In the early phase of irritative lesions such as bacterial meningitis, viral meningoencephalitis, neuritis, and focal trauma involving the facial nerve, facial muscles can twitch and even remain in spasm prior to paresis or paralysis that may ensue. True, permanent hemifacial spasm with constant contraction of facial muscles, that relaxes following facial nerve anesthesia or general anesthesia as seen in humans and dogs does not yet appear to be recorded in large animals. This might be expected to occur following recovery from bacterial otitis media. As occurs in many other regional muscle groups, 18facial muscles are occasionally seen to undergo repetitive contraction described as facial tic or myoclonus. Some of these syndromes wax and wane, and one facial tic in a horse has been seen to become almost violent when hypocalcemia associated with systemic illness occurred, to then quieten with IV calcium treatment. The underlying cause for facial and other localized myoclonia is notoriously not found. 18–20
Brainstem auditory evoked potential recordings may be used as proxy for facial nerve function as the facial nerve is intimate with the vestibulocochlear nerve for their course in the region of the temporal bone and its middle and inner ear compartments. 21,22
1 1 Espinosa P, Nieto JE, Estell KE, Kass PH and Aleman M. Outcomes after medical and surgical interventions in horses with temporohyoid osteoarthropathy. Equine Vet J 2017; 49(6): 770–775.
2 2 Walker AM, Sellon DC, Cornelisse CJ, et al. Temporohyoid osteoarthropathy in 33 horses (1993–2000). J Vet Intern Med 2002; 16(6): 697–703.
3 3 Myrna KE. Neuro‐ophthalmology in the Horse. Vet Clin North Am Equine Pract 2017; 33(3): 541–549.
4 4 de Lahunta A, Glass E and Kent M. Veterinary Neuroanatomy and Clinical Neurology. 4th ed. Saunders, Elsevier, St. Louis, MO. 2015.
5 5 Gosselin VB, Francoz D, Babkine M, et al. A retrospective study of 29 cases of otitis media/interna in dairy calves. Can Vet J 2012; 53(9): 957–962.
6 6 Lamm CG, Munson L, Thurmond MC, Barr BC and George LW. Mycoplasma otitis in California calves. J Vet Diagn Invest 2004; 16(5): 397–402.
7 7 Francoz D, Fecteau G, Desrochers A and Fortin M. Otitis media in dairy calves: a retrospective study of 15 cases (1987 to 2002). Can Vet J 2004; 45(8): 661–666.
8 8 Katz L. Left otitis media/interna and right maxillary sinusitis in a Percheron mare. Vet Clin North Am Equine Pract 2006; 22(1): 163–175.
9 9 Ragle CA. Head Trauma. Vet Clin North Am Equine Pract 1993; 9(1): 171–183.
10 10 Vatistas N and Mayhew IG. Differential diagnosis of polyneuritis equi. In Practice 1995; 17: 26–29.
11 11 Vatistas NJ, Mayhew IG and Whitwell KE. Polyneuritis equi: a clinical review incorporating a case report of a horse displaying unconventional signs. Prog Vet Neurol 1991; 2: 67–72.
12 12 Johnstone LK, Engiles JB, Aceto H, et al. Retrospective evaluation of horses diagnosed with neuroborreliosis on postmortem examination: 16 cases (2004–2015). J Vet Intern Med 2016; 30(4): 1305–1312.
13 13 Jensen R, Maki LR, Lauerman LH, et al. Cause and pathogenesis of middle ear infection in young feedlot cattle. J Am Vet Med Assoc 1983; 182(9): 967–972.
14 14 Maenhout D, Ducatelle R, Coussement W, et al. Space occupying lesions of cranial nerves in calves with facial paralysis. Vet Rec 1984; 115(16): 407–410.
15 15 Van der Lugt JJ and Jordaan P. Facial paralysis associated with space occupying lesions of cranial nerves in calves. Vet Rec 1994; 134(22): 579–580.
16 16 McFadden AM, Mackereth GF, Avery MI, et al. A syndrome of facial paralysis of dairy calves in the Franklin district of New Zealand. N Z Vet J 2009; 57(1): 63–68.
17 17 Torre F. Use of autogenous cartilage graft from auricular cartilage in treatment of unilateral paralysis of nostril in racing standardbred horse. Equine Vet Educ 2003; 15(1): 10–14.
18 18 Beech J. Forelimb tic in a horse. J Am Vet Med Assoc 1982; 180(3): 258–260.
19 19 de Lahunta A, Glass EN and Kent M. Classifying involuntary muscle contractions. Comp Cont Ed Pract Vet 2006; 28: 516–529.
20 20 Kerby MJ. Repetitive facial nerve stimulation in a cow. Vet Rec 2006; 158(12): 420.
21 21 Wrzosek M, Niezwiedz A, Giza E, Borowicz H and Nicpon J. Auditory brainstem evoked response (BAER) in the diagnosis of nervous system diseases in horses. Medycyna Weterynaryjna 2012; 68(9): 557–561.
22 22 Aleman M, Puchalski SM, Williams DC, Kass PH and Holliday TA. Brainstem auditory‐evoked responses in horses with temporohyoid osteoarthropathy. J Vet Intern Med 2008; 22(5): 1196–1202.
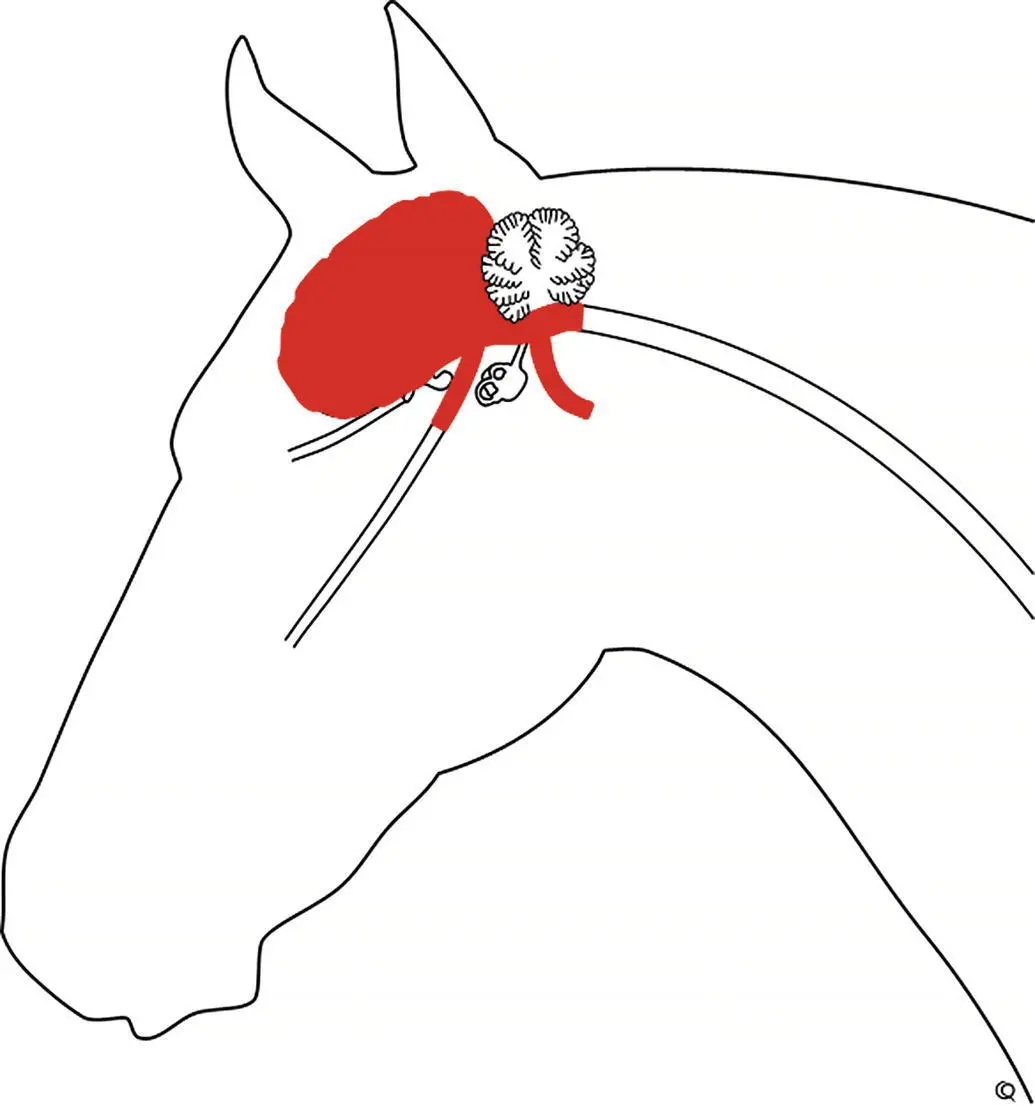
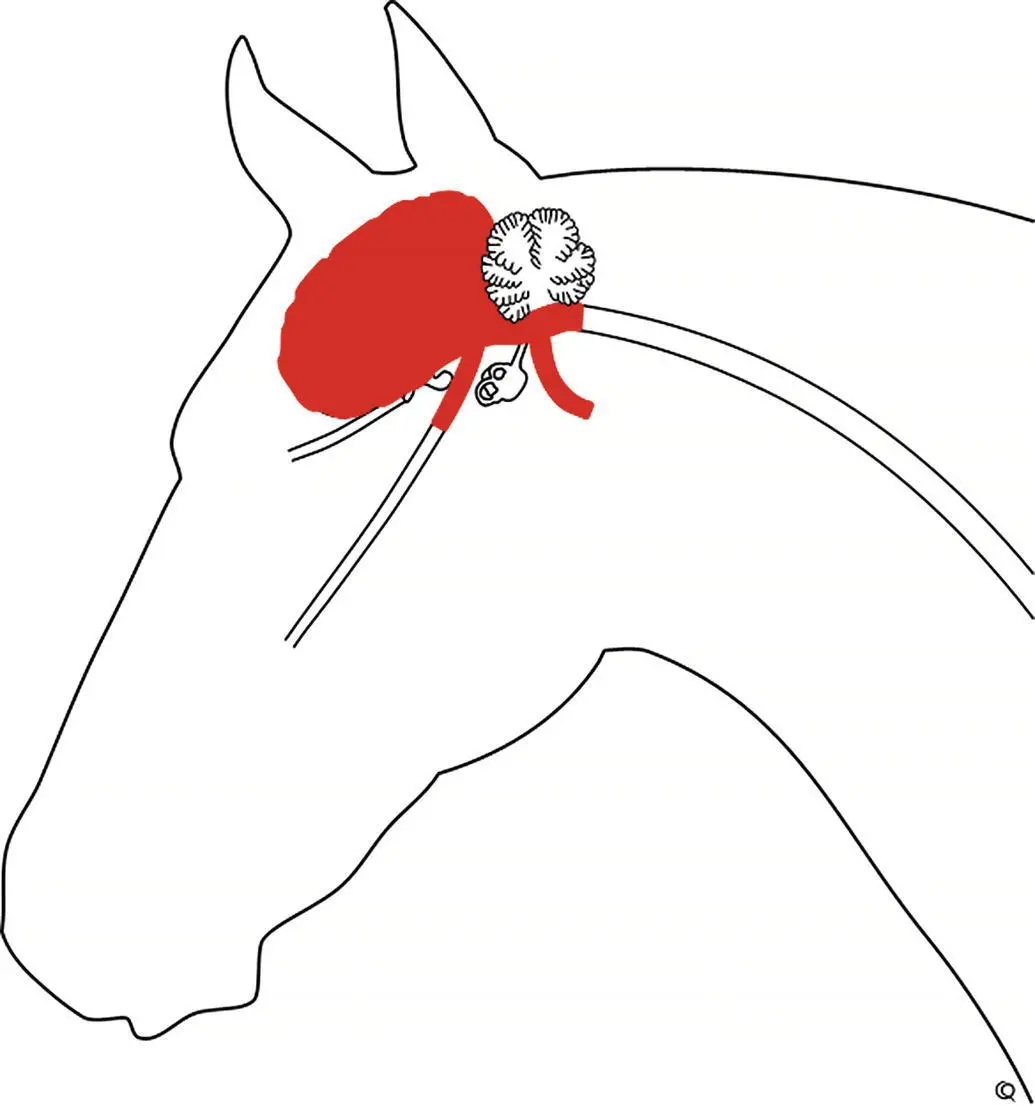
Dysphagia is a frequently occurring neurologic sign in preterm and neonatal infants 1and in large animals ( Figure 15.1). It is reported to occur in newborn foals 2at a frequency of ~1% and has been reported to occur in ~5% of foals admitted to an equine hospital neonatal ICU. 3The term dysphagia is used here in its broadest sense to mean difficulty in eating or drinking and includes disorders of prehension, mastication, and deglutition. Central control of eating is mostly by specific medullary centers and their afferent and efferent pathways in the following nerves (and their innervated structures): trigeminal (CN V‐ muscles of mastication and facial sensation); facial (CN VII‐ muscles of the lips and cheeks); glossopharyngeal, vagus, and accessory (CNs IX, X and XI‐ pharynx, and larynx); and hypoglossal (CN Xll‐ tongue). The voluntary effort in eating and drinking probably is initiated in the cerebral motor cortex and in basal nuclei. Therefore, disorders of the cerebrum, thalamus, medulla oblongata, and cranial nerves V, VII, IX, X and XII can cause dysphagia.
Physical damage to the naso‐ and oro‐pharynx, and the larynx, can result in food accumulating in the pharynx and airway with resultant nasal or oral food discharge. This includes postoperative complications resulting from various laryngeal surgical procedures, especially prosthetic laryngoplasty 4–6and from pharyngeal trauma in cattle. 7
Development of fully competent swallowing reflexes appear to occur late in gestation, and preterm human infants often have swallowing difficulties that with time most often improve or resolve. 1Newborn foals with apparent pharyngeal dysphagia most often also go on to resolve this problem. 3
Passing a stomach tube, inspecting teeth, auscultating the thorax for evidence of feed inhalation, taking appropriate radiographs, and using an endoscope to see the pharynx and larynx and the structures surrounding the guttural pouches are helpful ancillary aids. In particular, this should exclude many of the most common non‐neurologic causes of dysphagia including dental problems, esophageal choke, pharyngitis, oropharyngeal foreign body, pharyngeal abscess, or phlegmon and neoplastic masses. 4, 8When evaluating animals from rabies‐endemic regions that have had signs of dysphagia for less than 2 weeks, consideration must be given to this possibility early during evaluation.
Forebrain diseases do not cause actual paralysis of the muscles involved in eating but can impair voluntary control of these muscles, resulting in uncoordinated, dystonic, and weak movements of the face, tongue, mouth, and pharynx. Diffuse cerebral disease can cause dysphagia in addition to lack of ability to find or eat food due to other gross behavioral and attitudinal abnormalities such as mental obtundation, head pressing, circling, and blindness. Characteristically, there is some weakness and protrusion of the tongue, drooping of the lower lip, and drooling of saliva. Unweaned patients lose the suckling reflex. Included in these diffuse diseases are the arboviral encephalitides, rabies, hepatoencephalopathy, diffuse meningitis, neonatal encephalopathy, head trauma with brain swelling, leukoencephalomalacia, and hydrocephalus.
Читать дальше