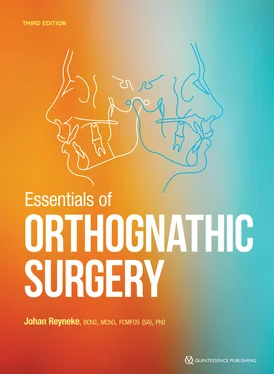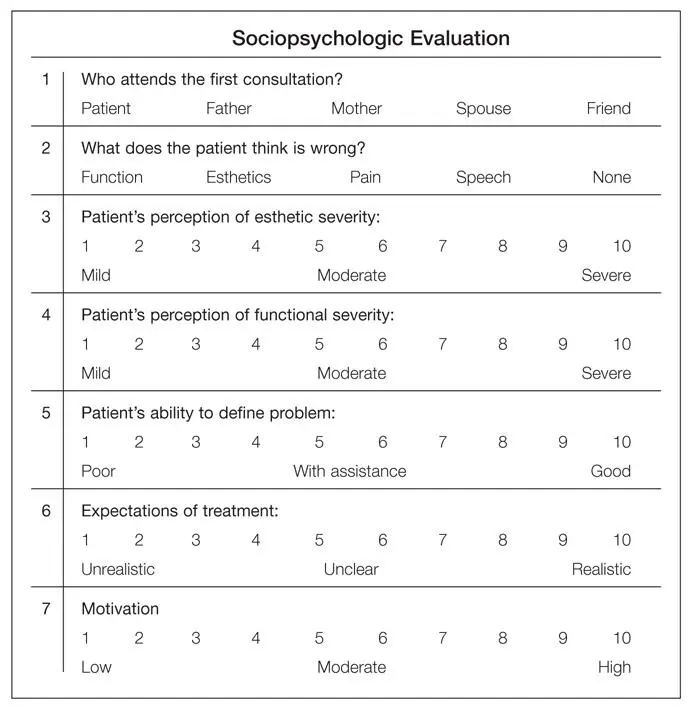
Fig 2-1Sociopsychologic evaluation form.
Esthetic Facial Evaluation
The clinical assessment of the face is probably the most valuable of all diagnostic procedures. The esthetic facial evaluation should be performed in a systematic fashion with the patient standing or seated comfortably. Primary emphasis should be placed on frontal esthetics because that is how people see themselves. Data should be recorded on a special form that can also serve as a checklist. Only abnormal and pertinent data should be recorded. Balance and proportion between the various facial structures in the individual are more important than numeric values. It is also important to compare the facial proportions with the patient’s general build and posture (ie, corporofacial relationship).
The clinical examination of the face should always be done with two questions in mind:
1 Would orthodontic-surgical treatment be able to correct the dental, skeletal, and soft tissue structure diagnosed as abnormal?
2 How would the orthodontic-surgical correction of the abnormal structures influence the facial structures considered to be normal?
It is often possible to correct the malocclusion of patients with dentofacial deformities by means of compromised orthodontic treatment , meaning an orthodontic-dental compromise for a skeletal jaw discrepancy resulting in an acceptable long-term functional and stable occlusion and facial esthetics. The fear of surgery, financial issues, unsatisfactory surgical experience of the orthodontist, and feasibility of correction by compromised orthodontic treatment will influence the orthodontist to implement orthodontic treatment for a skeletal deformity.
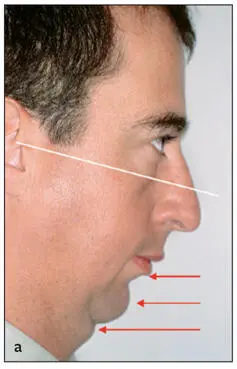
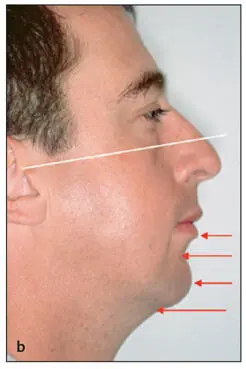
The patient should be examined in natural head posture, with the teeth in centric occlusion and the lips relaxed. Natural head posture is the position in which the patient orients his or her head and that feels most natural. Figure 2-2 illustrates the profound effect a change in head posture may have, for example, on chin position, chin-throat angle, and chin-throat length. Skeletal and soft tissue changes can therefore only be planned with the head in natural posture and the lips relaxed to ensure appropriate soft tissue changes. Orthodontic and surgical treatment are planned to produce ideal function in centric occlusion. All examination data should therefore be recorded in centric occlusion. However, patients with vertical maxillary deficiency and severely closed bites are an exception to this rule. Because of the inadequate height of the maxilla, these patients’ bites are overclosed, leading to distortion of their lips. To accurately evaluate these patients’ lips and maxillary incisor–upper lip relationships, they should be evaluated in an open bite posture. A wax bite can be placed between the teeth to increase the vertical dimension until the lips just part. The lack of tooth exposure, lip shape and thickness, anteroposterior position of the chin, labiomental fold, upper lip length, nasolabial angle, and soft tissue thickness can now be assessed more meaningfully. Figure 2-3 illustrates the profound changes in soft tissue characteristics in a patient with vertical maxillary deficiency in centric relation and in the open bite position.
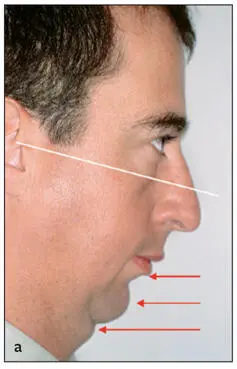
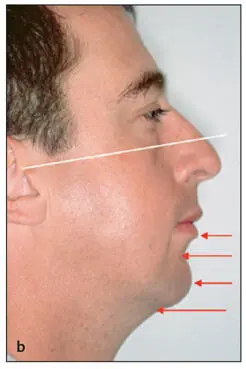
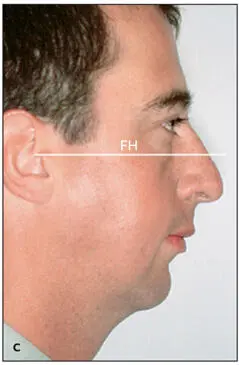
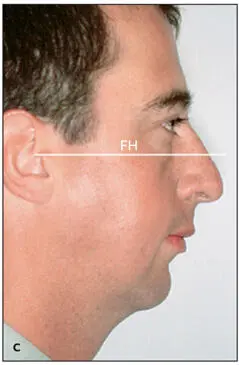
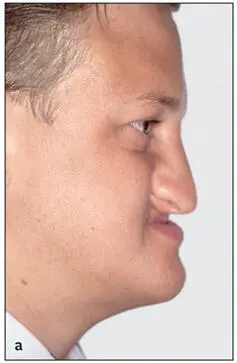
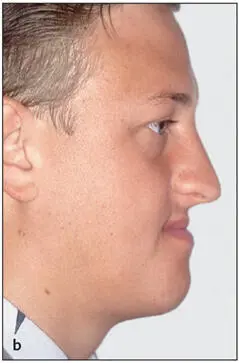
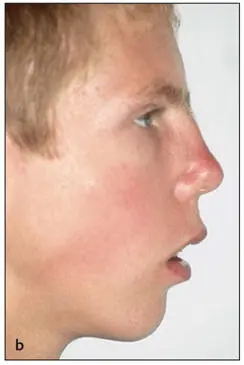
Fig 2-2Clinical assessment of the chin and throat area is possible only when the head is in natural posture. Note the differences with the head tilted down (a) , tilted up (b) , and with the head in natural posture (c) . The white line represents the Frankfort horizontal (FH) plane.
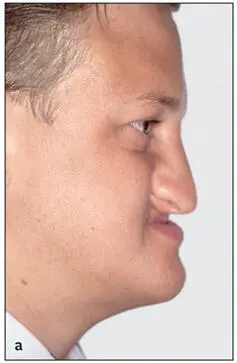
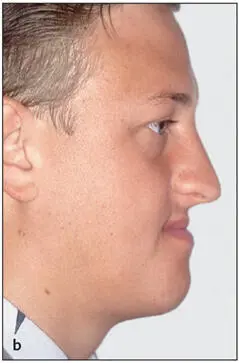
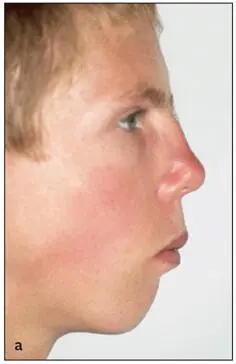
Fig 2-3Individual with vertical maxillary deficiency. Note the change in the shape of the lips and lower facial height with the teeth in occlusion (a) and with the mandible rotated open until the lips just part (b) .
It is imperative that the patient be examined with the lips in a relaxed position, because it is impossible to assess the relationship between the soft tissue and the hard tissue when the lips are forced together. Figure 2-4 demonstrates the effect of muscular compensation on the lips and chin. Note the change in the interlabial gap, labiomental fold, chin and lip shape, and maxillary tooth exposure. The sella-nasion (S-N) plane and Frankfort horizontal (FH) plane have traditionally been used as horizontal planes of reference for various cephalometric and clinical assessments. However, patients do not carry their heads with the S-N or FH planes parallel to the floor. Cephalometric landmarks should not dictate head posture used for facial assessment and treatment planning. The clinical evaluation should therefore be carried out with the head in the natural posture.
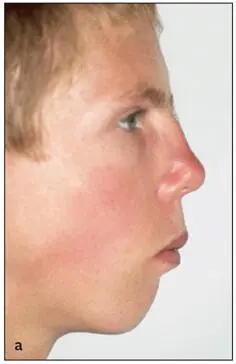
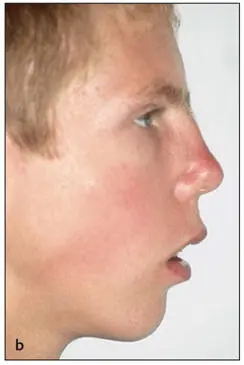
Fig 2-4The profile of the lower third is profoundly different when the lips are forced together (a) versus in repose (b) .
Frontal analysis
From the frontal view, it is particularly important to assess facial form; transverse dimensions; facial symmetry; the vertical relationship in the upper, middle, and lower thirds of the face; the lips; and the nose.
Facial form
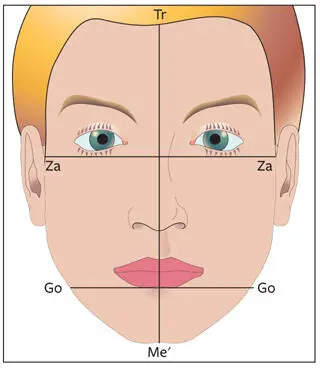
The relationship between the facial width and vertical height has a strong influence on facial harmony. Facial form and harmony should also be correlated with the patient’s overall body build. When correcting facial form, the overall body build of the individual should be considered (ie, short and stocky versus long and thin). The height-to-width proportion of the face is 1.3:1 for females and 1.35:1 for males. The bigonial width should be approximately 30% less than the bizygomatic dimension (Fig 2-5). Short, square facial types are often associated with a Class II deep bite malocclusion, vertical maxillary deficiency, masseteric hyperplasia, and macrogenia, whereas long, narrow facial types are often associated with vertical maxillary excess, a narrow nose, mandibular anteroposterior deficiency, microgenia, a high palatal vault, and an anterior open bite malocclusion (Figs 2-6 and 2-7; Table 2-1).
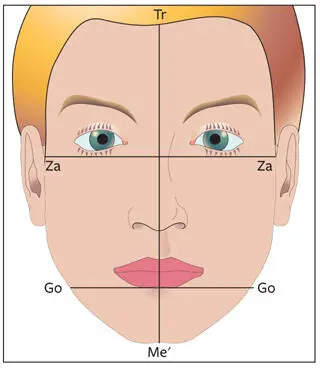
Fig 2-5Facial form. The facial height (trichion [Tr]–soft tissue menton [Me′]):bizygomatic width (Za-Za) should be 1.3:1 (females) and 1.35:1 (males). The bigonial width (Go-Go) should be approximately 30% less than the bizygomatic width.
Читать дальше