1.6 Amelogenesis Imperfecta (AI)

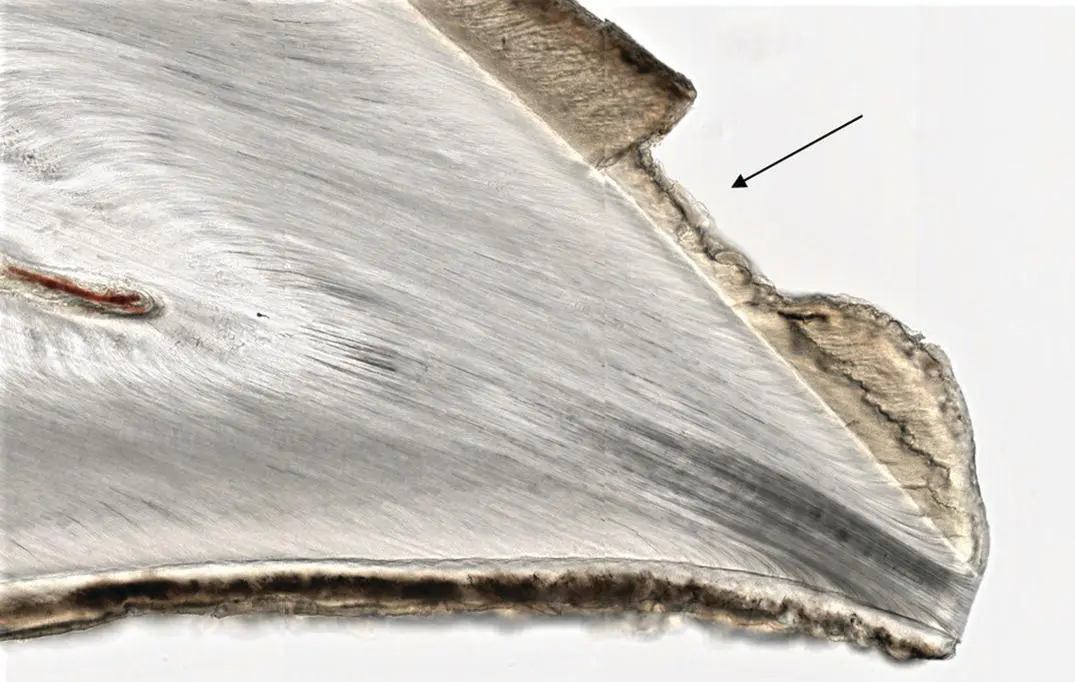
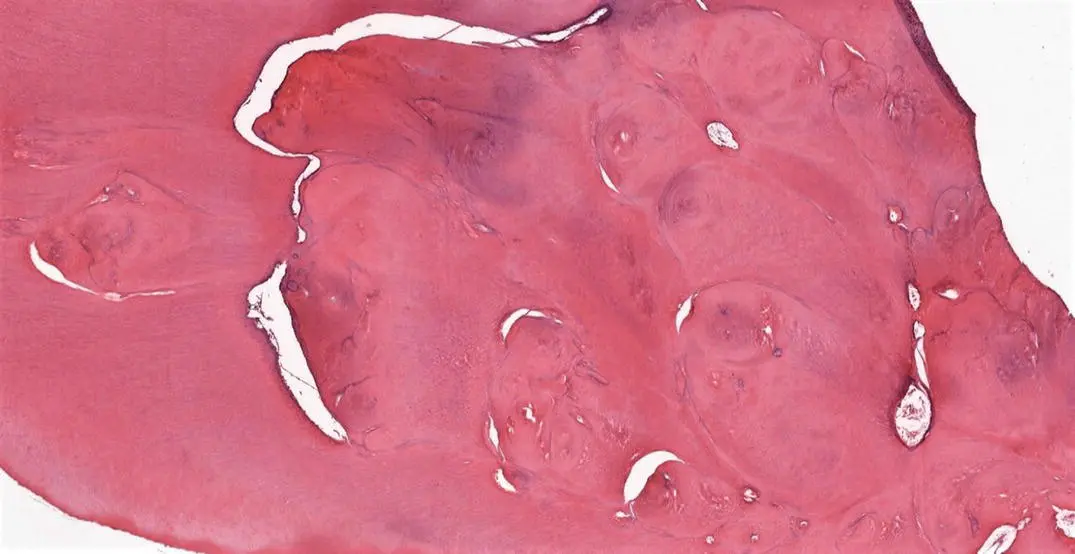
Figure 1.11Low‐power view of a ground section of a deciduous incisor showing irregular enamel surface (arrows) related to AI.
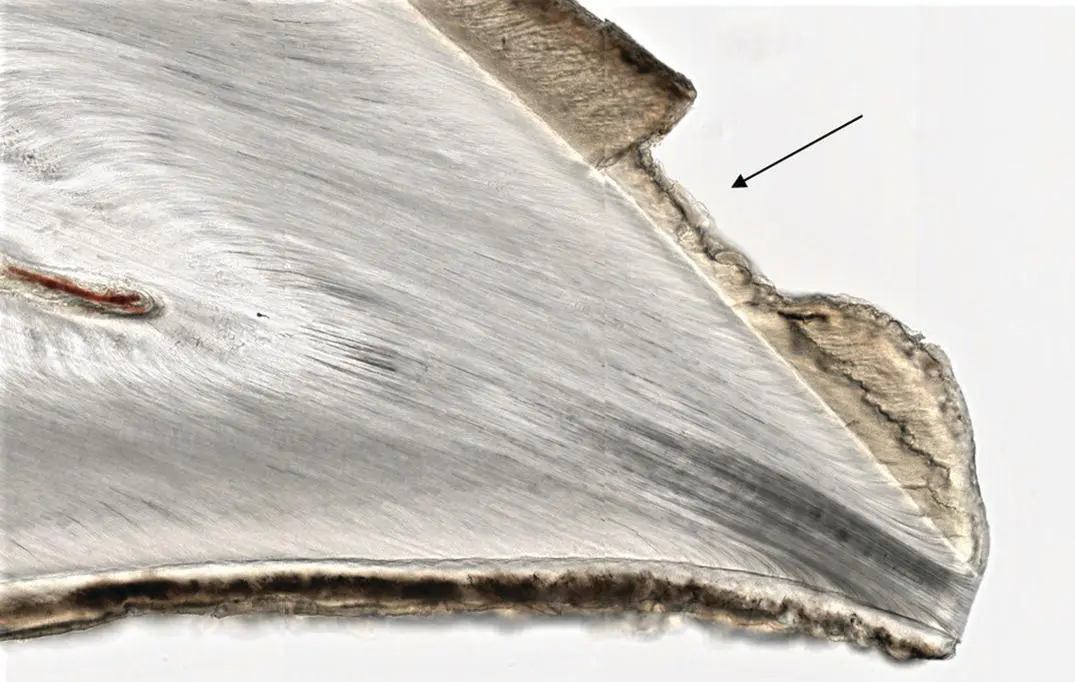
Figure 1.12High‐power view of a ground section of a deciduous incisor showing enamel pitting (arrow) related to AI.
Amelogenesis imperfecta (AI) refers to a group of inherited genetic alterations that result in a defective enamel structure. AI is usually not associated with any syndrome or systemic disease. The teeth could appear yellow, brown, or sometimes grey. Several classifications have been suggested in the literature with the most commonly used one dividing AI into hypoplastic, hypomatured, and hypocalcified types. The hypoplastic type has insufficient amount of enamel matrix, the hypomature type has defective maturation of enamel whereas the hypocalcified type shows insufficient calcification of enamel. The genetic abnormalities in AI usually affect amelogenin (AMELX), enamelin (ENAM), kallikrein (KLK4), and matrix metalloproteinase 20 (MMP‐20) genes. AI poses a significant clinical problem affecting the oral hygiene, masticatory function, and quality of life of the patient.
1.6.2 Key Identifying Features
On histological sections, it is difficult to identify the exact type of AI. However, reduced width/length of enamel along with pitting or clefts can be identified (ground sections) in addition to residual uncalcified enamel matrix (decalcified sections).
1.6.3 Clinical Considerations
Hypoplastic type is most common type of AI (60–73%) followed by hypomatured (20–40%) and hypocalcified (7%) types [9]. AI usually affects all the teeth of an individual and the diagnosis usually involves family history and clinical observation [10]. Radiographs reveal less than opaque enamel, especially when the mineralization has been affected [10]. The affected teeth are more prone to dental caries, dentinal sensitivity, and attrition [6]. Treatment options include masking of defective teeth with veneers and extra‐coronal restorations [11].
1.7 Dentinogenesis Imperfecta (DI)

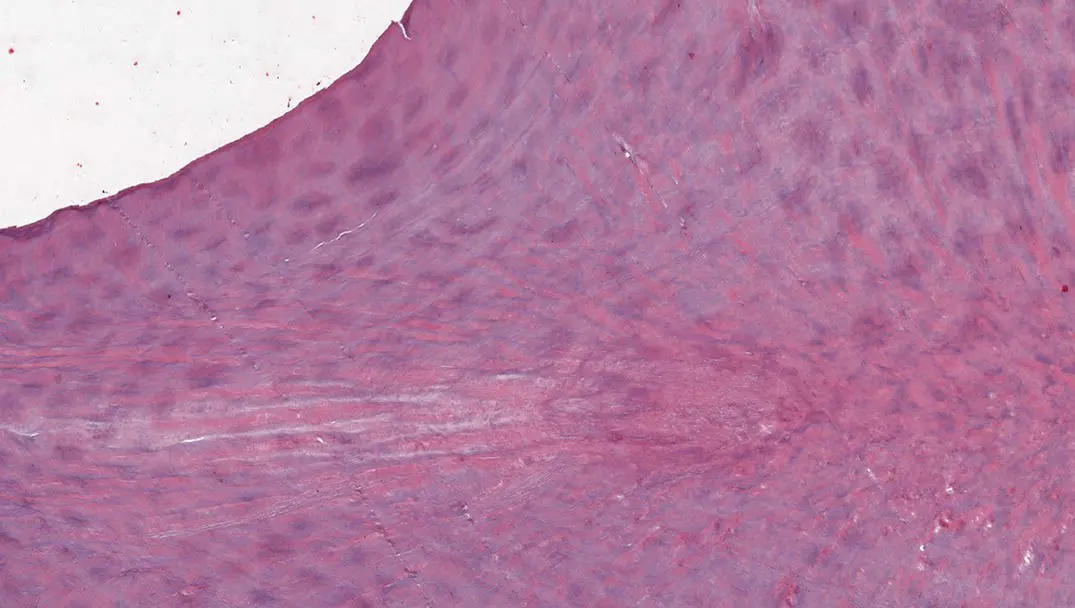
Figure 1.13H and E stained decalcified section showing DI.
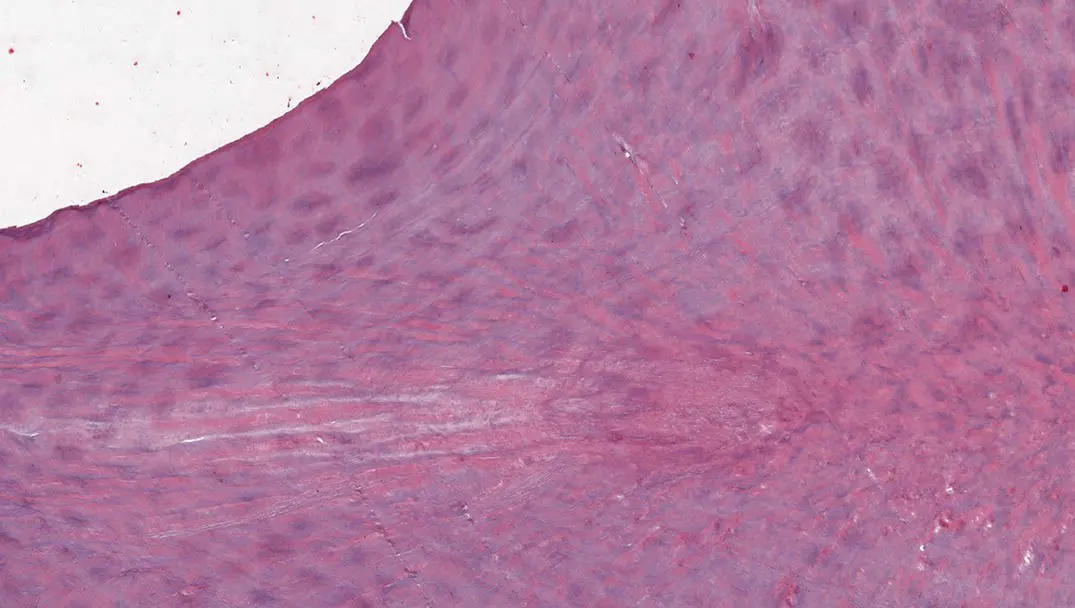
Figure 1.14H and E stained decalcified section showing DI with a haphazard tubular architecture.
Dentinogenesis imperfecta (DI) is a developmental hereditary condition (autosomal dominant) that affects the developing dentin. The dentin appears opalescent affecting both primary and permanent dentitions. DI can be classified into three main types: type I: DI associated with osteogenesis imperfecta; type II: DI similar to type I but not associated with osteogenesis imperfecta; and type III: initially reported in Brandywine population of Maryland and characterized by opalescent shell teeth (due to dentin hypotrophy) having marked attrition and large pulp chambers. As dentin forms the bulk of the tooth tissue, the teeth affected by DI are weak and prone to breakage and wear.
1.7.2 Key Identifying Features
On histological sections, teeth affected by DI show irregular dentinal tubules. In some areas, dentinal tubules can be completely absent. The dentin present can be quite irregular and haphazard and the pulp chamber can be quite small or completely obliterated.
1.7.3 Clinical Considerations
DI affects both dentitions and has an incidence of 1 in 6000 people [12]. The teeth have an amber color that ranges from yellow to brown or from blue to gray [13]. The normal scalloped interdigitation of dentin with enamel does not exist, and the flat enamel dentin junction leads to cracking of enamel followed by attrition of dentin [14]. The diagnosis is usually based on family history and the radiographical and clinical appearance of the teeth. Radiographically, the teeth usually have bulbous crowns with obliterated pulp chambers [12]. Clinically, the teeth are discolored with visible clinical defects and fractured enamel [5]. Treatment modalities include prosthetic crowns, over‐dentures, orthodontic treatment (depending upon the severity), and dental implants (when all other conservative approaches have failed [12, 15]).
1.8 Dentin Dysplasia (DD)
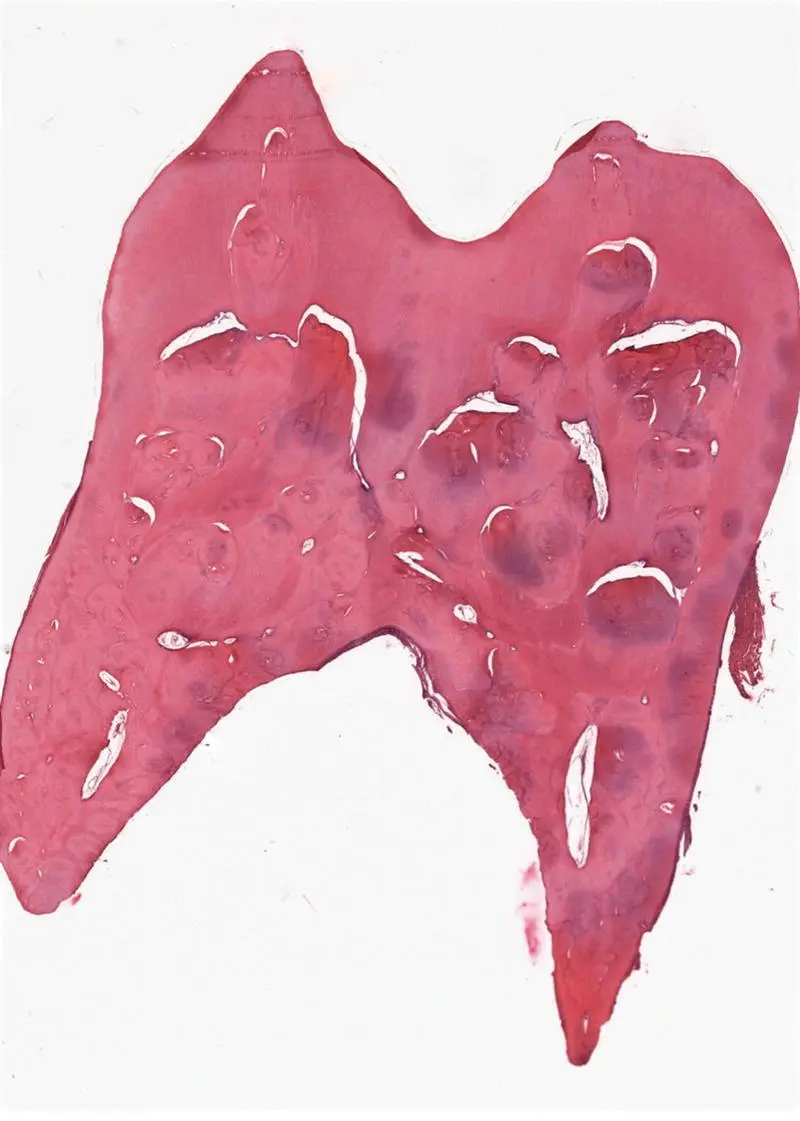
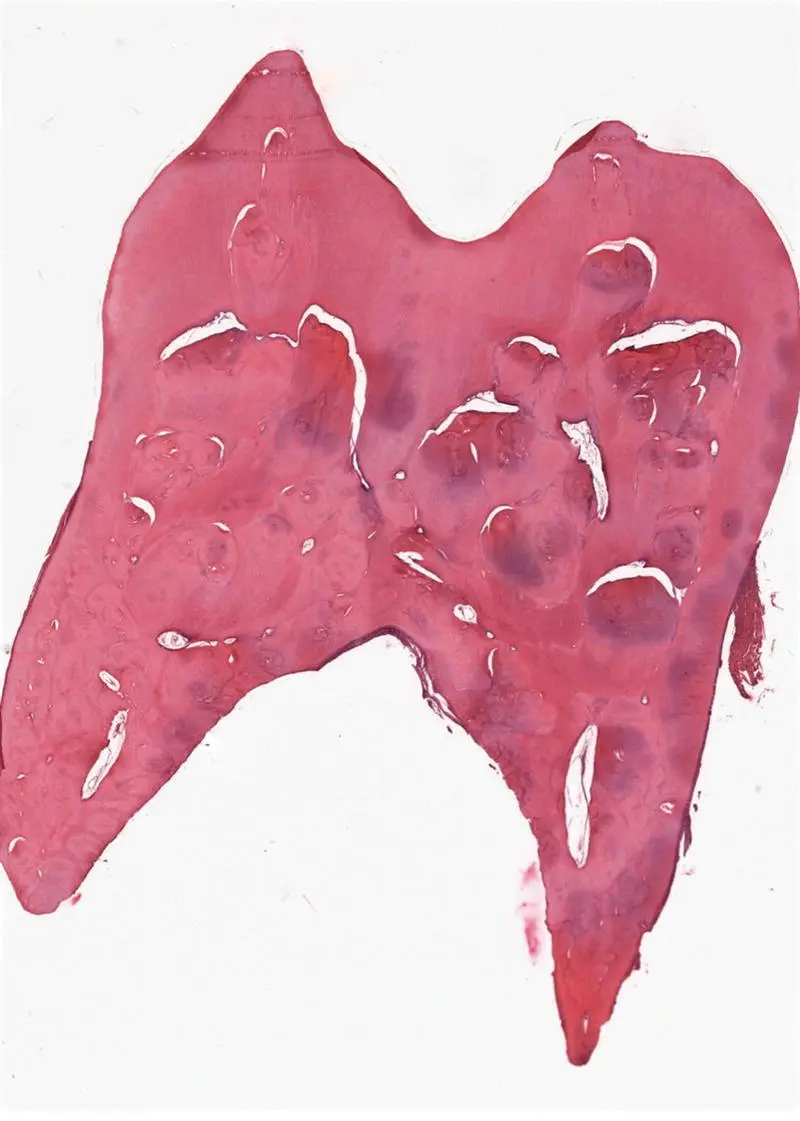
Figure 1.15H and E stained decalcified section showing DD with haphazard coalescent globules of dentin and pulpal obliteration.
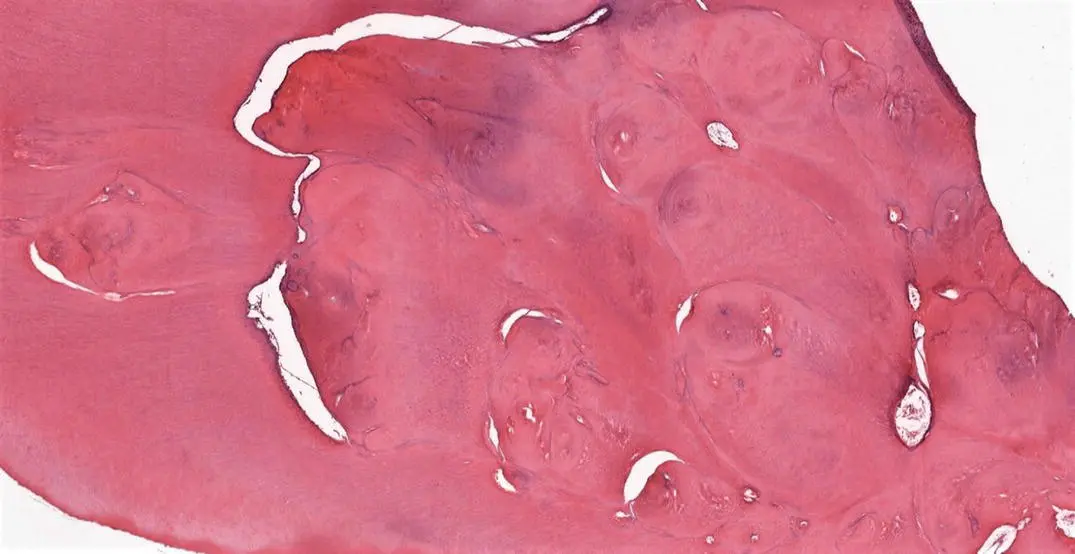
Figure 1.16H and E stained decalcified section showing DD with the typical “water around the boulders” appearance.
Dentin dysplasia (DD) is a rare genetic disorder that affects the development of dentin, mostly in radicular area. It can affect both dentitions, where the teeth have normal enamel but abnormal dentin with atypical pulp morphology. The first classification of DD was put forward by Witkop in the 1970s with DD divided into two types: DD‐1 (radicular type) and DD‐2 (coronal type) [16]. The teeth affected by DD‐1 present with short, blunt roots with obliterated pulp chambers. In DD‐2, teeth present with discoloration (brown to blue, amber colored, or opalescent), normal roots but enlarged pulp chambers (thistle tube appearance). The pulp chambers of primary teeth in DD‐2 are almost completely obliterated whereas in permanent teeth, they may be partially obliterated.
1.8.2 Key Identifying Features
Histologically, irregular dentin with a disturbed tubular pattern, atubular areas, and globular atypical dentin masses inside pulp chambers can be seen.
1.8.3 Clinical Considerations
The etiology of this disease is still unclear. Wesley et al. previously proposed that it could be due to a problem with ameloblasts which leads to an abnormal differentiation of odontoblasts, leading to DD [17]. It was also proposed earlier that due to a problem with dental papilla (foci within it becoming calcified), DD develops as a result of less growth and/or obliteration of pulp chambers [18]. The diagnosis is based on clinical examination and radiographs. The teeth affected by DD have esthetic and functional abnormalities [19]. In addition, they are more prone to be mobile and are exfoliated prematurely [19]. The treatment options include stainless‐steel crowns, endodontic therapy (although difficult due to obliteration of pulp chambers), removable dentures, and dental implants [20–22].
Читать дальше