however, some license is taken with respect to forebrain, which here refers to the prosencephalon plus diencephalon, as clinically, lesions in these collective regions generally present the same syndromes. It is important to recognize these various areas when sending brain sections for histopathologic examination.
Structurally, the forebrain (prosencephalon) is composed of the cerebral hemispheres (most of the telencephalon), thalamus and hypothalamus (diencephalon), hippocampus, basal nuclei, and the limbic system, all situated in the rostral fossa of the neurocranium. The middle fossa contains the midbrain (mesencephalon). Caudally, the hindbrain (rhombencephalon) is composed of the cerebellum and pons (together with the metencephalon) and the medulla oblongata (myelencephalon) that all reside in the caudal fossa. Both the cerebrum (cerebro) and cerebellum (cerebello) have their own outer (cortical) and inner (medullary) portions, composed particularly of gray matter (neuronal cell bodies) and white matter (neuronal fibers), respectively. The remainder of the brain comprising the midbrain, pons, and medulla oblongata makes up the brainstem. This contains white matter pathways passing to and from brain and spinal cord regions, and gray matter, mostly contained in nuclei as relay centers and sensory and motor nuclear areas for the body, including the cranial nerve nuclei.
The spinal cord is the conduit between the brain and the peripheral spinal (non‐cranial) nerves and their innervated structures of the body. Thus, it contains all the afferent and efferent neuronal fibers connecting to and from the brain as superficial white matter tracts. It has a cervicothoracic (brachial) enlargement (intumescence) and a lumbosacral (pelvic) enlargement at the levels of the thoracic and the pelvic limbs, respectively. These swellings are the result of a higher density of neuronal cell bodies at these sites, collected in the butterfly‐shaped, central gray matter and supplying the sensory and motor spinal nerves for the limbs.
To avoid some confusion, vertebral levels are labeled as C7, T3, L4, S5, Ca6 (caudalis as opposed to coccygeal), etc ., and spinal cord segments are labeled as C 8, T 3, L 4, S 5, Ca 6, etc .
Clinically, the autonomic nervous system functions independently and involuntarily from the rest of the nervous system, receiving afferent input from the environment via the basic and special senses to maintain the body’s internal milieu. The parasympathetic component has a brainstem and sacral outflow to the head and body, whereas the sympathetic component has a thoracolumbar outflow.
The entire CNS is protected within the bony neurocranium of the head and in the vertebral canal within the vertebral column. It is covered by meninges consisting of the thick (pachy) dura mater and thin (lepto) arachnoid and pia mater. Between the latter two membranes, is cerebrospinal fluid (CSF), produced by the choroid plexuses of the lateral and fourth ventricles. This fluid also fills the cavities within the brain (ventricles) and spinal cord (spinal canal), which are lined by ciliated ependymal cells.
Because we refer to vertebral structures very often, it is worth reviewing the recommended correct nomenclature as in Nomina Anatomica Veterinaria http://www.wava‐amav.org/wava‐documents.html
Columna Vertebralis
Corpus vertebrae
Extremitas cranialis (Caput vertebrae)
Extremitas caudalis (Fossa vertebrae)
Crista ventralis
Arcus vertebrae
Pediculus arcus vertebrae
Lamina arcus vertebrae
Foramen vertebrale
Canalis vertebralis
Spatium interarcuale
Foramen intervertebrale
Incisura vertebralis cranialis
Incisura vertebralis caudalis
Foramen vertebrale laterale
Sulcus n. spinalis
Processus spinosus
Processus transversus
Processus costalis
Processus articularis cranialis
Processus articularis caudalis
Processus accessorius
As well as meningeal cells, ependymal cells, neurons (somata and their axons and dendrites), and blood vessels, several other types of supporting, protective, and nutritive glial (glue) cells (neuroglia) make up a large part of the volume of the CNS. The largest of these glial cells are the astrocytes with their star‐shaped processes. These cells basically act to support the CNS, which has little cytoskeletal framework. They also act as pseudofibroblasts and can lay down collagen in response to injury to the CNS. Originally, the processes of other small glial cell types were thought to be few (oligo); these cells being named oligodendrocytes. We now know that their processes are extensive and extend to and maintain all the myelin sheaths covering CNS axons. The small microglial cells appear to be the tissue macrophages of the mononuclear phagocytic system within the CNS, responding along with migrating inflammatory cells from the circulation when there are inflammatory processes occurring in CNS tissues.
The neuronal processes in the peripheral nervous system (PNS) with their myelin sheaths are called nerve fibers and make up the nerve roots, nerve plexuses, and peripheral nerves. Some neurons, particularly those in the autonomic nervous system and the sensory neurons, have their cell bodies in aggregations known as ganglia. Also, several networks of interwoven nerves (plexuses) occur in the PNS, the largest of which are the brachial plexus supplying the thoracic limbs and the lumbosacral plexus for the pelvic limbs.
The cells that ensheathe PNS nerve fibers are Schwann cells. These assist in maintaining a framework for nerves, as well as producing the abutting layers of myelin that surround all the larger fibers, allowing quite rapid saltatory (leaping, jumping) conduction of electrical impulses. The PNS has a fibrous connective tissue cytoskeleton that consists of the epineurium that wraps around a whole nerve, the perineurium that surrounds a bundle or fascicle of fibers, and the endoneurium that separates the individual nerve fibers.
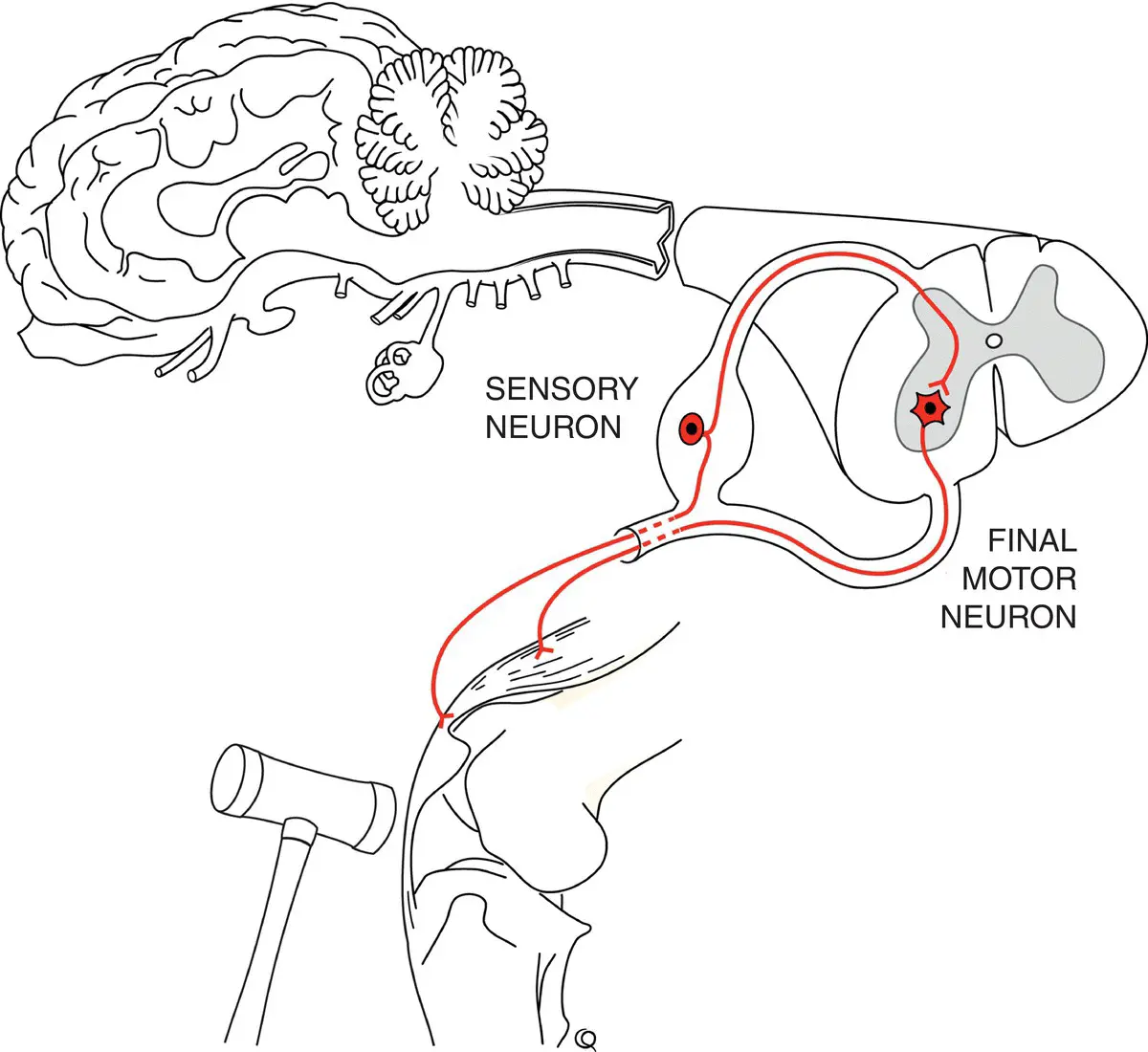
Probably the most important structural and functional unit of the nervous system is the simple reflex pathway ( Figure 1.2). A neurologic examination basically involves testing simple and complex reflex pathways and interpreting the effected reflex activity and complex responses (see Chapter 2, Neurologic Evaluation).
A simple spinal reflex pathway, depicted as a patellar tendon reflex in Figure 1.2, is composed of two neurons. Stimulation of a sensory stretch receptor in a tendon with its sensory neuronal cell body in the dorsal root ganglion stimulates an efferent motor neuron. These motor neurons are usually alpha motor neurons and are collectively referred to as final motor neurons, having their cell bodies in the ventral gray matter of the spinal cord (and in cranial nerve nuclei in the brainstem). Reflex motor responses to sensory stimuli will occur without any other afferent or efferent connections within the CNS; so long as these two (or more) neurons comprising the reflex arc, as well as the sensory nerve ending, the neuromuscular junction, and the effector muscle, all are intact. In contrast, lesions, due to any cause, that damage parts of the reflex pathway will suppress those reflexes. Indeed, if the damage is to the alpha motor neurons in the ventral gray matter of the spinal cord or the cranial nerve motor nuclei, or to their peripheral axons, there will be loss of reflexes and severe weakness and ultimate muscle atrophy, i.e ., signs of a final motor neuron lesion.
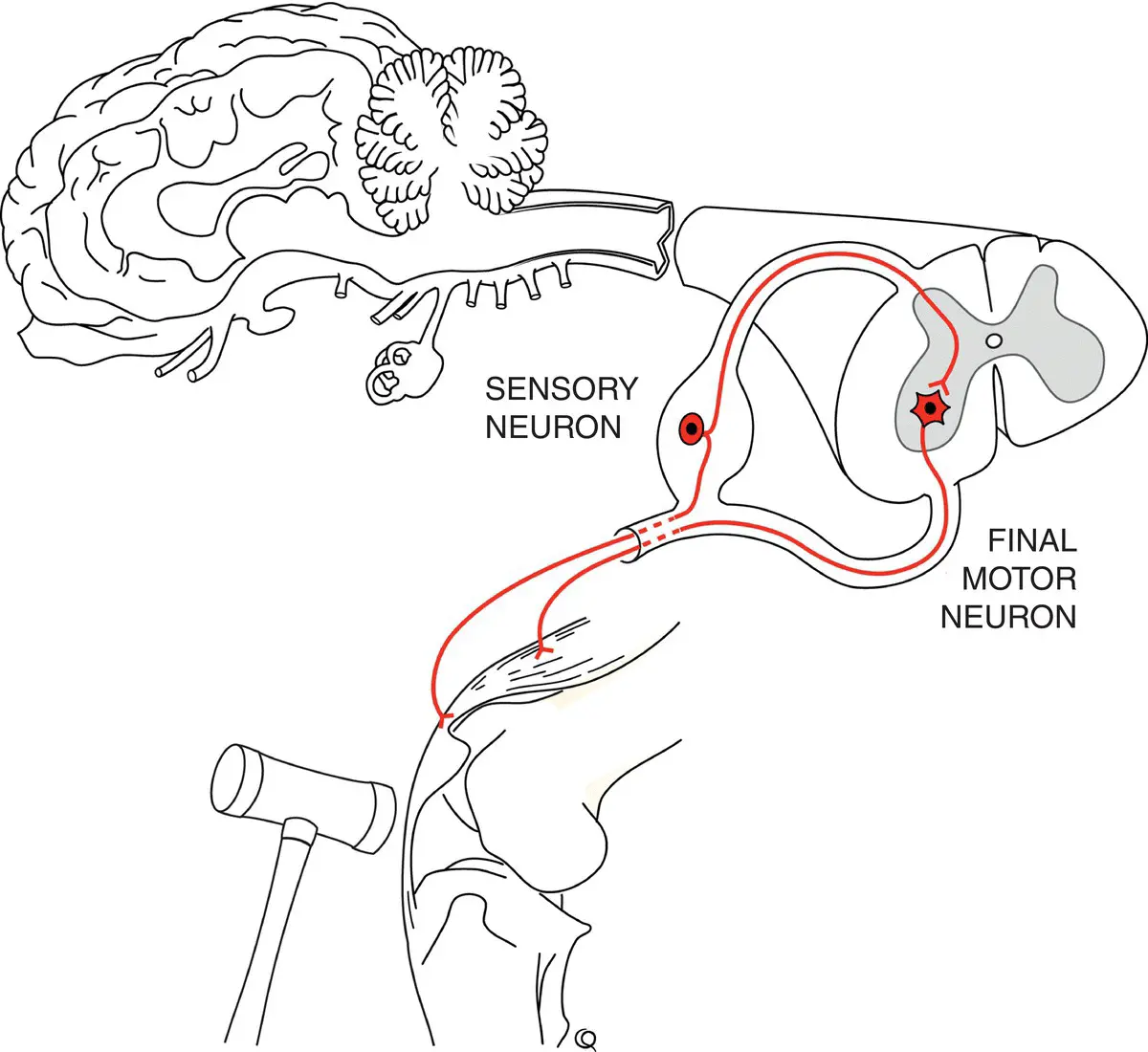
Figure 1.2 Basic monosynaptic spinal reflex pathway (patellar reflex) showing the sensory neuron synapsing on the final motor neuron. In many other reflex pathways, there is at least one internuncial neuron within the CNS allowing further modulation of the reflex.
Читать дальше