The .STL file of the selected version was integrated into guided surgery software and the implants were planned in the correct prosthetically oriented 3D position. After implantation and tooth preparation, the same .STL file was used for the fabrication of the final tooth- and implant-supported restorations with aid of a CAD/CAM procedure. By copy-pasting one design into each treatment phase, the predictability of the treatment was improved, as well as the efficiency of the entire treatment process.
Digital technologies offer significant improvement opportunities in many dental and medical fields. Restorative dentistry has been one of the disciplines that has profited the most from these technological advancements 13. Among these innovations, CAD/CAM technologies have greatly influenced the production of provisional and definitive restorative components 9 , 12 , 13. As the technology establishes and further develops (intraoral optical scanners, cast optical scanners, virtual design software, 3D printers), new indications rise in other treatment phases of the restorative workflow.
Despite the initial economic investment needed to create a digital workflow (software, scanners, printers), the current technical limitations of these rather recent technologies, and the learning curve required to master the virtual tools this pathway offers, the dental digitalization is an unstoppable phenomenon that will surely push the dental standards even higher. The incorporation of these technologies into the prosthetic diagnostic phase improves patient–clinician–technician communication without significantly increasing the treatment costs. This improves the predictability of the treatment outcome, one aim that is crucial in contemporary restorative dentistry.
1.4.6 Augmented reality in dentistry
Augmented reality is a versatile new digital technology applied in dentistry for guided implant surgery, preoperative planning in maxillofacial surgery, in orthodontics, and in endodontology. Yet, most interestingly it has opened up new horizons in restorative dentistry 18.
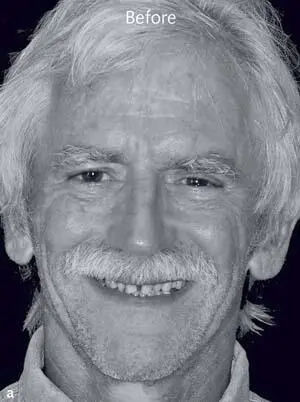
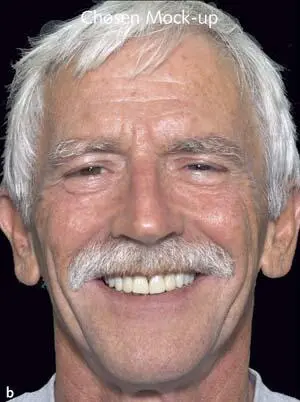
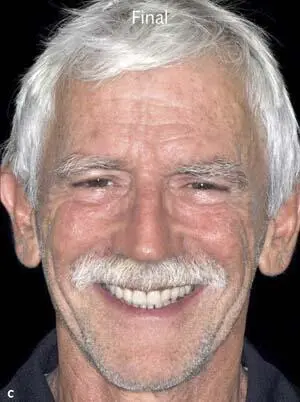
New augmented reality tools were introduced which allow for dynamic virtual diagnostics, before the treatment is even started. As an example, an augmented reality application was recently developed, and is now available for iPad or iPhone. This app acts as a virtual-mirror-like tool which helps patients to identify their treatment needs and desires for improvement at a very early stage (eg, Ivosmile, Ivoclar Vivadent, Liechtenstein). By this the communication with the restorative team is improved, and before investing time and money in elaborating the pretreatment diagnostics the first important desires can already be defined. The virtual mock-up is superimposed live on the patient’s face, while following all live movements of the lips, face, and head giving a natural appearance (Fig 1-4-8). The software automatically recognizes the correct position of the virtual teeth onto the natural teeth and within the face, without any need for reference points, which normally need to be defined for the super-imposition of 3D data and facial scans 19. The appearance is similar to looking into a mirror while changing different virtual mock-ups and thereby dental looks, and serves for communication and planning purposes.
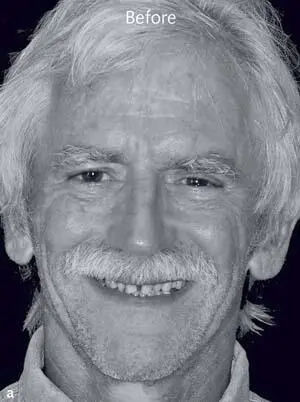
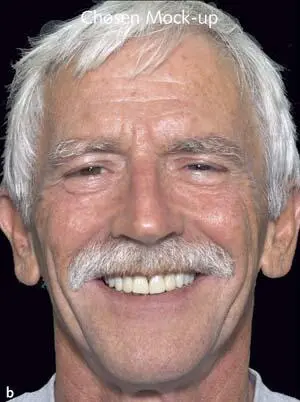
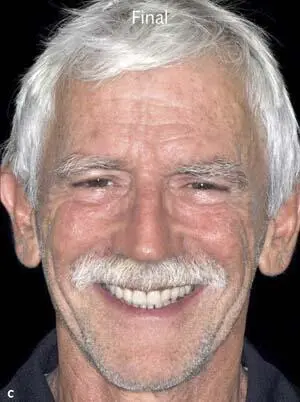
Figs 1-4-8a to 1-4-8c Before and after insertion of selected diagnostic mock-up (reproduced from Sancho-Puchades et al 16, with permission).





Figs 1-4-8d to 1-4-8h Situation before treatment, three different mock-ups, and final restoration (reproduced from Sancho-Puchades et al 16, with permission).
As indicated before, the presented app is using facial recognition (FR) and augmented reality (AR). FR describes a technology capable of automatically identifying a person from a digital image, using reference lines of the face and mathematical algorithms 20 , 21. AR is a type of technology in which an environment is enhanced through the process of superimposing computer-generated virtual content over a real structure 18 , 22. Even if AR tools were mainly used for video games and animations, the medical field is working to integrate these technologies for diagnosis, surgery, education, and communication with patients 23.
To date, this new technology serves for communication purposes only, yet, in the future its utility will certainly be expanded. As an example, the selected virtual solution may be exported from the app as an open .STL file, to be imported onto CAD or guided surgery software. The file may, hence, serve for the planning and execution of the respective treatment steps without further need of development of the virtual diagnostics by the dental technician. With this, time and efficiency may be increased, in line with the predictability of the treatment.
Furthermore, with aid of the exported selected virtual solution and its import into other digital files of the patients, eg, cone beam computed tomography (CBCT), the clinician can analyze whether or not anatomic limitations exist, and if pretreatment (eg, orthodontics) may be recommended in order to fulfill the patient expectations. The software may even be used to indicate solutions for compromise in such situations. As all these developments are just in their early days, they will need to further evolve in the years to follow.
Their current application is highlighted in Part II, Chapter 8 (Special indications) of this book.
1.4.7 Diagnostics for fixed implant-supported restorations, surgical stents
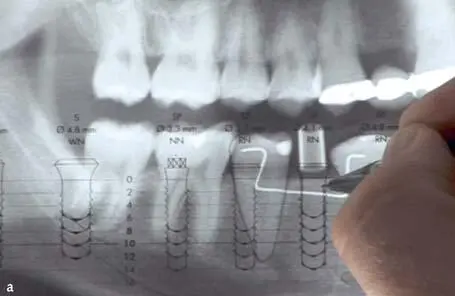
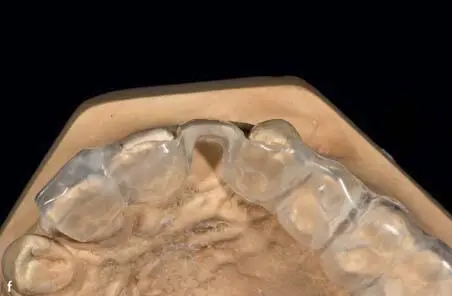
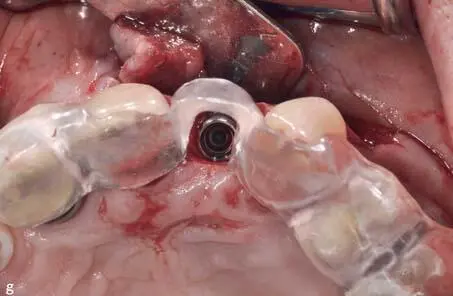
The 3D implant position is associated with the esthetic outcome of the implant-borne restorations and the associated soft tissue outcomes 24. In the past, the pretreatment diagnostics and planning of dental implants were mainly based on stone casts and 2D radiographs. Clinical structures such as the crowns of adjacent teeth, soft tissue margins, and tooth axes were used as orientation landmarks, and a template with composite resin simulating the future crown served as a drilling guide as well as a later means of assessing the 3D position of the implant. Radio-opaque templates made using radio-opaque composites allowed for the preliminary transfer of information from diagnostic radiographs (Fig 1-4-9).
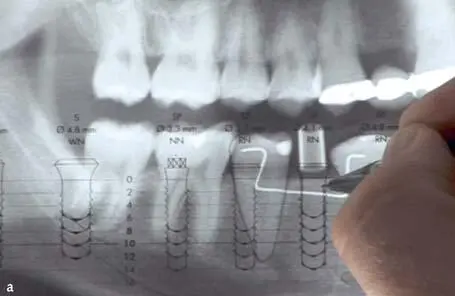




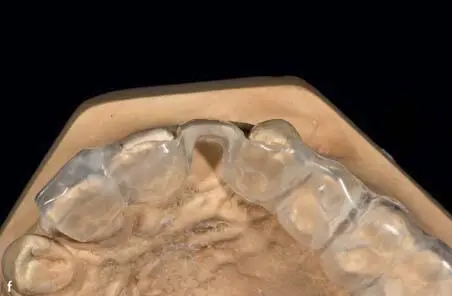
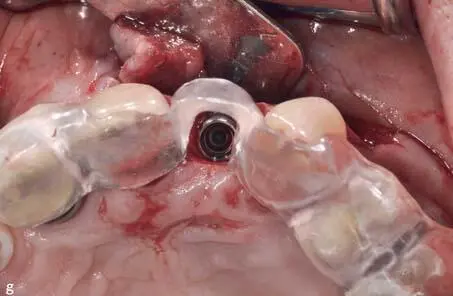
Figs 1-4-9a to 1-4-9g Step-by-step procedure at a conventional implant planning including a 2D radiographic analysis, manual diagnostic wax-up, and fabrication of a conventional surgical stent. The conventional surgical stent helps defining the best 3D prosthetically oriented position of the implant.
Читать дальше