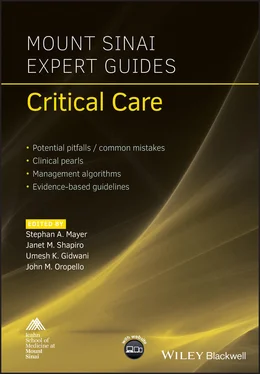
Mount Sinai Expert Guides
Здесь есть возможность читать онлайн «Mount Sinai Expert Guides» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Mount Sinai Expert Guides
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Mount Sinai Expert Guides: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Mount Sinai Expert Guides»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Mount Sinai Expert Guides — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Mount Sinai Expert Guides», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Side effects:Vasodilation and hypotension.Myocardial depression.Respiratory depression.Pancreatitis.Propofol infusion syndrome:A potentially lethal syndrome marked by metabolic acidosis, hypertriglyceridemia, and hypotension refractory to vasopressors.Believed due to mitochondrial dysfunction.Treatment is cessation of infusion and supportive.Associated with prolonged infusions of greater than 70 μg/kg/min.Incidence of propofol infusion syndrome 1%, mortality 33%.
Recommended doses:Bolus: 0.1–0.3 mg/kg slowly.Infusion: 5–50 μg/kg/min.
Dexmedetomidine
Pharmacology:Alpha‐2 receptor agonist.Minimal respiratory depression.Hypnotic and analgesic properties.No active metabolites.Onset of action after loading dose 5–10 minutes.
Side effects:Hypertension: often associated with loading doses.Hypotension: often associated with loading doses.Bradycardia.
Recommended doses:Loading dose: 1 μg/kg over 10 minutes.
Infusion: FDA approved for 0.2–0.7 μg/kg/h for up to 24 hours; reports have shown safety with maximum infusion 1.5 μg/kg/h for up to 1 month.
Miscellaneous:No proven benefit to delirium.
Ketamine
Pharmacology:NMDA antagonist.Hypnotic and analgesic.Active metabolite norketamine.There should be no expectation of decreased opioid use or rates of delirium after a single intraoperative dose of ketamine.Onset of action 30–40 seconds.Elimination half‐life 2–3 hours.
Side effects:Increased salivation.Potential for increased intracranial pressure (ICP)Potential for sympathetic discharge.Hallucinations: can be attenuated by simultaneous administration of benzodiazepine.Negative inotropy: may be harmful in heart failure patients; further research is warranted.
Recommended doses:Bolus: 0.1–0.5 mg/kg IV.Infusion: 0.05–0.4 mg/kg/h.
Reading list
1 Barr J, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013; 41(1):263–306.
2 Devlin JW, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med 2018; 46:e825–73.
3 Joffe AM, McNulty B, Boitor M, Marsh R, Gélinas C. Validation of the critical‐care pain observation tool in brain‐injured critically ill adults. J Crit Care 2016; 36:76–80.
4 Khan BA, et al. Comparison and agreement between the Richmond Agitation‐Sedation Scale and the Riker Sedation‐Agitation Scale in evaluating patients’ eligibility for delirium assessment in the ICU. Chest 2012; 142(1):48–54.
5 Kotifs K, Zegan‐Baranska M, Szydlowski L, Zukowski M, Ely EW. Methods of pain assessment in adult intensive care unit patients – Polish version of CPOT (Critical Care Pain Observation Tool) and BPS (Behavioral Pain Scale). Anaesthesiol Intensive Ther 2017; 49(1):66–72.
6 Parker AM, Sricharoenchai T, Raparla S, Schneck KW, Bienvenu OJ, Needham DM. Posttraumatic stress disorder in critical illness survivors. Crit Care Med 2015; 43(5):1121–9.
7 Patanwala AE, Martin JR, Erstad BL. Ketamine for analgosedation in the intensive care unit: a systematic review. J Intensive Care Med 2017; 32(6):387–95.
8 Payen J, et al. Assessing pain in critically ill sedated patients by using a behavioral pain scale. Crit Care Med 2001; 29(12):2258–63.
9 Reade MC, et al. for the DahLIA Investigators and the Australian and New Zealand Intensive Care Society Clinical Trials Group. Effect of dexmedetomidine added to standard care on ventilator‐free time in patients with agitated delirium: a randomized clinical trial. JAMA 2016; 315(14):1460–8.
10 Turunen H, et al. Dexmedetomidine versus standard care sedation with propofol or midazolam in intensive care: an economic evaluation. Crit Care 2015; 19(1):67.
Additional material for this chapter can be found online at: www.wiley.com/go/mayer/mountsinai/criticalcare
This includes multiple choice questions. 
CHAPTER 3 Vascular Access
Jennifer Wang and John M. Oropello
Icahn School of Medicine at Mount Sinai, New York, NY, USA
OVERALL BOTTOM LINE
Providers need to optimize central venous catheter and arterial catheter insertion in critically ill patients.
Strict sterile technique during insertion is crucial for minimizing infection, the most serious and frequent complication associated with line placement.
In general, central venous and arterial lines should be removed as soon as possible to minimize the risk of infection.
Central venous access
Indications
Difficult venous access, frequent blood sampling.
Rapid administration of fluids and blood products (resuscitation).
Administration of fluids and medication caustic to small veins (e.g. vasopressors, chemotherapy, total parenteral nutrition).
Renal replacement therapy, plasmapheresis.
Transvenous pacemaker, pulmonary artery catheter.
Venous access sites
Internal jugular (IJ), subclavian medial (SM) or lateral (SL), and femoral (F) veins.
Catheter types ( Figure 3.1)
Multilumen or single lumen (central venous access catheters).
Dialysis (large bore, double, or multilumen catheters).
Introducer (large bore for rapid resuscitation access, temporary pacemaker, or pulmonary artery catheter insertion).
Procedure
Prior to procedure, ensure that the patient’s name, procedure, and site of insertion are confirmed with the patient’s nurse.
Pre‐procedure US: the vein is visualized under US when using the IJ, SL, or F veins for access. (Note: the SM vein approach places the needle tip under the clavicle, hence it is not possible to visualize cannulation of the subclavian vein under US when using this approach.) Scan above, at, and below site of planned insertion (or lateral to medial with SL approach) with compression to check for thrombosis ( Figure 3.2) or stenosis. Video 3.1 demonstrates the appearance of the vessels when performing the SL approach. On the viewer’s left, cephalad (towards the head, i.e. closer to the clavicle) is the subclavian artery (SA); to the viewer’s right, caudad (towards the feet, i.e. closer to the lung) is the subclavian vein (SV) (since the vessel has not yet passed the first rib, technically speaking it may be called the axillary vein). Note that the SV is compressible and non‐pulsating. Also note the twinkling horizontal line about 0.5 cm below the SV coming in from the right side with respiration: this is the pleural line.
For any neck line insertion (IJ or SM/SL sites) pre‐scan (US) the pleura on the side of planned insertion for the presence and degree of lung sliding. (See Chapter 4, Videos 4.1 and Video 4.2.) This can improve the accuracy of post‐procedure US to assess for pneumothorax.
Optimize site of insertion by selecting a plane where the artery is not directly beneath the vein (IJ insertion) or directly overlying the vein (F insertion) if possible. For IJ lines, turning the patient’s head toward the side of insertion may move the IJ to a more lateral position relative to the carotid artery. For F lines, moving the US superiorly toward the inguinal ligament will locate the vein medial to the artery. Moving the US down the leg (away from the inguinal ligament in the direction of the knee) will locate a position where the artery is overlying the vein, making access more difficult. Also, flexion of the lower extremity at the knee with lateral rotation may also help to move the femoral vein more medially from under the femoral artery. US will demonstrate whether this maneuver is effective or not.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Mount Sinai Expert Guides»
Представляем Вашему вниманию похожие книги на «Mount Sinai Expert Guides» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Mount Sinai Expert Guides» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.