The submandibular duct emanates from the anterior‐superior aspect of the gland and turns anteriorly and lies along the superior surface of the mylohyoid muscle between the genioglossus muscle medially and the sublingual gland laterally. The ducts open into the anterior medial (paramidline) floor of mouth at the sublingual papillae.
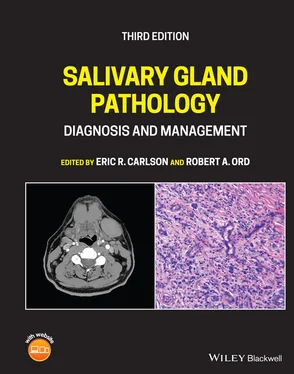
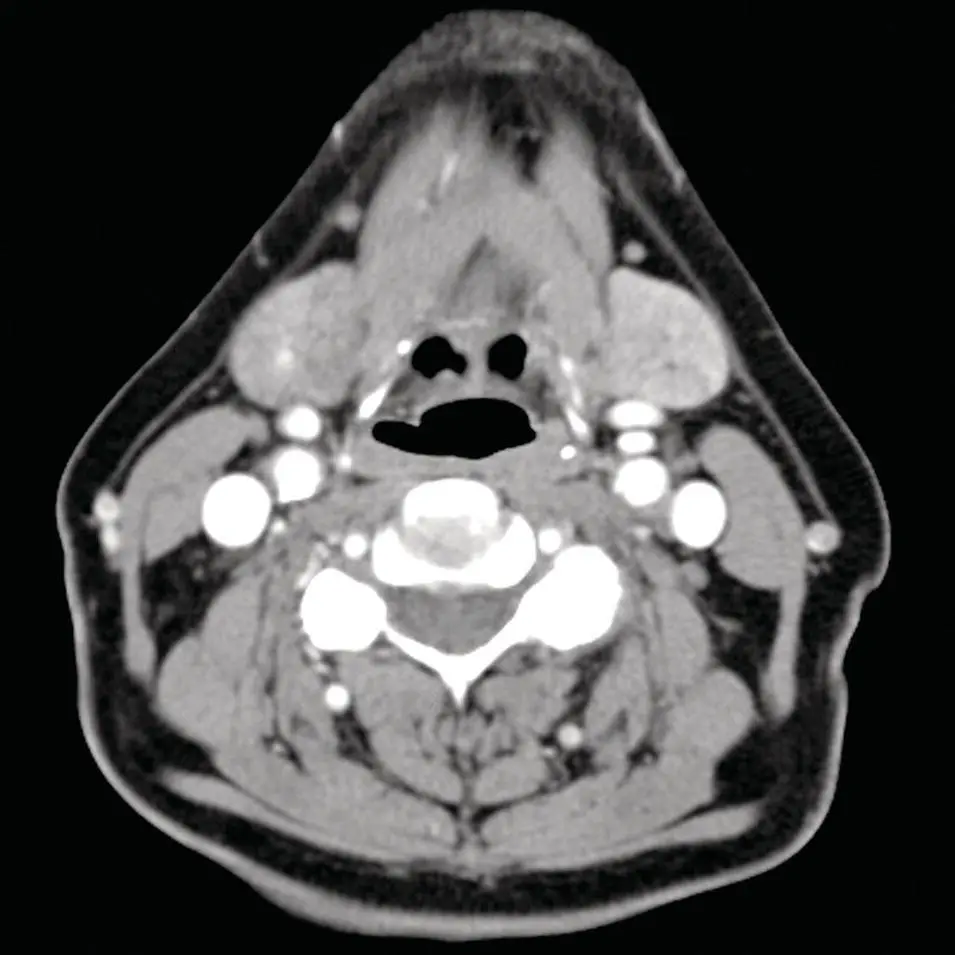
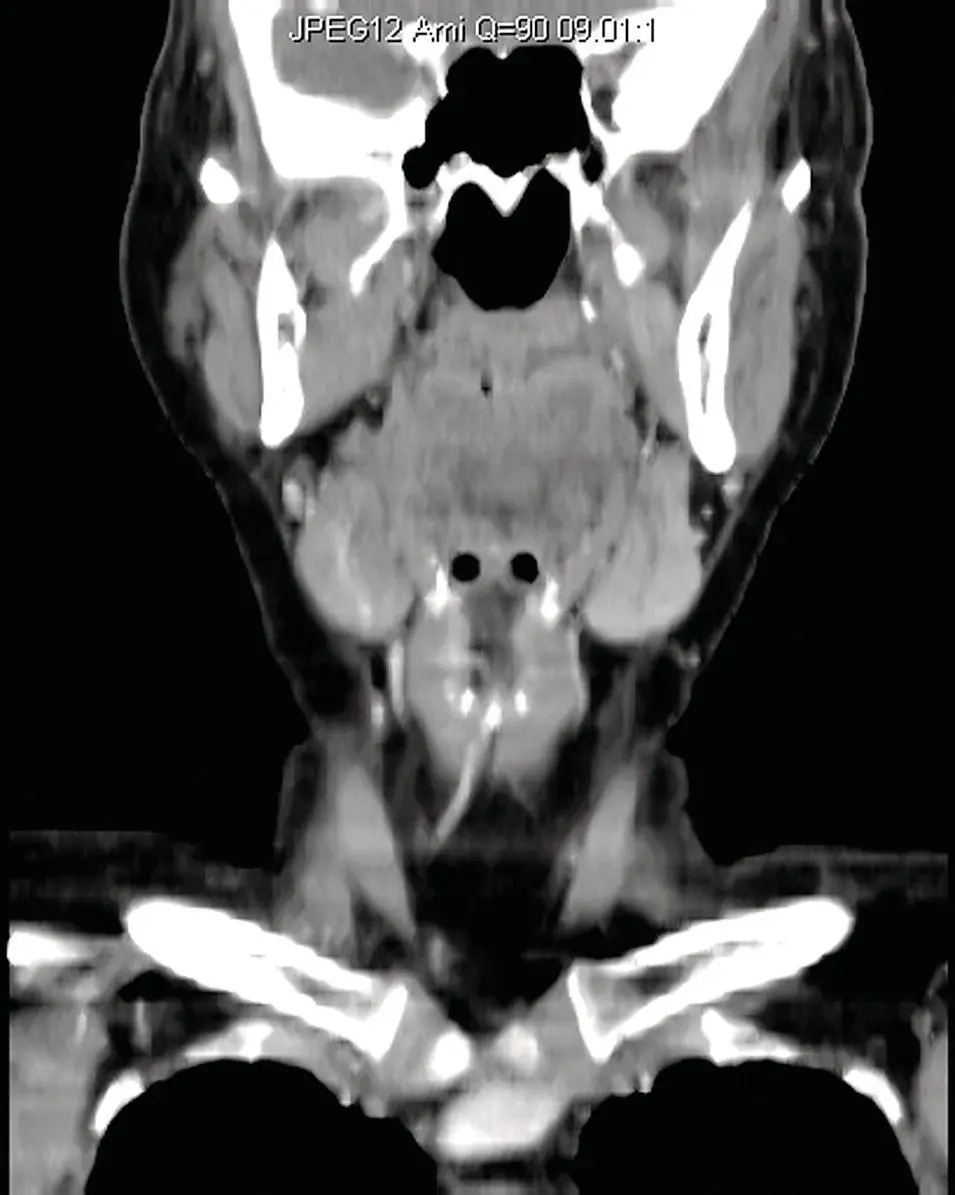
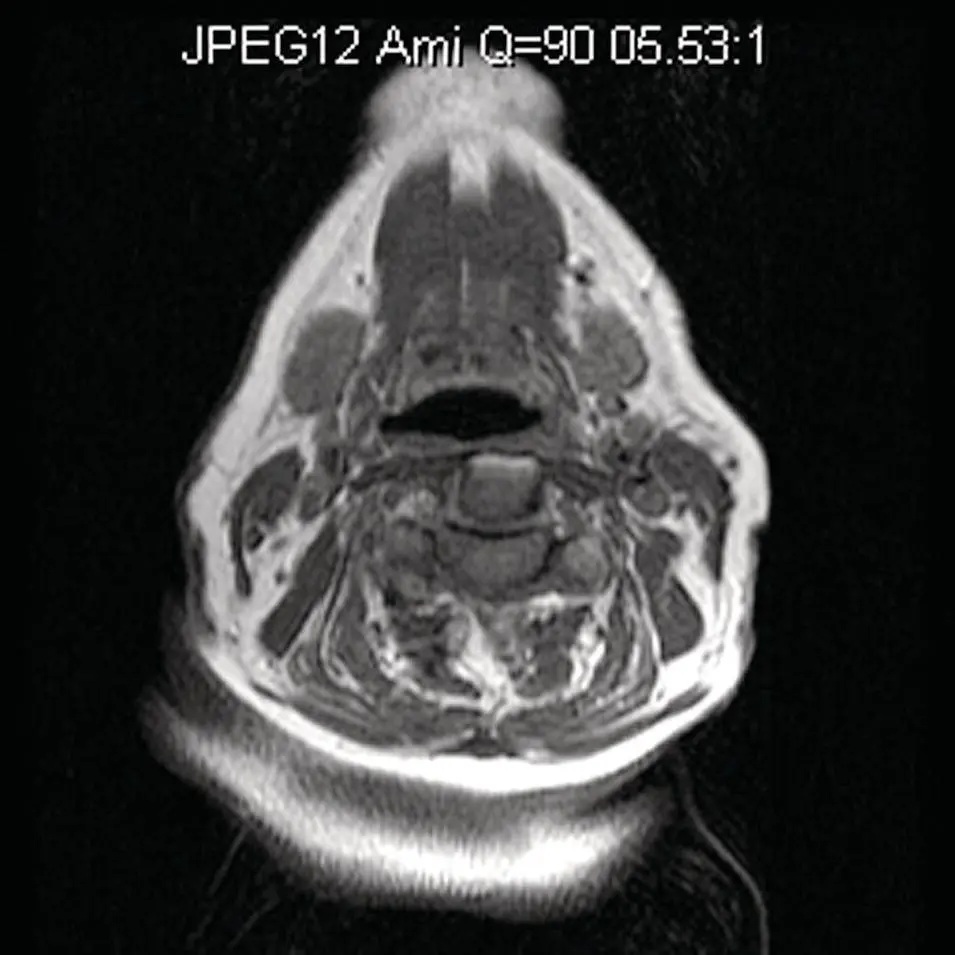
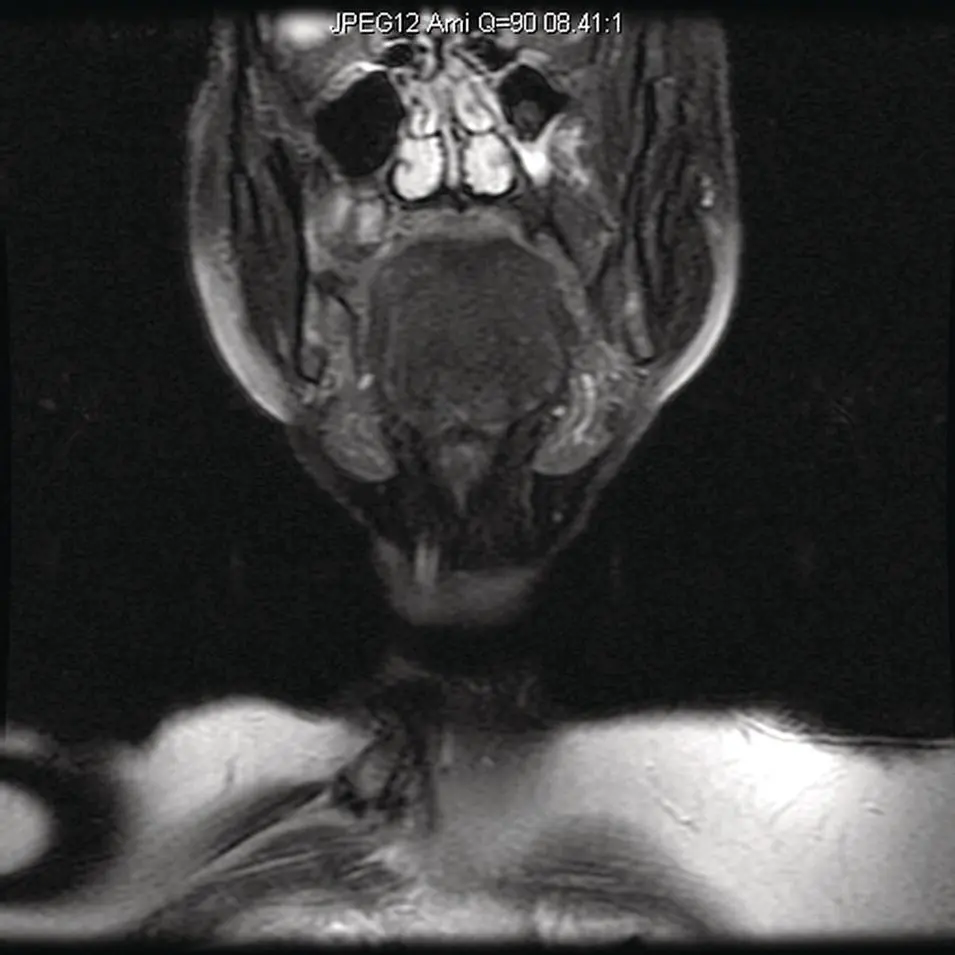
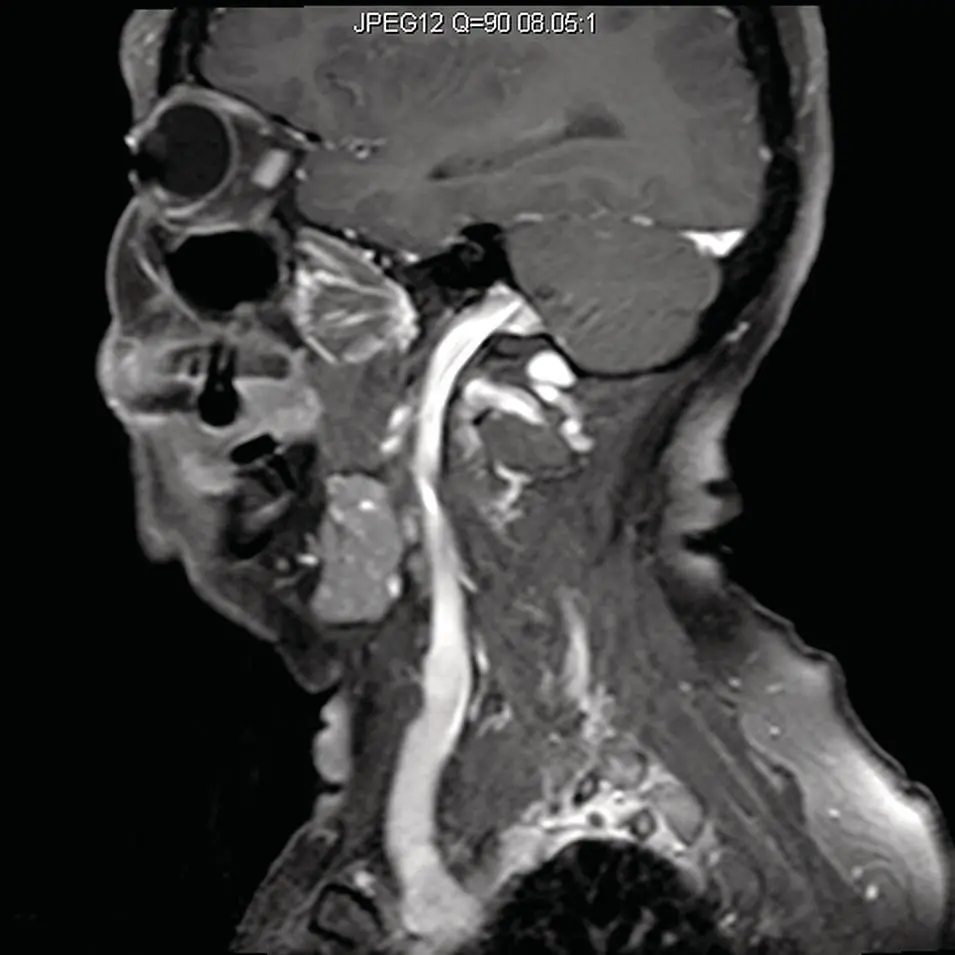
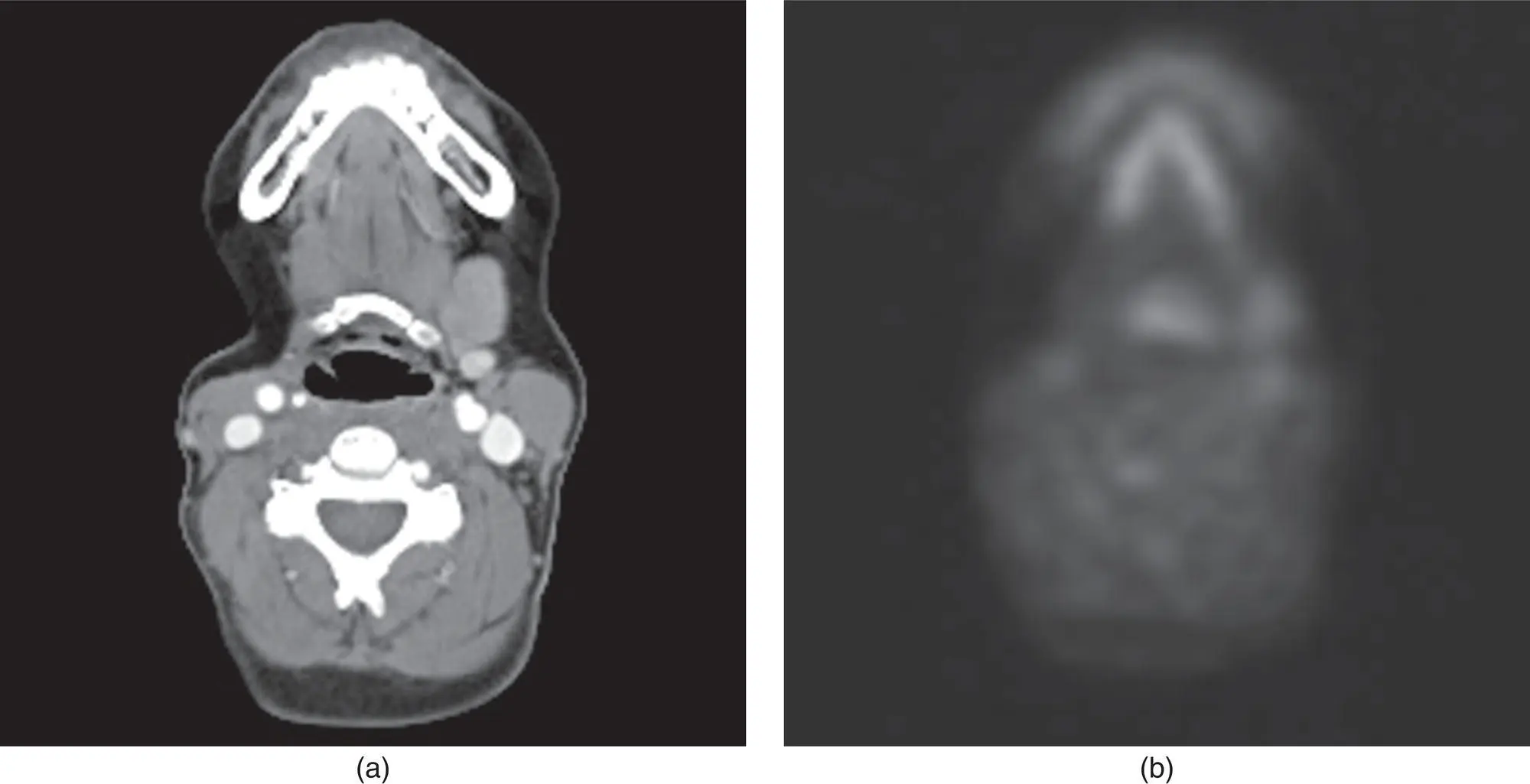
On CT scans the submandibular gland has a density that is isodense to slightly hyperdense relative to skeletal muscle. The gland does not become as fatty replaced as the parotid gland. The SMG demonstrates a signal characteristic like that of skeletal muscle on T1 and T2 weighted images and is less intense when compared to the parotid gland secondary to less fatty replacement. The FDG uptake is moderate but higher than that of the parotid gland. The SMG undergoes contrast enhancement by CT and MRI (Kaneda 1996).
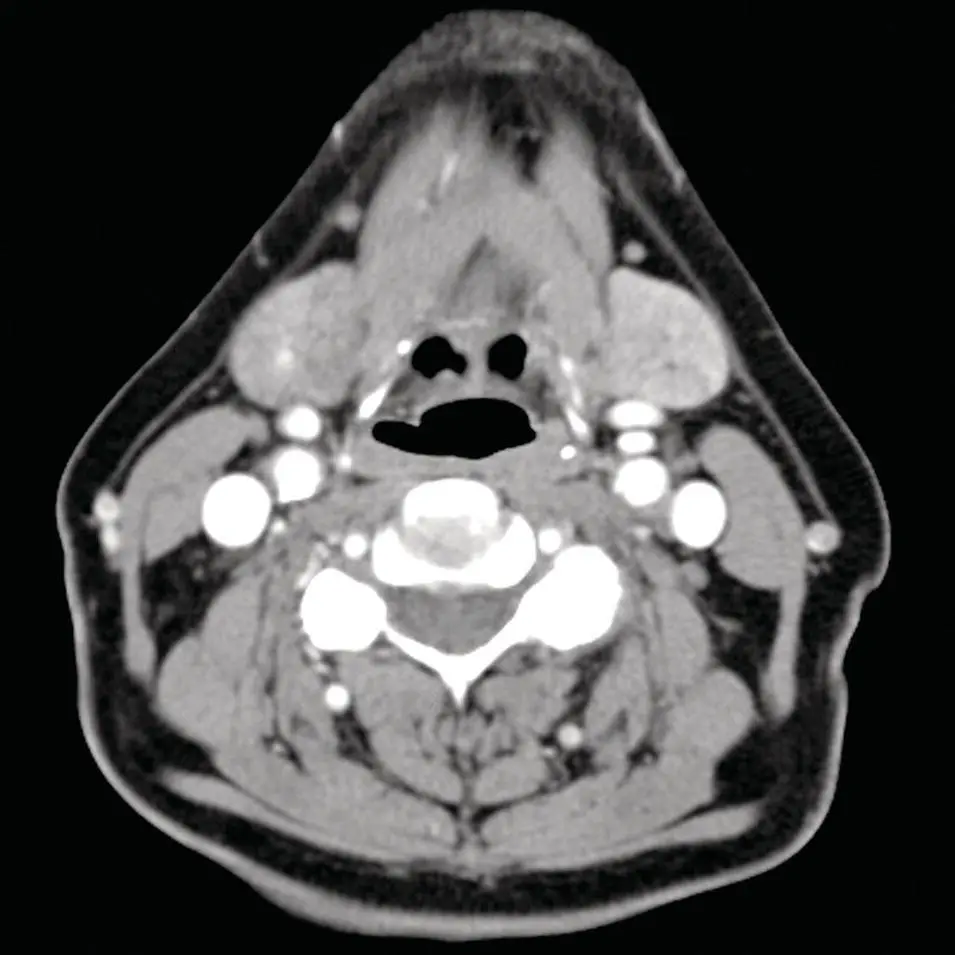
Figure 2.37. Axial CT at the level of the submandibular gland demonstrating density higher then skeletal muscle.
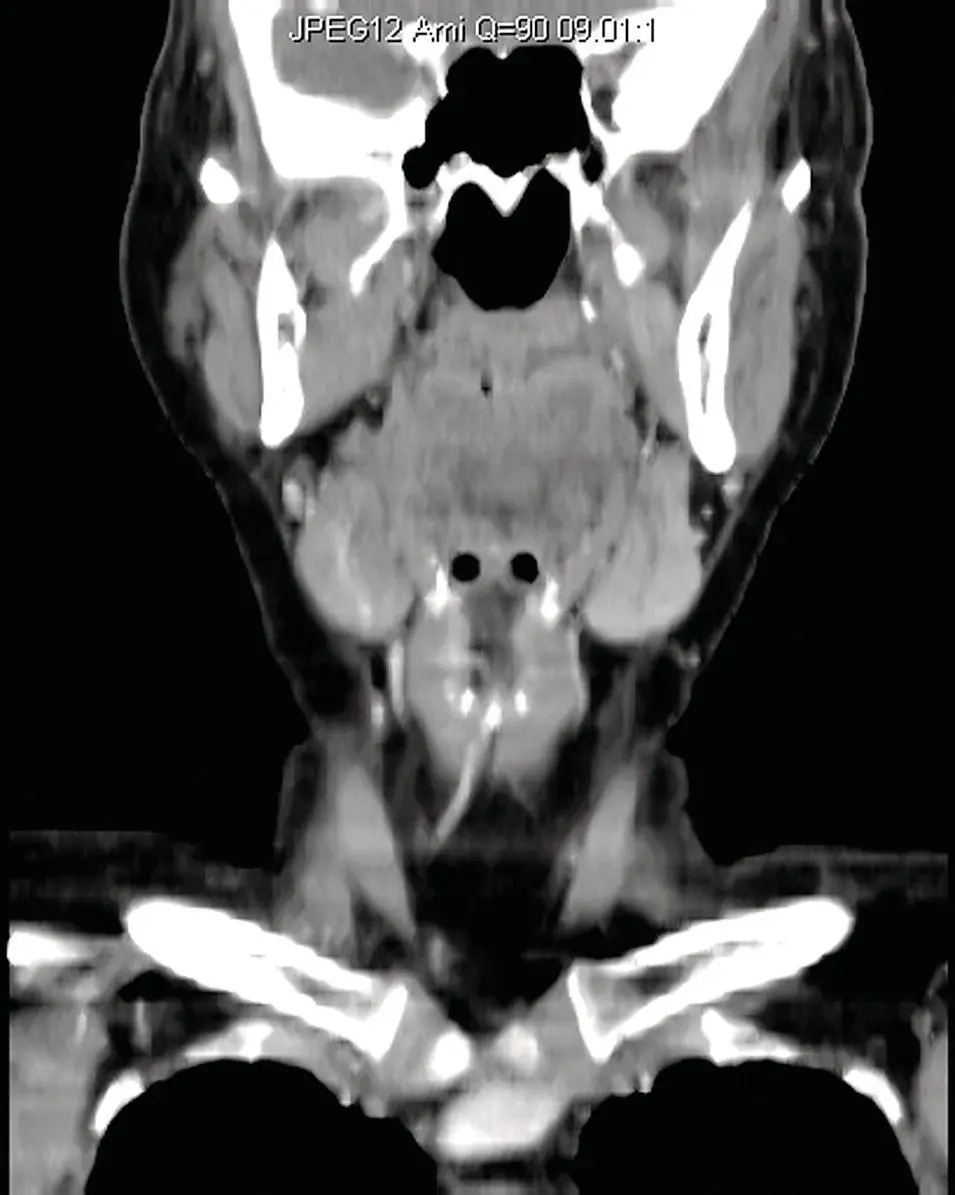
Figure 2.38.Reformatted coronal CT at the level of the submandibular gland demonstrating its relationship to the mylohyoid muscle and floor of mouth.

Figure 2.39.Reformatted sagittal CT at the level of the submandibular gland demonstrating its relationship to the floor of mouth. Note the slight notch at the hilum of the gland. Majority of the gland “hangs” below the mylohyoid muscle.
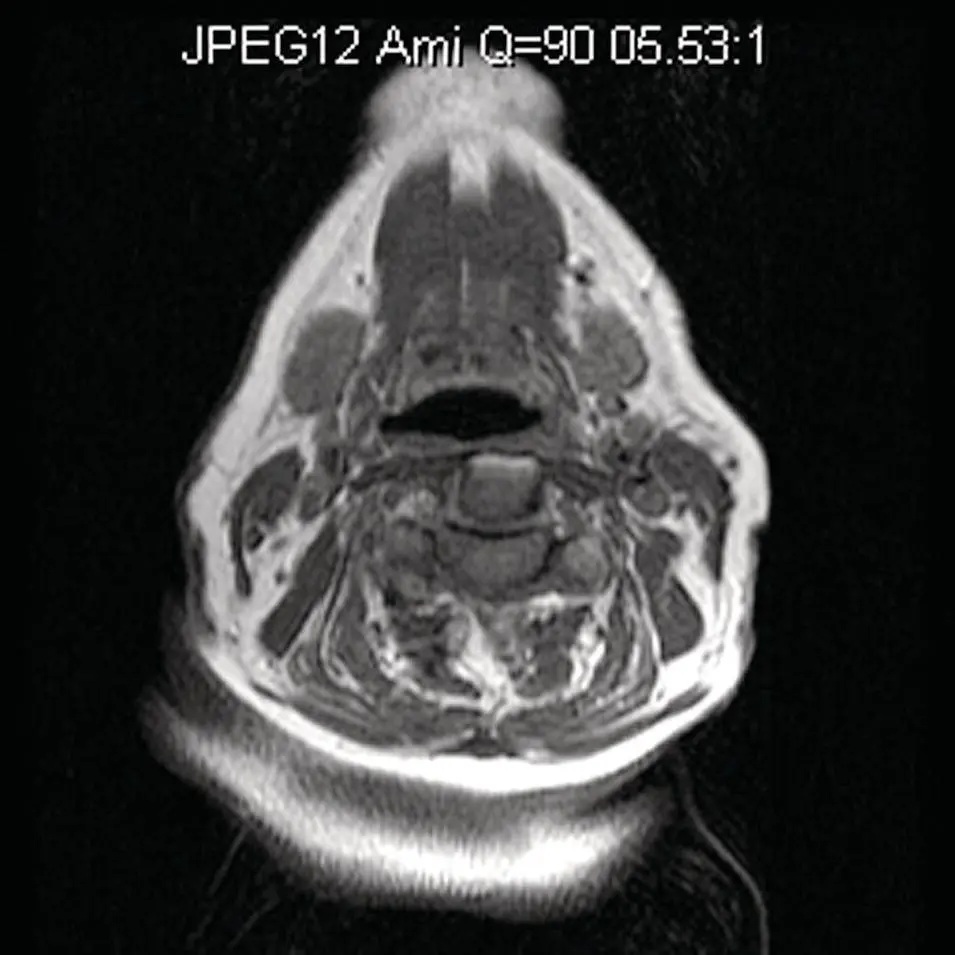
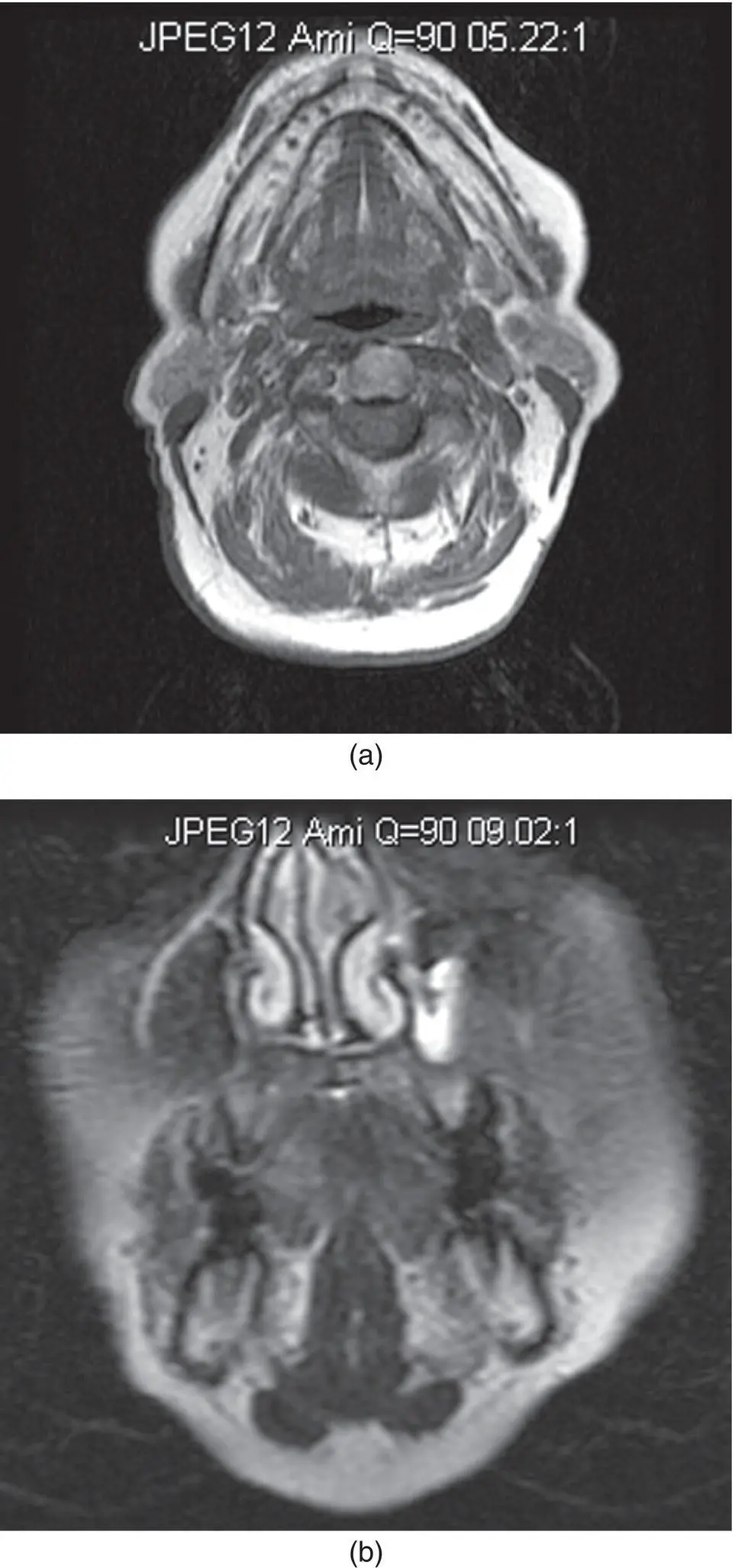
Figure 2.40.Axial T1 MRI of the submandibular gland demonstrating slight hyperintensity to muscle. Note the bright subcutaneous fat.
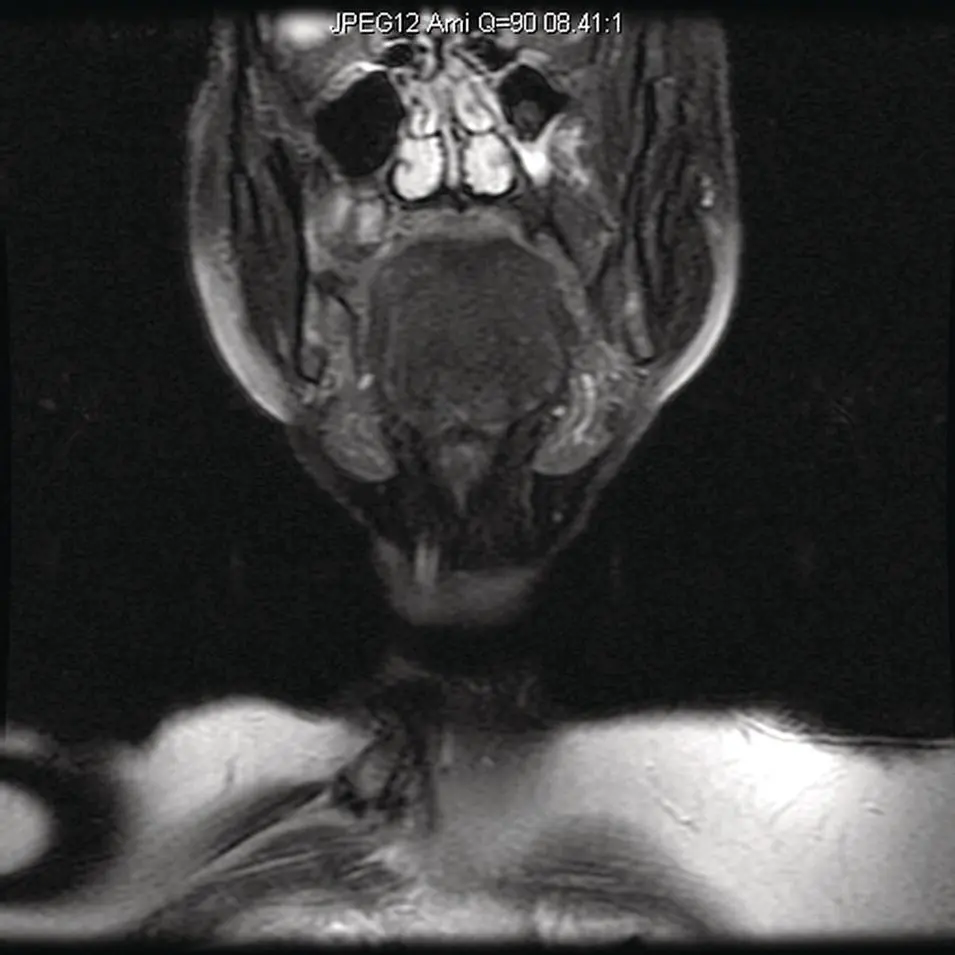
Figure 2.41.Coronal fat saturated T2 MRI of the submandibular gland. Note the slightly incomplete fat suppression and the engorged and edematous mucosa of the nasal cavity and turbinates.
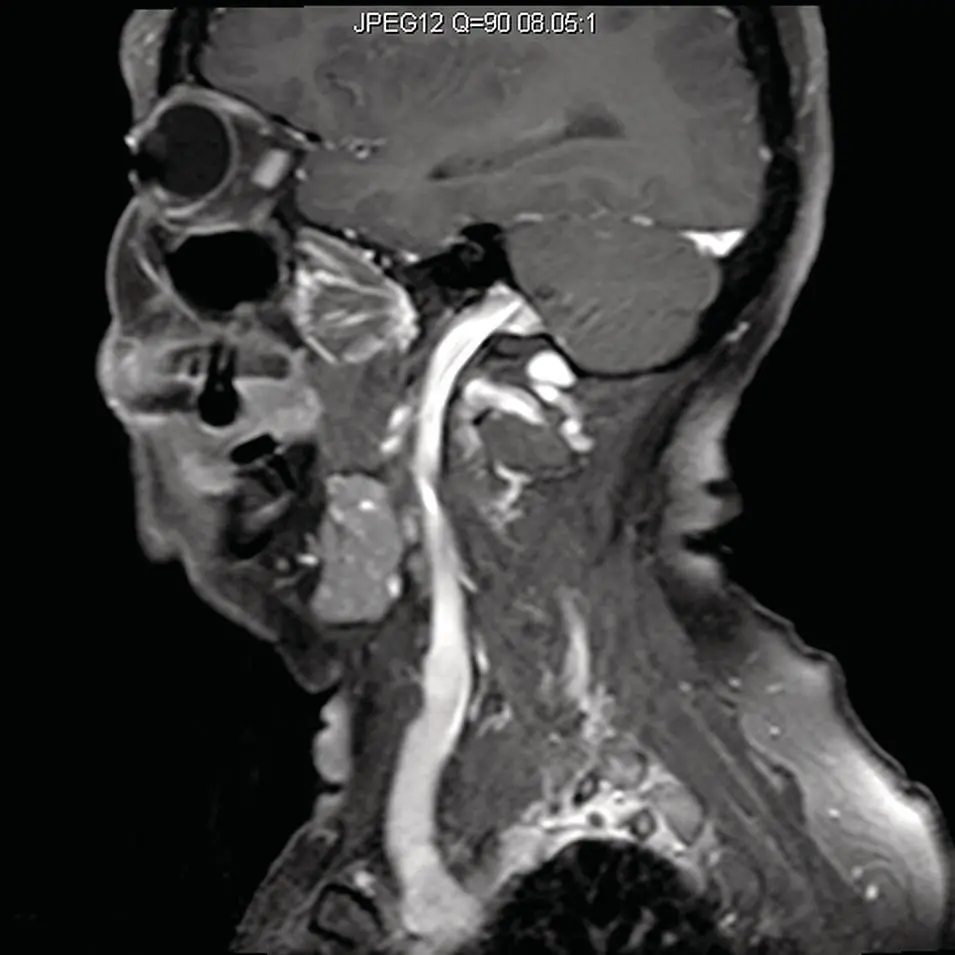
Figure 2.42.Sagittal T1 fat saturated MRI of the submandibular gland demonstrating the well‐defined appearance on a fat suppressed background. Note the slight notch at the hilum. Note the entire internal jugular vein is visualized.
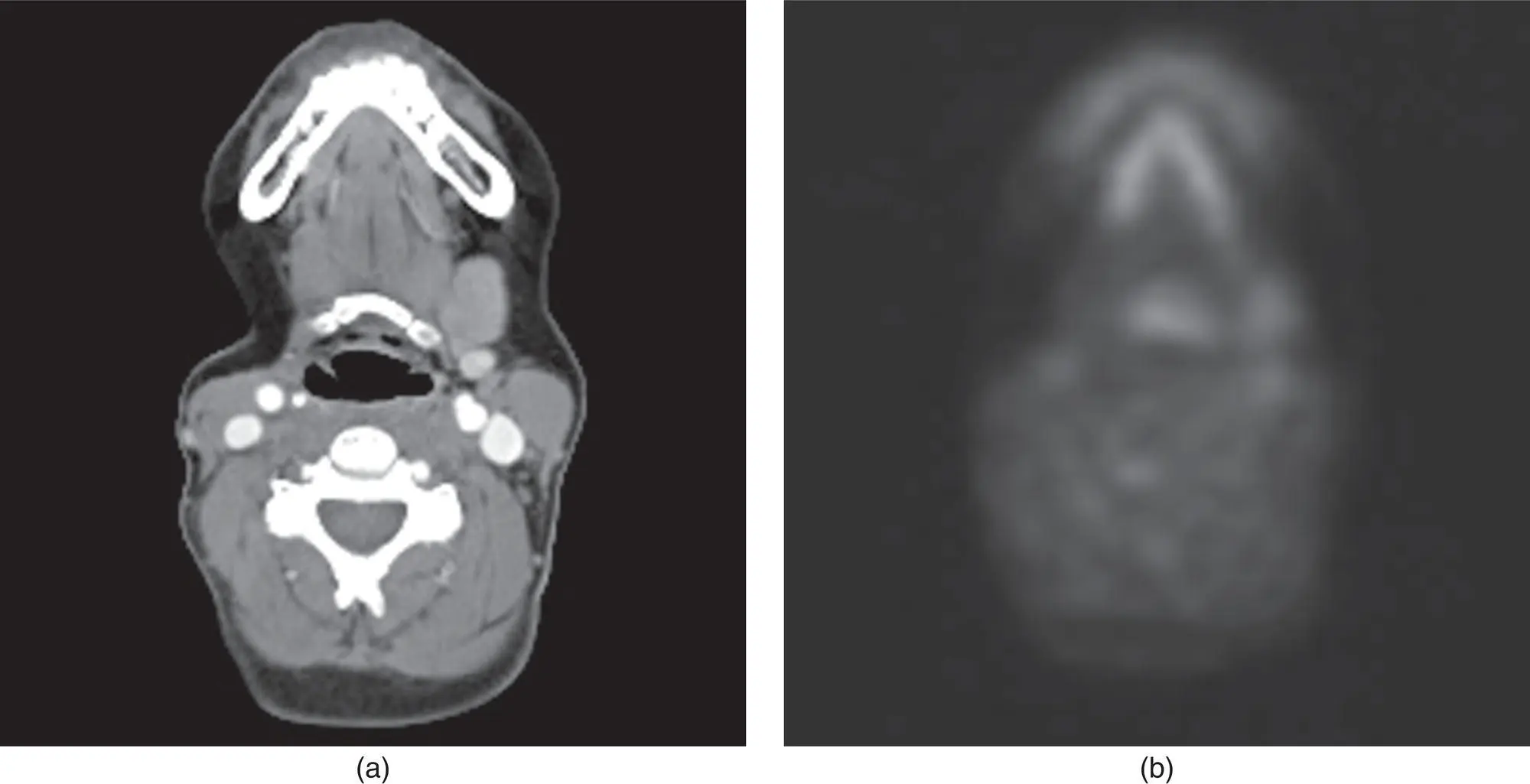
Figure 2.43. Axial CT (a) and corresponding PET (b) of the submandibular gland demonstrating slight normal uptake. Note the strong asymmetry of uptake on the PET corresponds to the absent submandibular gland on the right confirmed by the CT.
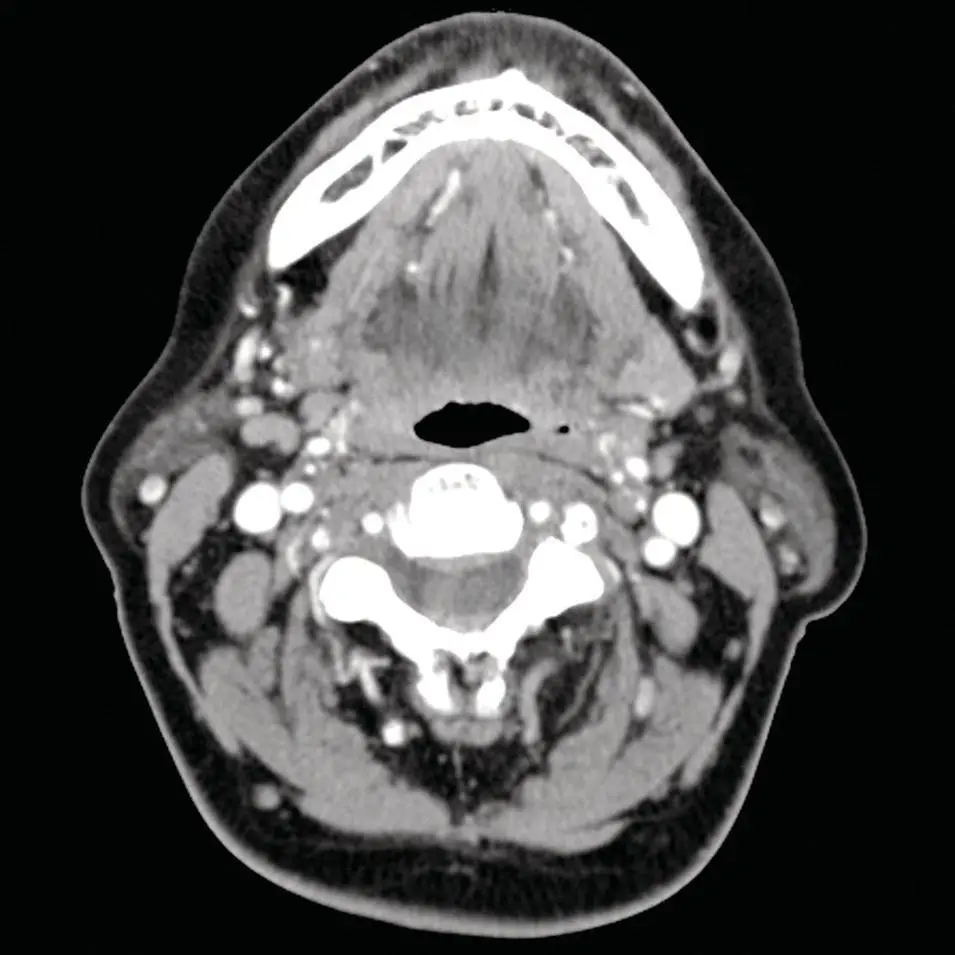
The sublingual gland (SLG) is the smallest of the major salivary glands and is the least likely to be involved with pathology. The SLG measures an approximately 3.5 cm in oblique AP, 1.0 cm in oblique LR, and 1.5 cm in SI dimensions. Anatomically, the SLGs exist in the floor of mouth and lie on the superior surface of the mylohyoid muscle, bordered anteriorly and laterally by the mandible, and medially by the submandibular duct, genioglossus muscle, and geniohyoid muscle. The submandibular gland serves as its posterior border ( Figures 2.44through 2.46). The sublingual gland communicates with the oral cavity via multiple small ducts (ducts of Rivinus) opening into the floor of mouth adjacent to the sublingual papilla. These small ducts may be fused and form a larger single duct (duct of Bartholin) and empty into the submandibular duct (Beale and Madani 2006).
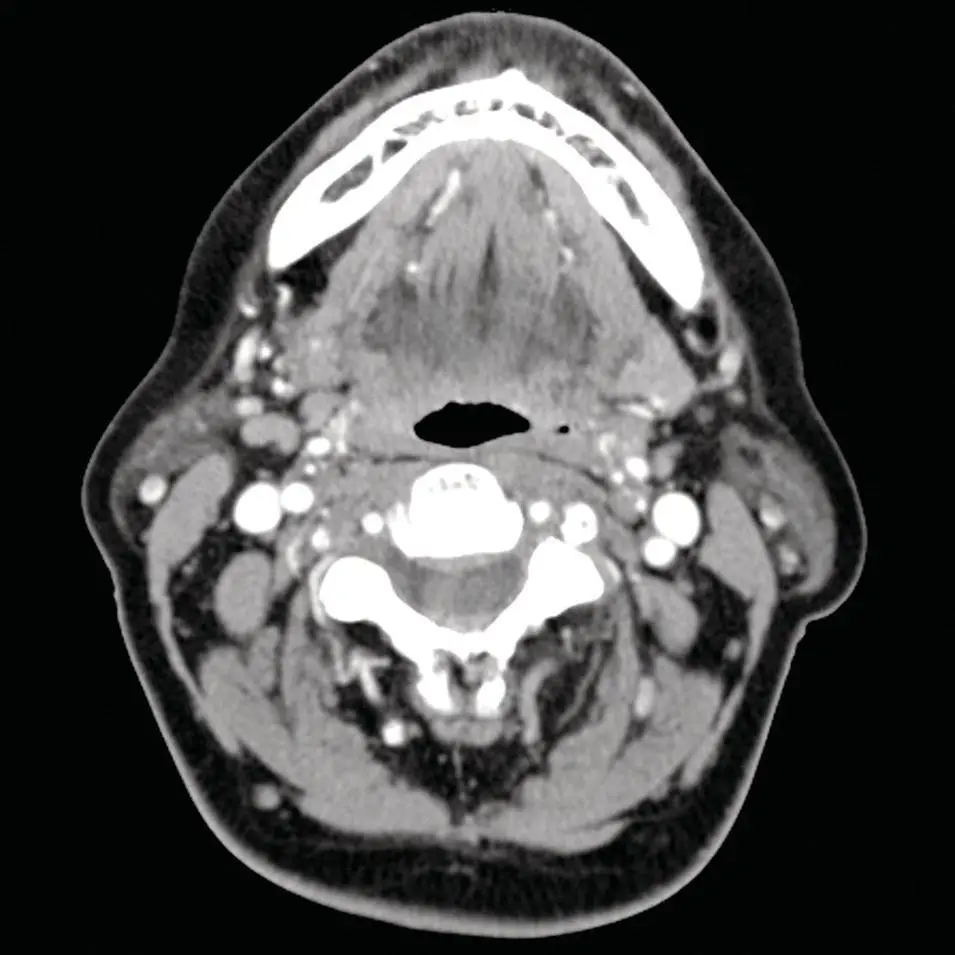
Figure 2.44. Axial CT of the neck at the level of the sublingual gland demonstrating mild normal enhancement along the lateral floor of mouth.
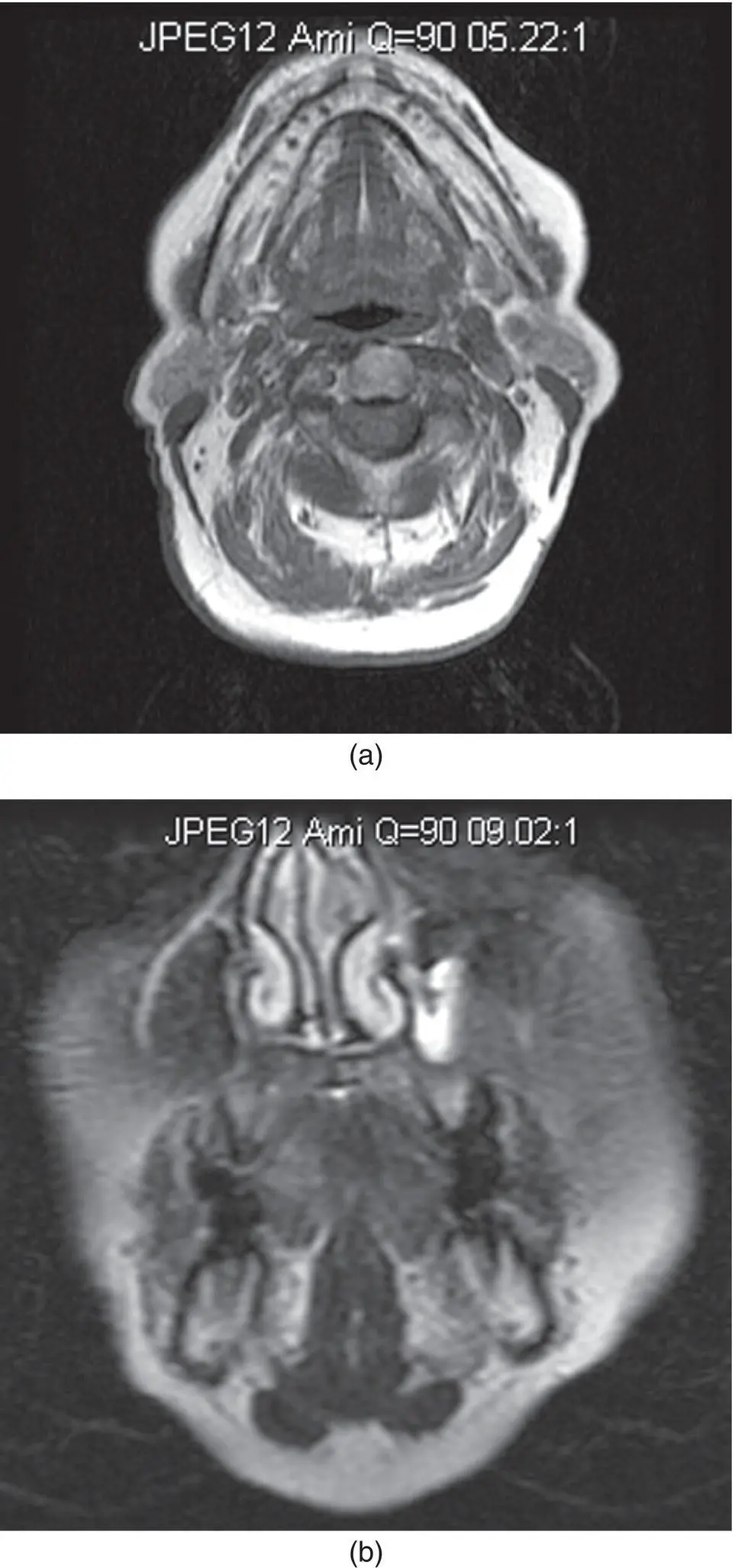
Figure 2.45.Axial contrast‐enhanced T1 MRI of the sublingual gland demonstrating enhancement (a). Note the deep lobe of the submandibular glands seen at the posterior margin of the sublingual glands. Coronal T2 weighted image demonstrating the sublingual gland “cradled” between the mandible laterally, the genioglossus muscle medially, the geniohyoid muscle inferomedially, and the combined mylohyoid and digastric muscles inferiorly (b).
Figure 2.46. Axial PET of the sublingual gland demonstrating the intense uptake seen in the sublingual glands bilaterally medial to the mandible (photopenic linear regions).
The SLG can be seen by CT and MRI and is similar in appearance to the SMG, although smaller (Sumi et al. 1999a). FDG uptake is less well defined since it is small and closely approximated to adjacent skeletal muscle, but the uptake is moderate.
Occasionally, accessory salivary tissue is found in the SMS along the anterior aspect (anterior to the normal submandibular gland). This is caused by herniation of sublingual gland through defects in the mylohyoid muscle, called a mylohyoid boutonniere, which typically occurs between the anterior and posterior parts of the mylohyoid muscle. The accessory gland may be accompanied by sublingual branches of the facial artery and vein. Although the accessory tissue may mimic a tumor, this should be readily identified as normal since the accessory tissue has the same characteristics on CT and MRI as normal sublingual or submandibular gland (White et al. 2001; Hopp et al. 2004).
The minor salivary glands are unevenly distributed throughout the upper aerodigestive tract and are submucosal in location. They are more concentrated in the oral mucosa where they inhabit the mucosa of the hard and soft palate, buccal mucosa, floor of mouth, as well as the mucosa of the lips, gingiva, and tongue. They are also found in the pharynx (nasal and oral), sinonasal spaces, larynx, trachea, and bronchi. Functionally, they are either mucinous (predominantly in the palatal mucosa) or mixed seromucinous glands. The serous minor salivary glands are found only on the tongue at the circumvallate papilla. The minor salivary glands do not have large defined ducts but do contain multiple small excretory ducts. MRI of minor salivary glands has been achieved with high‐resolution surface coils of the upper and lower lips. Patients with Sjogren disease had smaller gland area relative to normal, best demonstrated in the upper lip (Sumi et al. 2007).
Читать дальше