81 Sobrino‐Guijarro B, Cascarini L, Lingam RK. 2013. Advances in imaging of obstructed salivary gland can improve diagnostic outcomes. Oral Maxillofac Surg 17:11–19.
82 Sokoloff L. 1961. Local Cerebral Circulation at Rest and During Altered Cerebral Activity Induced by Anesthesia or Visual Stimulation. In: S.S. Kety, J. Elkes (eds.) The Regional Chemistry, Physiology and Pharmacology of the Nervous System. Oxford, Pergamon Press, pp. 107–117.
83 Sokoloff L. 1986. Cerebral circulation, energy metabolism, and protein synthesis: General characteristics and principles of measurement. In: M. Phelps, J. Mazziotta, H. Schelbert (eds.) Positron Emission Tomography and Autoradiography: Principles and Applications for the Brain and Heart. Raven Press, pp. 1–71.
84 Som P, Curtin H (eds.). 1996. Head and Neck Imaging, 3rd edn. Mosby‐Year Book Inc, pp. 823–914.
85 Som P, Brandwein M, Silver A. 1995. Nodal inclusion cysts of the parotid gland and parapharyngeal space: A discussion of lymphoepithelial, AIDS‐related parotid and branchial cysts, cystic Warthin's tumors, and cysts in Sjogren's syndrome. Laryngoscope 105(10):1122–1128.
86 Stahl A, Dzewas B, Schwaige W, Weber W. 2002. Excretion of FDG into saliva and its significance for PET imaging. Nuklearmedizin 41:214–216.
87 Su Y, Liao G, Kang Z, Zou Y. 2006. Application of magnetic resonance virtual endoscopy as a presurgical procedure before sialoendoscopy. Laryngoscope 116:1899–1906.
88 Sugai S. 2002. Mucosa‐associated lymphoid tissue lymphoma in Sjogren's syndrome. AJR 179:485–489.
89 Suh J, Abenoza P, Galloway H et al. 1992. Peripheral (extracranial) nerve tumors: Correlation of MR imaging and histologic findings. Radiology 183:341–346.
90 Sumi M, Izumi M, Yonetsu K, Nakamura T. 1999a. Sublingual gland: MR features of normal and diseased states. AJR 172(3):717–722.
91 Sumi M, Izumi M, Yonetsu K, Nakamura T. 1999b. The MR imaging assessment of submandibular gland sialoadenitis secondary to sialolithiasis: Correlation with CT and histopathologic findings. Am J Neuroradiol 20:1737–1743.
92 Sumi M, Yamada T, Takagi Y, Nakamura T. 2007. MR imaging of labial glands. Am J Neuroradiol 28:1552–1556.
93 Takagi Y, Sumi M, Sumi T et al. 2005a. MR microscopy of the parotid glands in patients with Sjogren's syndrome: Quantitative MR diagnostic criteria. Am J Neuroradiol 26:1207–1214.
94 Takagi Y, Sumi M, Van Cauteren M, Nakamura T. 2005b. Fast and high resolution MR sialography using a small surface coil. J Magn Reson Imaging 22:29–37.
95 Takahashi N, Okamoto K, Ohkubo M, Kawana M. 2005. High‐resolution magnetic resonance of the extracranial facial nerve and parotid duct: Demonstration of the branches of the intraparotid facial nerve and its relation to parotid tumours by MRI with a surface coil. Clin Radiol 60:349–354.
96 Takashima S, Takeuchi N, Morimoto S et al. 1991. MR imaging of Sjogren's syndrome: Correlation with sialography and pathology. J Comput Assist Tomogr 15(3):393–400.
97 Takashima S, Tomofumi N, Noguchi Y et al. 1992. CT and MR appearances of parotid pseudotumors in Sjogren's syndrome. J Comput Assist Tomogr 16(3):376–383.
98 Tanaka T, Ono K, Habu M et al. 2007. functional evaluation of the parotid and submandibular glands using dynamic magnetic resonance sialography. Dentom Radiol 36:218–223.
99 Tatsumi M, Engles J, Ishimori T et al. 2004. Intense 18F‐FDG uptake in Brown fat can be reduced pharmacologically. J Nucl Med 45:1189–1193.
100 Thoeny H. 2007. Imaging of Salivary gland tumors. Cancer Imaging 7:52–62.
101 Tonami H, Munetaka M, Yokata H et al. 2002. Mucosa‐associated lymphoid tissue lymphoma in Sjogren’s syndrome: Initial and follow‐up imaging features. AJR 179:485–489.
102 Uchida Y, Minoshima S, Kawata T et al. 2005. Diagnostic value of FDG PET and salivary gland scintigraphy for parotid tumors. Clin Nucl Med 30:170–176.
103 Wan Y, Chan S, Chen Y. 2004. Ultrasonography‐guided core‐needle biopsy of parotid gland masses. Am J Neuroradiol 25:1608–1612.
104 Wang Y, Chiu E, Rosenberg J, Gambhir S. 2007. Standardized uptake value atlas: Characterization of physiological 2‐deoxy‐2‐[18F]fluoro‐D‐glucose uptake in normal tissues. Mol Imaging Biol 9(2):83–90.
105 Warburg O. 1925. Uber den Stoffwechsel der Carcinom‐Zelle. Klin Wochenschr 4:534–536.
106 White D, Davidson H, Harnsberger H et al. 2001. Accessory salivary tissue in the mylohyoid boutonnière: A clinical and radiologic pseudolesion of the oral cavity. Am J Neuroradiol 22:406–412.
107 Witt BL, Schmidt RL. 2014. Ultrasound‐guided core needle biopsy of salivary gland lesions: A systematic review and meta‐analysis. Laryngoscope 124:695–700.
108 Wong K, Ahuja A, King A et al. 2004. Vascular lesion in the parotid gland in adult patients: Diagnosis with high‐resolution ultrasound and MRI. British J Radiol 77:600–606.
109 Yabuuchi H, Fukuya T, Tajima T et al. 2003. Salivary gland tumors: Diagnostic value of gadolinium enhanced dynamic MR imaging with histopathologic correlation. Radiology 226:345–354.
110 Yerli H, Aydin E, Coskum M et al. 2007. Dynamic multislice CT of parotid gland. J Comput Assist Tomogr 31(2):309–316.
Chapter 3 Infections of the Salivary Glands
Outline
Introduction
General Considerations
Bacterial Salivary Gland Infections Acute Bacterial Parotitis Variants of ABP and Their Etiology Diagnosis of Acute Bacterial Parotitis Treatment of Acute Bacterial Parotitis Chronic (Recurrent or Refractory) Bacterial Parotitis Treatment of Chronic Bacterial Parotitis Chronic Recurrent Juvenile Parotitis Treatment of Chronic Recurrent Juvenile Parotitis Acute Bacterial Submandibular Sialadenitis Treatment of Acute Bacterial Submandibular Sialadenitis Chronic Recurrent Submandibular Sialadenitis Bartonella Henselae (Cat‐Scratch Disease) Tuberculous Mycobacterial Disease Nontuberculous Mycobacterial Disease
Viral Salivary Gland Infections Mumps Human Immunodeficiency Virus Influenza A
Bacterial Sialadenitis in Pregnancy
Autoimmune Sialadenitis and IgG4‐Related Disease
Summary
Case Presentation – Gadzooks
References
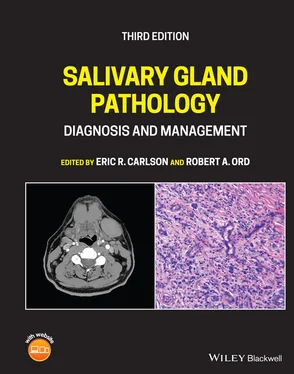
Most non‐neoplastic swellings of the major salivary glands represent acute or chronic infections of these glands. Sialadenitis, a generic term used to describe infection of the salivary glands, has a diverse range of signs and symptoms and predisposing factors. Although any of the major and minor salivary glands can become infected, these conditions most commonly occur in the parotid ( Figure 3.1) and submandibular glands ( Figure 3.2), with minor salivary gland and sublingual gland infections being very rare. From an etiologic standpoint, these infections may be related to underlying bacterial, viral, fungal, mycobacterial, parasitic, or immunologically mediated inflammation/infections (Miloro and Goldberg 2002). The most common of these diagnoses include acute bacterial parotitis and acute submandibular sialadenitis (see Table 3.1). Numerous risk factors may predispose patients to sialadenitis. The classic risk factor is the hospitalized patient who recently underwent surgery with general anesthesia. Additionally, dehydration (insufficient intake) may contribute to sialadenitis, as may chronic nausea/vomiting (excessive output) in hospitalized patients. Both conditions decrease intravascular volume, thereby decreasing perfusion of salivary gland tissue with resultant decreased salivary flow. In general terms, stasis and decreased salivary flow predispose patients to sialadenitis, although, medications and comorbid diagnoses may also contribute to this diagnosis (see Table 3.2).
Читать дальше