Pathology of the Salivary Glands
Pathologic states of the salivary glands include tumors (epithelial and non‐epithelial), infections and inflammation, autoimmune diseases, vascular lesion, and non‐salivary tumors.
Of all salivary gland tumors, most (80%) are found in the parotid gland. The submandibular gland contains approximately 10% with the remainder in the sublingual and minor salivary glands. Of all parotid gland tumors, 80% are benign and 20% malignant. About 50% of submandibular gland tumors are benign and most of sublingual gland tumors are malignant. About 50% of minor salivary gland tumors are benign. The smaller the gland, the more likely that a mass within it is malignant. The pleomorphic adenoma and papillary cystadenoma lymphomatosum (Warthin tumor) account for most of benign salivary tumors, with the former being the more common at about 80% of benign and latter less common at about 15% of benign masses. Most of the malignant salivary gland tumors are represented by mucoepidermoid and adenoid cystic carcinomas.
Malignancies of the parotid gland may result in metastatic involvement of intraparotid and adjacent level II, and III jugular chain lymph nodes. The SMG drains primarily into adjacent level IB lymph nodes and then into the jugular chain and deep cervical nodes. The SLG drains into both level IA and IB nodes and then subsequently into the jugular chain and deep cervical nodes.
VASCULAR LESIONS
Lymphangioma (Cystic Hygroma)
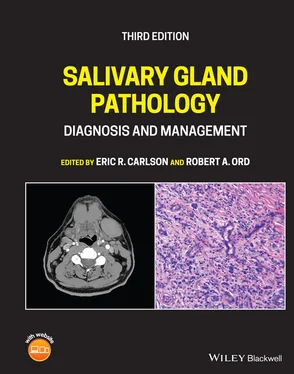
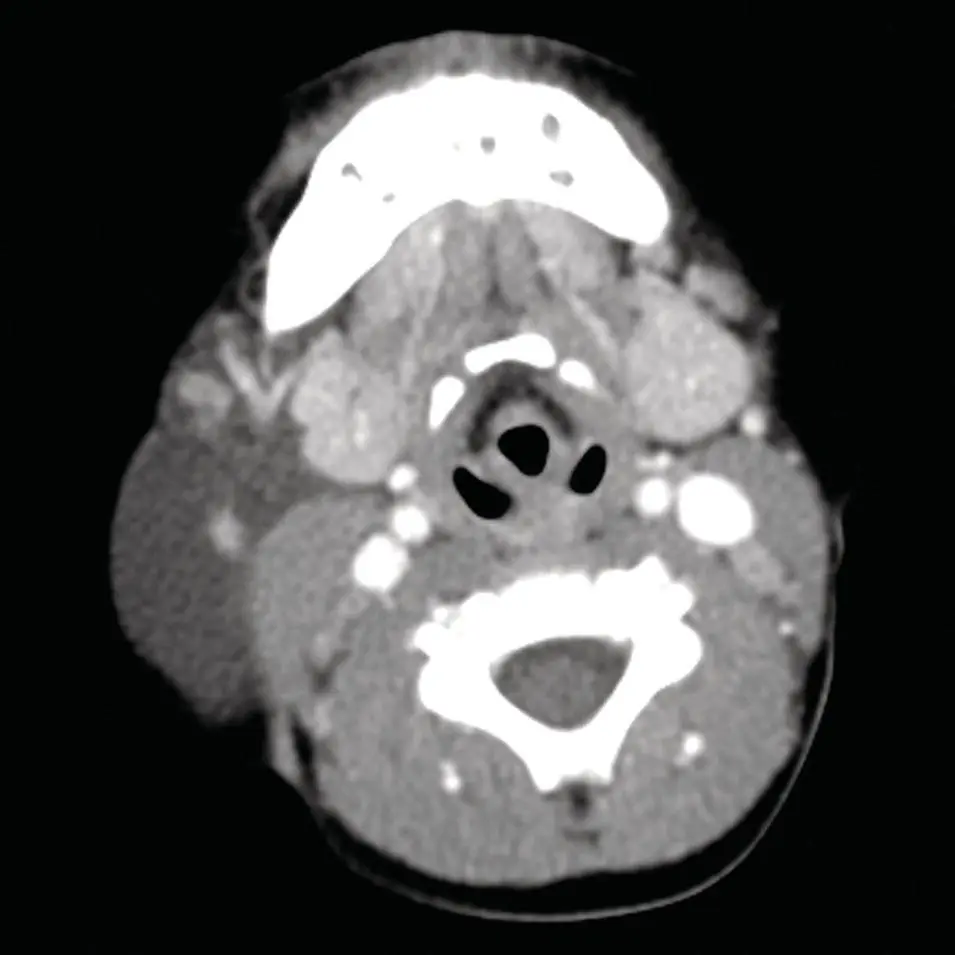
The cystic hygroma is included in this discussion because of its transpatial location and that it might mimic other cystic masses. It is typically multilocular and has an epicenter in the posterior triangle, but may be found in the submandibular space and less commonly in the sublingual space. The imaging characteristics are those of cysts and follow fluid density on CT and signal intensity on MRI, although do typically demonstrate internal architecture from septation with varying thickness. CT typically demonstrates isodensity to simple fluid or slight hyperdensity if infected or contains products of hemorrhage (Koeller et al. 1999; Makariou et al. 2003) ( Figure 2.47). US demonstrates anechoic spaces consistent with simple fluid with septa of variable thickness. Like cystic (and few solid lesions) lesions, there is increased thru transmission. Infection and hemorrhage cause variable degrees of echogenicity and thicker septations (Koeller et al. 1999; Makariou et al. 2003). MRI, however, can be variable on both T1 and T2 sequences based on the fluid characteristics. With simple fluid, T1 and T2 are isointense to simple fluid (CSF) but with infection, or hemorrhage products, the increased protein concentration as well as cellular debris and iron from hemoglobin can result in varying degrees of T1 hyperintensity and variable hypo‐ or hyperintensity on T2 ( Figure 2.48). Any of these modalities may demonstrate fluid‐fluid or fluid‐debris layers. Both CT and MRI will demonstrate enhancement in the setting of infection (Macdonald et al. 2003). These lesions are more common in the pediatric age group, although small lesions may persist into adulthood. When found in the submandibular or sublingual space, they may be mistaken for a ranula (especially giant or plunging ranulae) and less likely hemangioma or thyroglossal duct cyst if midline (Kurabayashi et al. 2000; Macdonald et al. 2003). Although dermoids are in the differential diagnosis, they are usually identified by their imaging characteristics secondary to their contents of fat and dermal elements. Epidermoid cysts may be more difficult to differentiate from cystic hygromas and ranulae because of similar imaging characteristics (Koeller et al. 1999). Because the lymphangiomas have a vasculolymphatic origin, they may be associated with venous anomalies and rarely saccular venous aneurysms (Makariou et al. 2003). Vascular flow signals may be seen with Doppler US. The venous anomalies or aneurysms may be difficult to differentiate from other vascular malformations; however, their association with typical findings of lymphangiomas may assist in diagnosis.
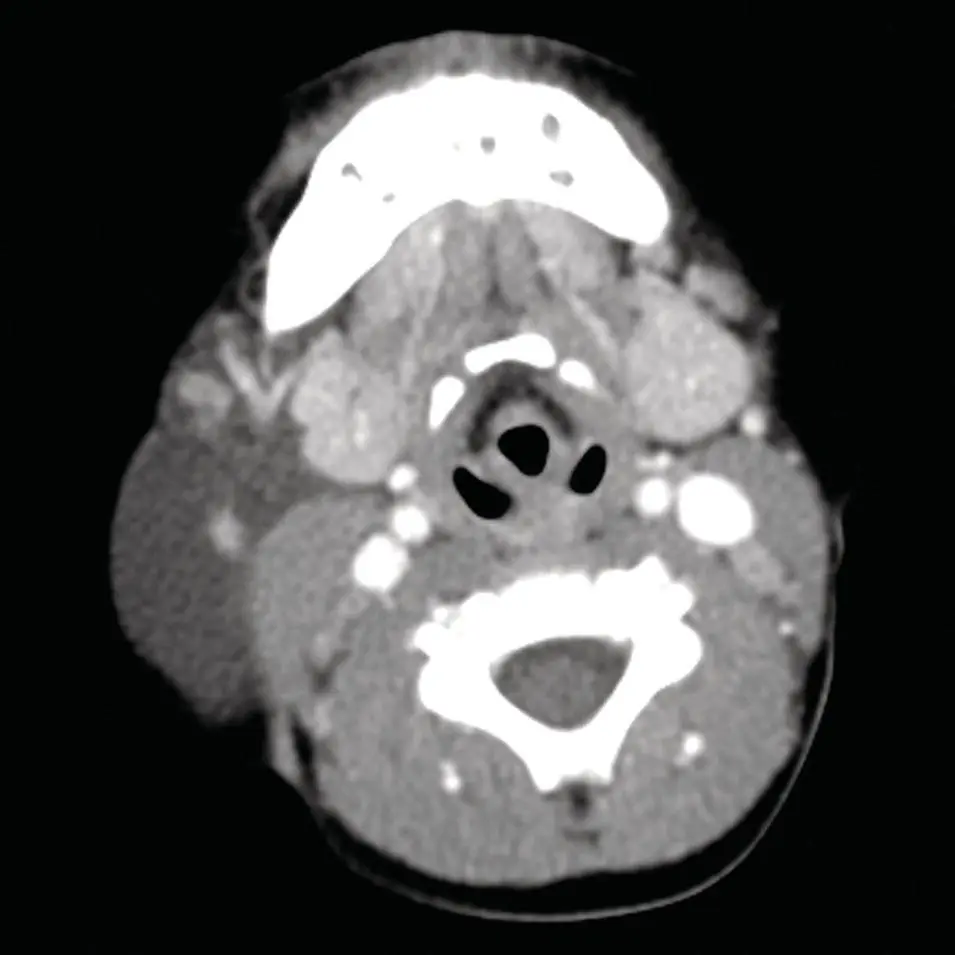
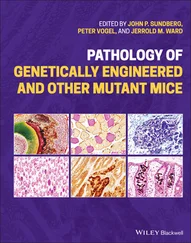
Figure 2.47. Axial contrast‐enhanced CT of the neck at the level of the submandibular glands demonstrating a low‐density structure on the right of approximately fluid density (compare to the CSF in the spinal canal), which is intermediate in density relative to the muscles and subcutaneous fat. A large lymphangioma associated with the right submandibular gland was diagnosed.
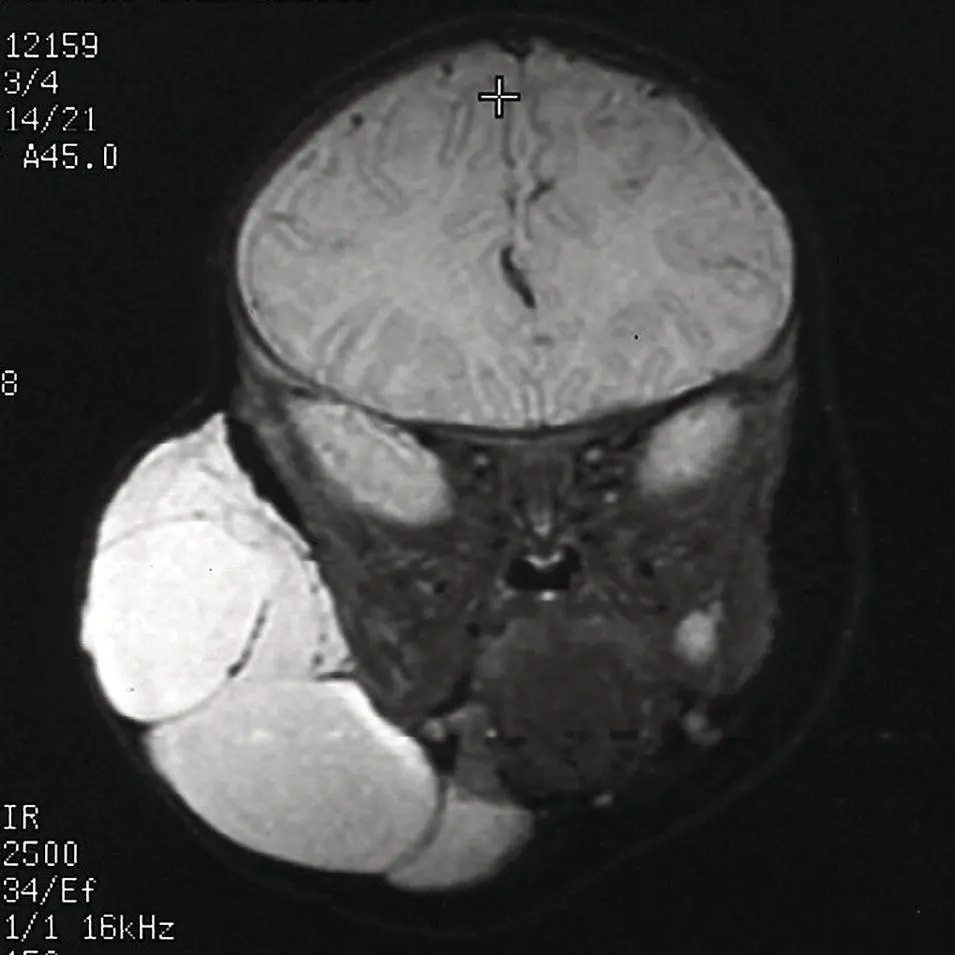
Figure 2.48. Coronal STIR MRI of the face of a different patient with a very large lymphangioma with large septations. Note the lymphangioma fluid is brighter than the CSF and there is fat suppression of the subcutaneous fat.
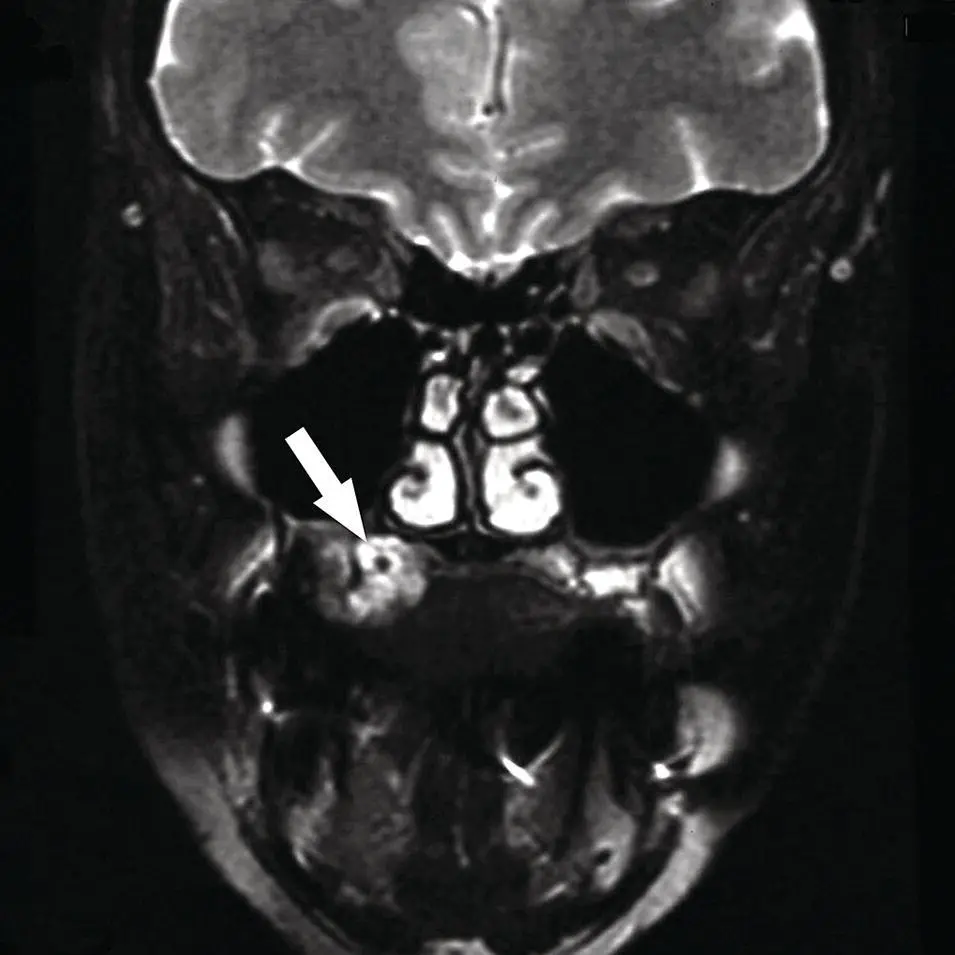
Hemangiomas are typically found in the pediatric age group. The majority are of the cavernous type and less likely the capillary type. They are best demonstrated by MRI and show marked enhancement. They are also very bright on T2 MRI. Foci of signal void may be vascular channels or phleboliths ( Figures 2.49– 2.51). They are typically slow flow lesions and may not be angiographically evident. US can vary from hypoechoic to heterogenous (Wong et al. 2004).
Other rare vascular lesions within salivary glands, most commonly the parotid gland, include aneurysms, pseudoaneurysms, and arteriovenous fistulae (AVFs). The aneurysms or pseudoaneurysms are most commonly associated with trauma or infection (mycotic). MRI in high flow lesions demonstrates “flow voids” or an absence of signal but slow flow lesions or turbulent flow can demonstrate heterogenous signal mimicking a mass. Contrast enhancement and MRA can help delineate vascular lesions from masses. CT without contrast however demonstrates a mass or masses isodense to skeletal muscle or normal blood vessels. With contrast, large vascular channels become more obvious, although smaller lesions may still mimic a mass. US (especially Doppler US) can reveal characteristic flow patterns of arterial waveforms in the venous channels for AVFs. US can also delineate aneurysms with their turbulent flow patterns. Angiography is typically reserved for endovascular treatment. CTA or MRA is useful for noninvasive assessment of arterial feeders and venous anatomy in AVFs and in defining aneurysms (Wong et al. 2004).

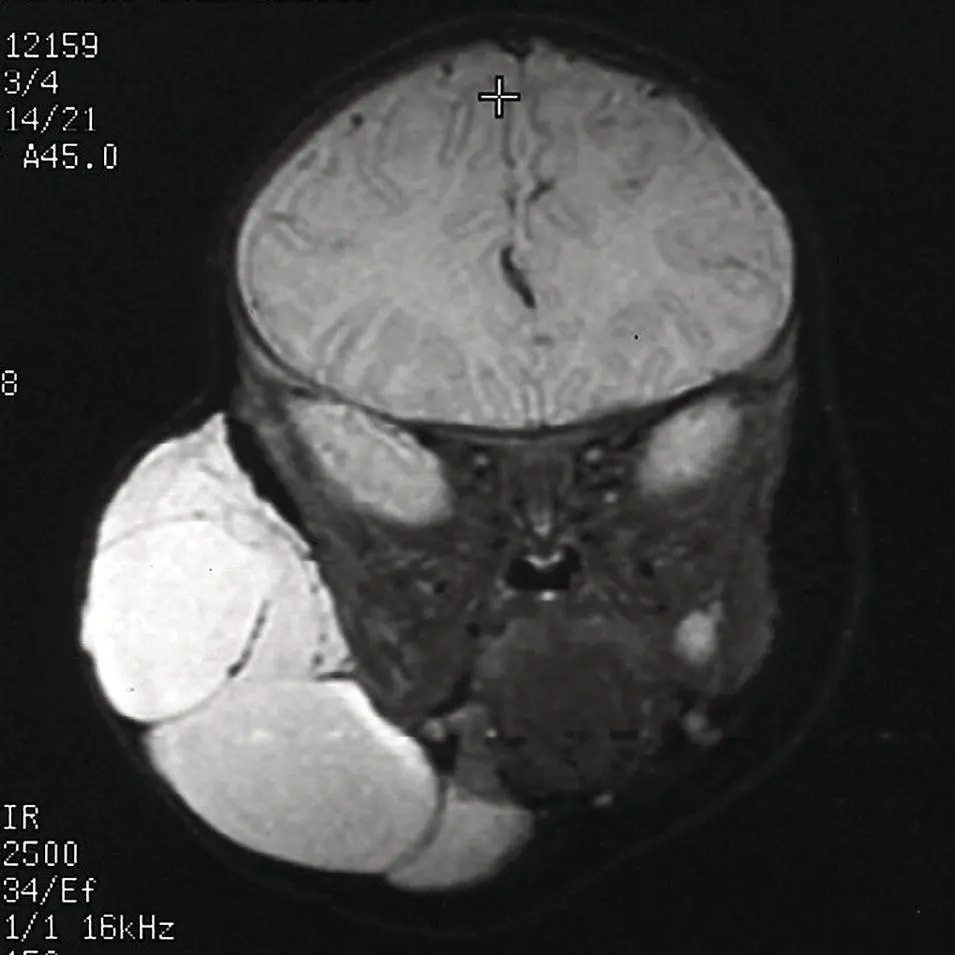
Figure 2.49. Direct coronal CT displayed in bone window demonstrating smooth erosion of the hard palate on the right lateral aspect, along with a dense calcification consistent with a phlebolith (arrow). A hemangioma is presumed based on this CT scan.

Figure 2.50.Coronal fat suppressed contrast‐enhanced T1 MRI image corresponding to the same level as Figure 2.49, demonstrating a sharply marginated homogenously enhancing mass (arrow).
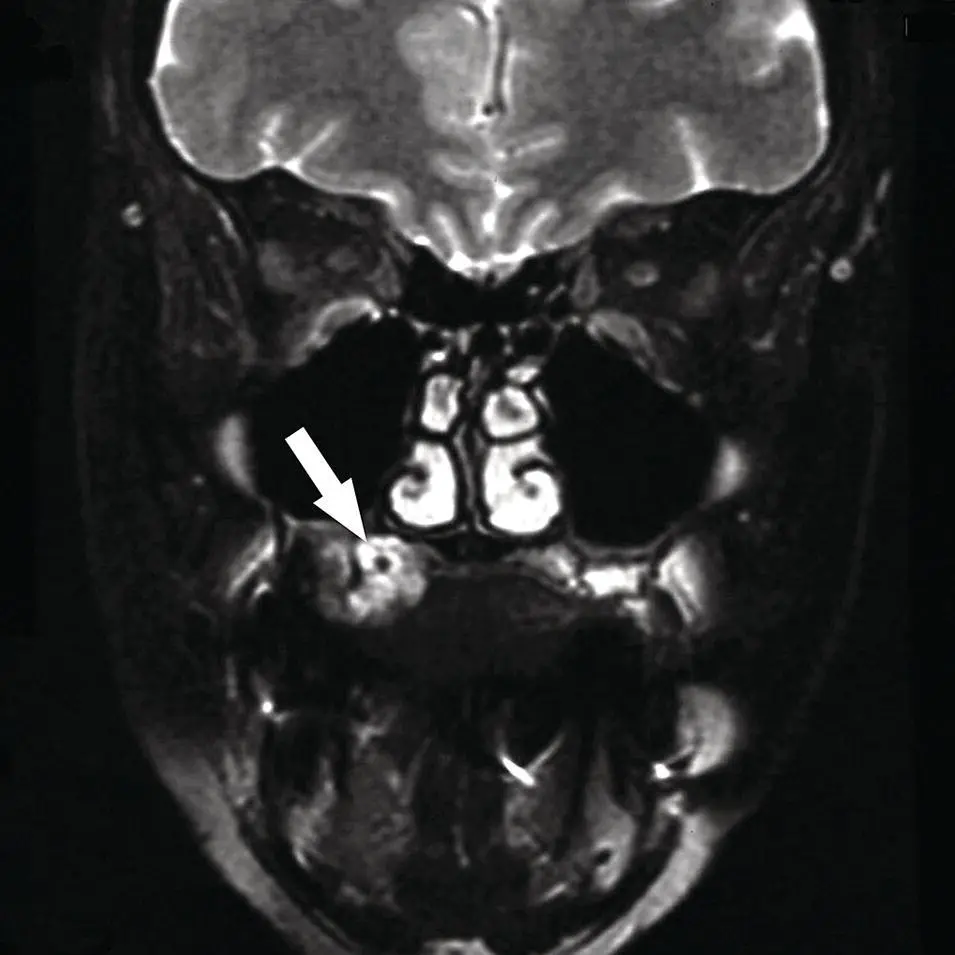
Figure 2.51. Coronal fat saturated T2 MRI image demonstrating a well‐demarcated hyperintense mass with a focal signal void centrally. A hemangioma containing a phlebolith (arrow) was presumed based on this MRI.
Читать дальше