Source: Reproduced with permission of Dr Gregory Lisciandro, Hill Country Veterinary Specialists and FASTVet.com, Spicewood, TX.
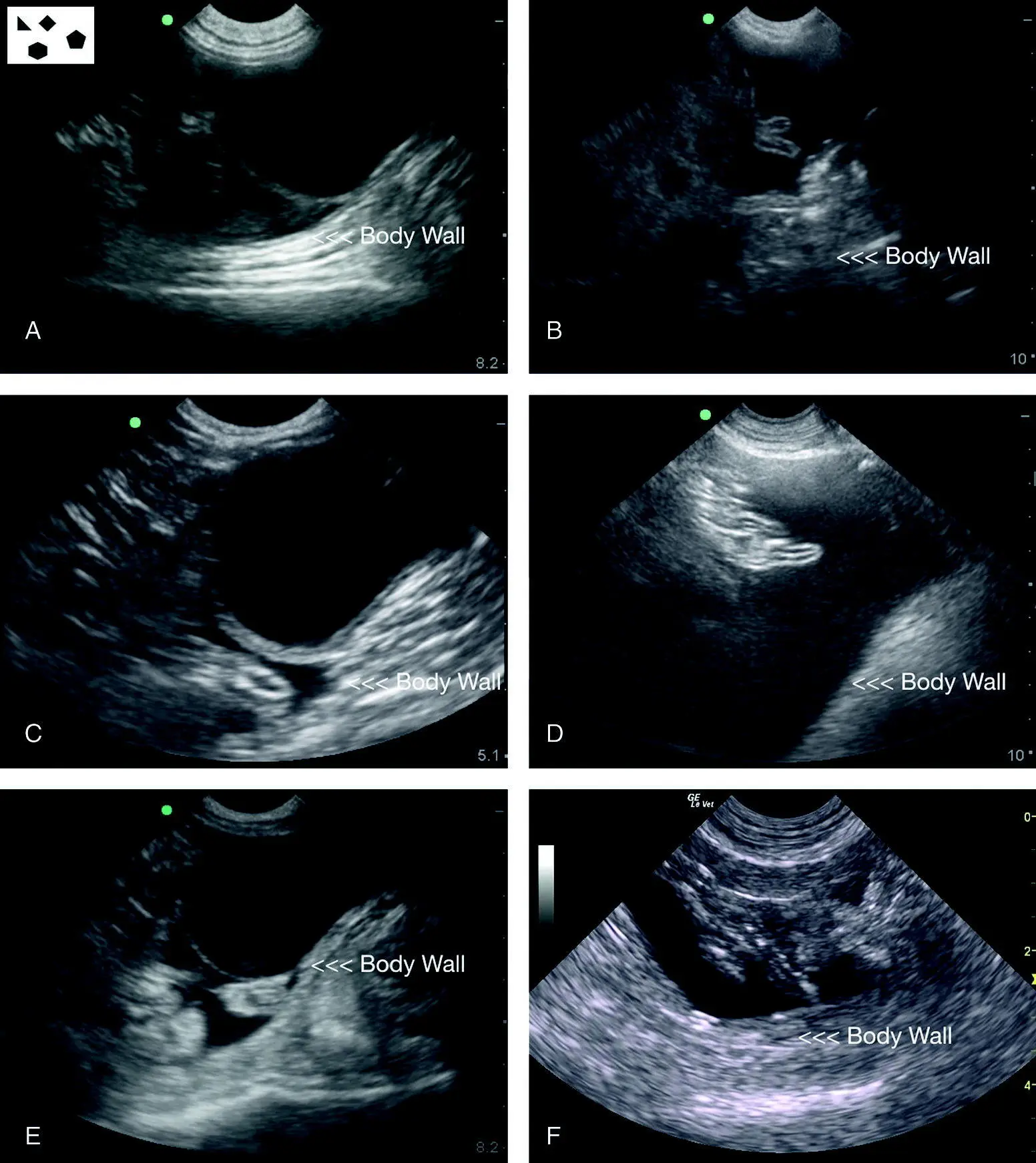
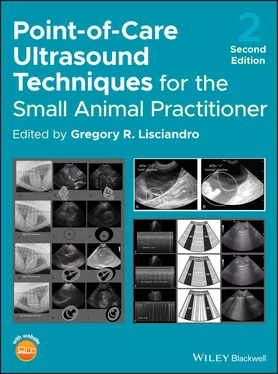
Figure 6.25. Examples of typical positive studies at the CC view. In (A), (C) and (E), CC view positives are shown with a urine‐filled urinary bladder in contrast to images in (B), (D) and (F) in which the urinary bladder is not readily apparent as in (B) or absent in (D) and (F). The urinary bladder is likely not ruptured, as most of these patients are nontrauma cases, and the probe could be slid caudally and/or directed toward the pubis to locate a small urinary bladder. In the absence of a urinary bladder, the serial AFAST examination post resuscitation is invaluable to determine the presence of the urinary bladder and urine production. Note the consistency in the images with their proportionality and location of the relevant CC view structures of the urinary bladder, “CC pouch”, and body wall.
Source: Reproduced with permission of Dr Gregory Lisciandro, Hill Country Veterinary Specialists and FASTVet.com, Spicewood, TX.
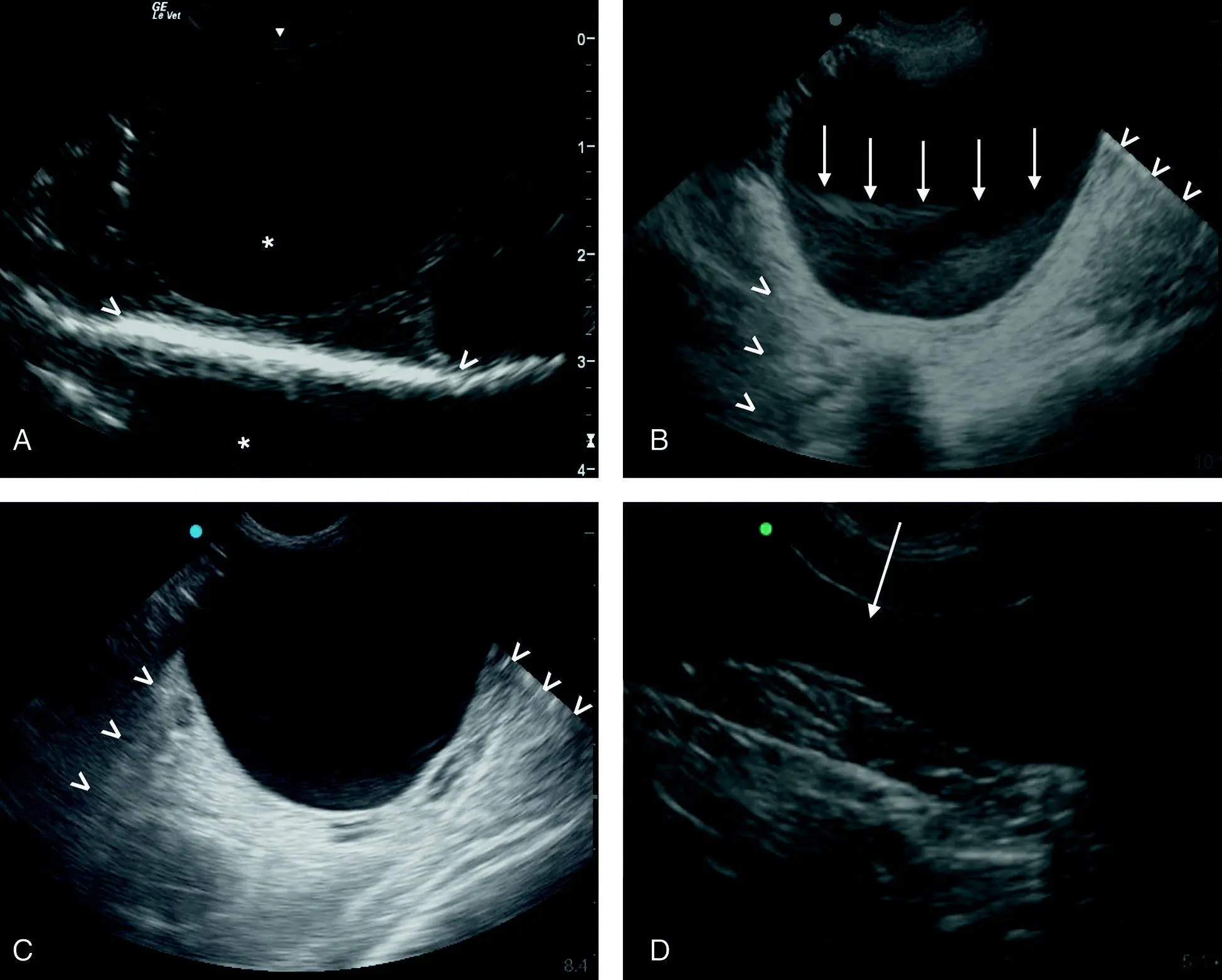
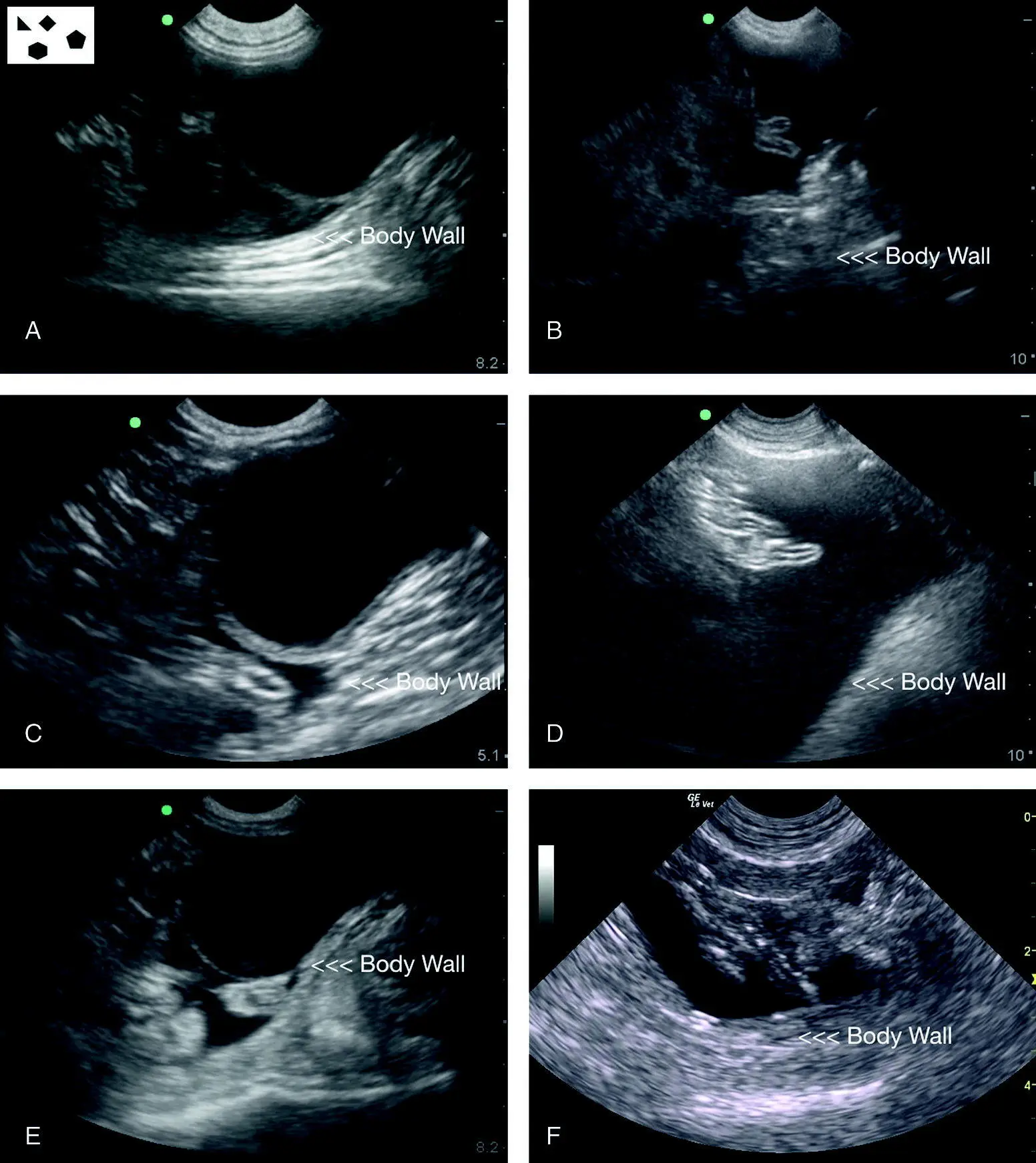
Figure 6.26. Relevant artifacts at the CC view. (A) A mirror image artifact is present beyond the body wall and marked with an asterisk (*). Placing the focus cursor in the center of the image and changing the angle of insonation can help eliminate mirror image. Acoustic enhancement artifact, the hyperechoic body wall, is also present through the fluid‐filled urinary bladder and its cranial and caudal borders marked (V). In (B) the acoustic enhancement artifact is again marked (V). The arrows outline the borders of a slice‐thickness artifact that mimics sediment. Turning down the gain will reduce the artifact whereas sediment will persist. Color flow Doppler will also demonstrate there is no flow through the artifact. In (C) is another example of acoustic enhancement artifact with marked borders (V). In (D) probe pressure deforms the shape of the urinary bladder, making it “dumbbell” or “ figure 8” shaped, and is often uncomfortable for your patient. When measuring the urinary bladder for volume estimation, probe pressure will contribute to error.
Source: Reproduced with permission of Dr Gregory Lisciandro, Hill Country Veterinary Specialists and FASTVet.com, Spicewood, TX.
Pearl:Direct the probe into the “CC pouch” as a general rule of thumb to avoid confounders.
Pearl:Note that in puppies and kittens <6 months of age (and even up to 9 months), many have small volumes (<3 mm maximum dimension) of anechoic free fluid (ascites) that is considered normal (Lisciandro et al. 2015, 2019; Stander et al. 2010), having AFS of 1 and 2. These juveniles are most commonly positive at the CC, SRU and DH views (Lisciandro et al. 2015, 2019; Romero et al. 2015).
Don’t sweat questionable small pockets of free fluid (<3 mm), by remembering the mantra of “resuscitate, rehydrate, and reevaluate” with a serial AFAST. Always perform at least one repeat serial AFAST four hours post admission (sooner if the patient is questionable or unstable) to avoid missing subtle or nonexistent free fluid (or other soft tissue‐related pathology) on the initial AFAST that has become more obvious and substantial (Lisciandro et al. 2009).
Abnormalities of the Urinary Bladder
The AFAST from its inception in 2005 has been a target organ approach in addition to screening for free fluid, its FAST component. With the repetitive fanning through the urinary bladder, deviations from the expected appearance of the urinary bladder are bound to be noted by the sonographer, from sediment to calculi to thrombi to masses. Some examples are shown in Figures 6.27and 6.28as well as some cofounders in Figure 6.29. Chapter 11provides more detail.
AFAST Hepato‐Renal Umbilical View
| Questions Asked at the HRU (SRU) View a |
| Is there any free fluid in the abdominal (peritoneal) cavity? |
Yes or no |
| How much free fluid is at the HRU view using the AFAST AFS system? |
0, 1/2 or 1 |
| What does the small intestine look like? b |
Unremarkable or abnormal |
| What does the spleen look like? b |
Unremarkable or abnormal |
| Is the liver in view in the transverse plane of the umbilicus? b |
Yes or noIf yes, suspect hepatomegaly |
| Is the stomach in view in the transverse plane of the umbilicus? b |
Yes or noIf yes, gastric distension |
| Could I be mistaking an artifact or pitfall for pathology? |
Know pitfalls and artifacts |
aNote that this view is the HRU view in right lateral recumbency and the SRU view in left lateral recumbency.
bIt is important to know that the AFAST target organ approach for parenchymal abnormalities is binary as “unremarkable” or “abnormal” to capture the case for additional imaging and confirmatory testing. More interpretative skills may be gained through experience, and additional ultrasound study and training.
Source: Reproduced with permission of Dr Gregory Lisciandro, Hill Country Veterinary Specialists and FASTVet.com, Spicewood, TX.
The final AFAST view that is used for the AFS is the hepato‐renal umbilical (HRU) view when the patient is in right lateral recumbency. The HRU view is imaged by placing the probe just ventral to the umbilicus while staying in the transverse plane of the umbilicus. Typically the HRU view includes loops of small intestine and often the spleen, especially in dogs. Its target organs are in reality the small intestine and spleen ( Figures 6.30and 6.31). At the level of the umbilicus, the liver and stomach should not be in view unless either is severely enlarged or distended, triggering additional imaging, such as radiography. The liver and right kidney are not part of the HRU view .
The probe with the marker toward the head in longitudinal (sagittal) orientation is placed just under the umbilicus and fanned through the most gravity‐dependent region referred to as the “HRU pouch” (see Figure 6.30). Find evidence that you are in fact imaging intraabdominal structures such as the spleen or small intestine. In larger dogs, it is possible to be imaging through the abdominal muscles and not within the abdominal cavity.
The probe is not routinely run under the patient unless imaging the right kidney for the HR5th bonus view (Lisciandro et al. 2009; Lisciandro 2011).
Excessive probe pressure may cause small volumes of free fluid to move away or, in other words, to either side of the probe head and be missed.
In contrast to the previous three AFAST views, rotating the probe counterclockwise for transverse imaging at the HRU view (and SRU view when in left lateral) helps differentiate small intestinal loops from free fluid by making the small intestine in transverse or cross‐section appear like “hamburgers” and in longitudinal or sagittal appear like “highways” because the small intestine consists of five ultrasonographic layers (see Figure 6.22and Chapter 12).
When the spleen is present, use it as an acoustic window to interrogate for free fluid between its capsule and loops of small intestine.
In the first edition, this view was named the hepato‐renal (HR) view and referred to as “The Big Lie” because the liver and the right kidney are not routinely examined, so neither “HR” target organ is directly scanned (Lisciandro 2014a). So we have renamed the HR view as the “HR umbilical view” to be more descriptive of where the probe is placed, and now advocate that the small intestine and spleen be its target organs.
Читать дальше