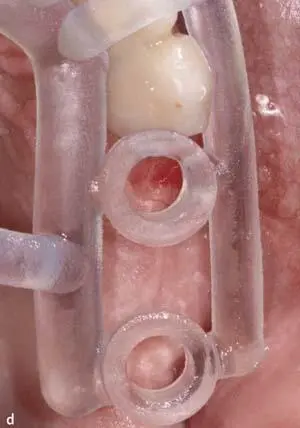
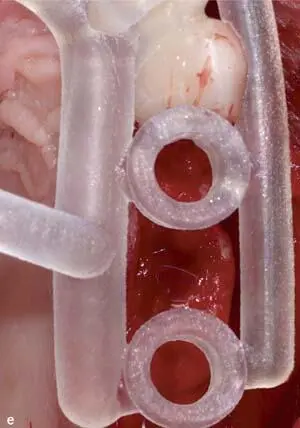
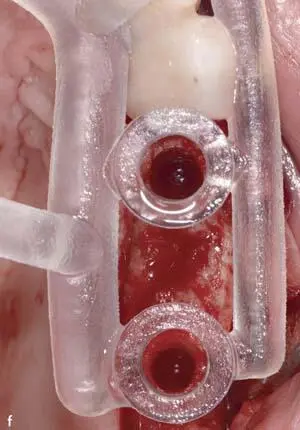
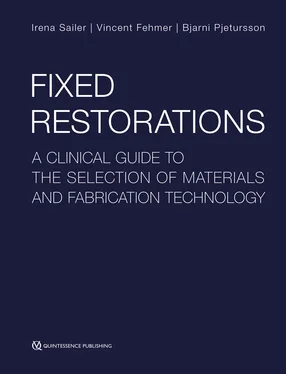
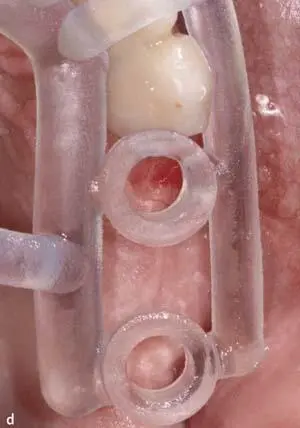
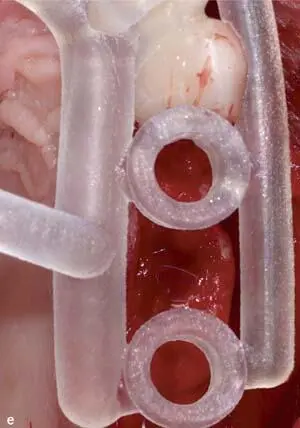
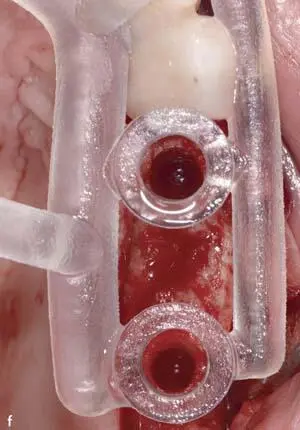
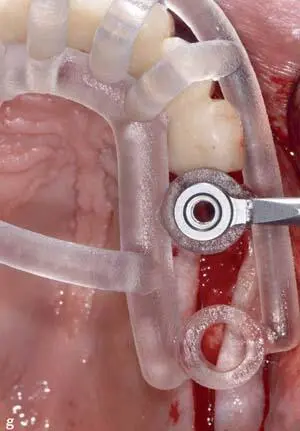
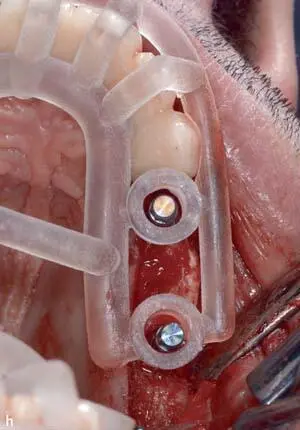
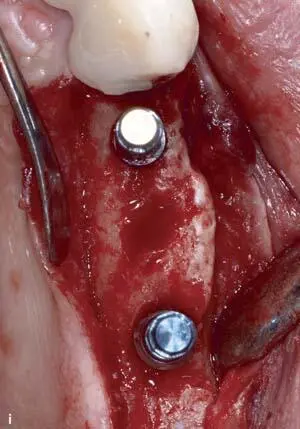
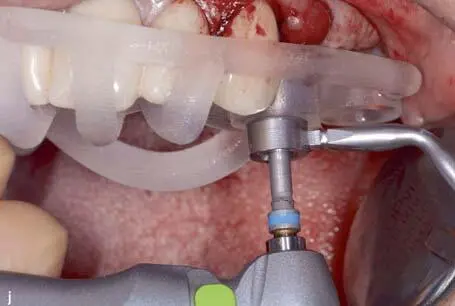
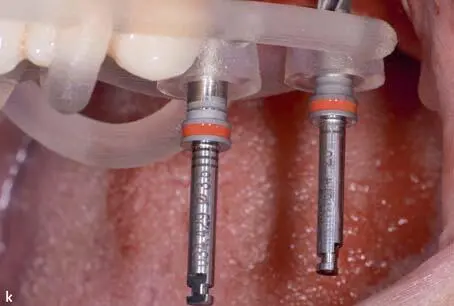
Figs 1-4-13 a to f 3D-printed surgical guide, based on guided surgery planning, transferring the relevant information of the virtually planned 3D implant position into the clinical situation. This specific guide (SMOP, Swissmeda) is an example of a digitally designed and printed surgical guide, allowing for excellent visibility of the surgical site, position accuracy, and enabling the surgeon to cool the surgical site during the implant bed preparation with sterile saline solution.
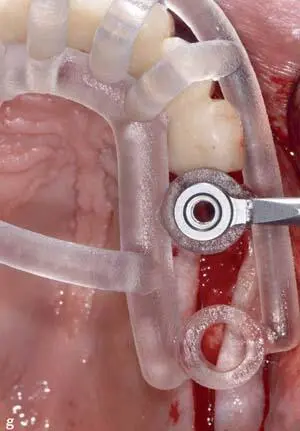
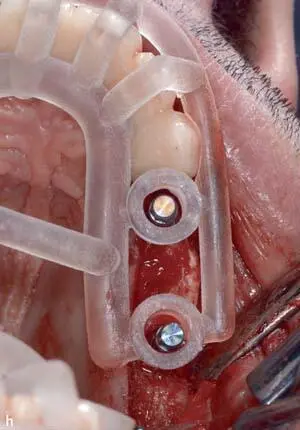
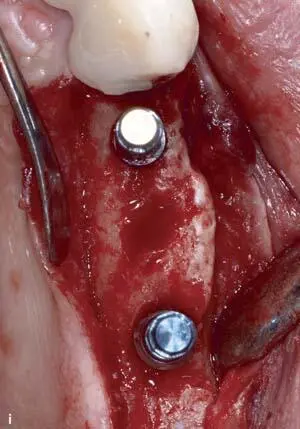
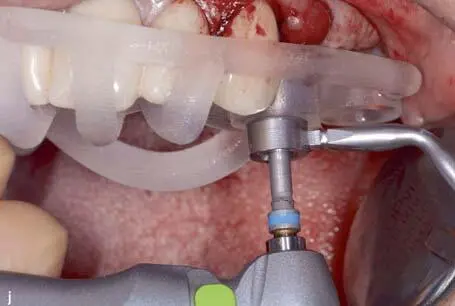
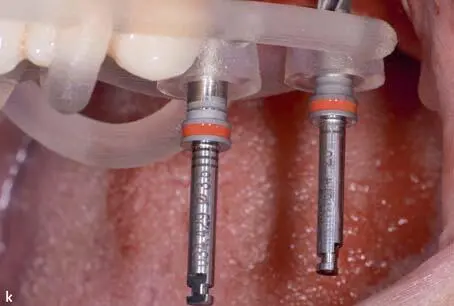
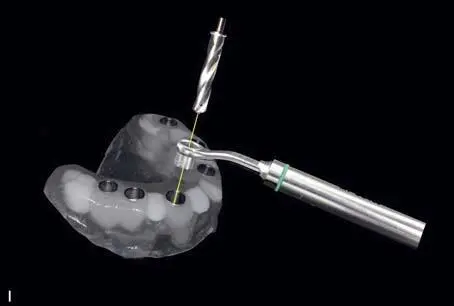

Figs 1-4-13 g to 1-4-13m 3D-printed surgical guide, based on guided surgery planning, transferring the relevant information of the virtually planned 3D implant position into the clinical situation. This specific guide (SMOP, Swissmeda) is an example of a digitally designed and printed surgical guide, allowing for excellent visibility of the surgical site, position accuracy, and enabling the surgeon to cool the surgical site during the implant bed preparation with sterile saline solution.
Creating a digital wax-up directly via the planning software
With this option, it is not only possible to upload and match the surface scan data of the current intraoral situation with the 3D CBCT data (as with options 1 and 2), but also to create a digital wax-up directly with the planning software. This workflow is highly efficient because the steps involved in displaying and then scaling and correctly positioning the virtual wax-up in the software can be completed very fast 33 , 34.
Most guided surgery systems today are intended for planning purposes only. They are equipped with rather rudimentary tooth libraries and design software tools that are, however, sufficient for single-tooth implant planning in situations with sufficient prosthetic references, like the adjacent teeth, albeit if used for cantilever and multispan fixed/removable dental prostheses restorations, proper adaptation and positioning of the virtual teeth can be very difficult.
There is great potential for the new generations of CAD/CAM software to fill this gap. Through the merging or modular docking of implant-planning software with the manufacturing software used in the dental laboratory, digital implant planning can now be performed in the virtual articulator with modern design tools, taking all the relevant information (such as the soft tissue margins) into consideration. The data can then be visualized in the implant-planning software in real time by creating a specific connection to the implant manufacturer (eg, Straumann DWOS Synergy Connection, Straumann, Basel, Switzerland). This allows the dental technician to continuously adapt the wax-up, and the clinician to change the implant position in the software module. After the implant-planning proposal has been finalized and approved, the dental technician designs the surgical guide using the software elements intended for dental laboratory use. The planned guide can be milled or 3D printed either in-house or by an external provider, which is sent to the corresponding datasets. This blending of software solutions also opens up new possibilities, eg, it is possible to design and manufacture temporary provisional restorations or abutments directly by utilizing the planned implant positions without having to laboriously export them from the planning software and then reimport them into the design software. In principle, the positioning of splints can be used to guide Part or all of the implant site preparation process. Some also allow for implant placement via the guide. Ultimately, it is up to surgeons to decide how much autonomous control they have over the entire process, ie, how much they want to rely on the planning software and surgical guide.
Читать дальше