Improving diabetes treatment and care
A key public health strategy is to implement a systematic approach to evaluate the quality of care provided to patients with diabetes. In the UK, since 2004, disease‐specific indicators for both the processes of diabetes care and the attainment of treatment targets have been assessed through the pay‐for‐performance Quality and Outcomes Framework (QoF).
In the UK in 2017, NHS England has allocated £36m to target four clinical areas where intervention is likely to result in improved outcomes, better quality care and longer term cost savings ( Table 4.2).
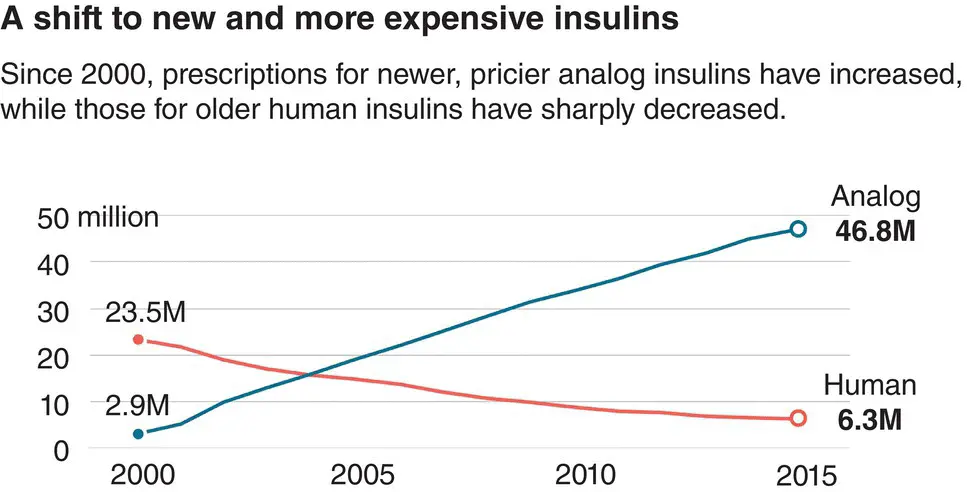
The number of diabetes treatments has increased sharply in the last 10 years. The global market for products used in the management of diabetes is in excess of $100b annually. Spending on insulin has increased faster than other diabetes drugs, and there has been a big shift towards analog insulins ( Figure 4.10).
Digital health interventions are likely to play an important role in improving the quality of diabetes care in the next 5–10 years. Digital and E‐health initiatives will include:
Wearable technologies that monitor levels of exercise.
Apps which allow users to access health coaches.
Online peer support groups.
Provide the ability to set and monitor goals electronically.
Table 4.2 Transformation Funding in the UK in 2017 is targeting 4 key areas to improve quality of care, outcomes and to achieve longer term cost savings.
| Work stream |
Approx funding |
| Improving Attainment |
|
| of NICE recommended |
£14m |
| Targets (HbA1c, BP, Lipids) |
|
| Increased Access to |
|
| Structured Education |
£11m |
| For T1 and T2 DM |
|
| Reducing the No of |
|
| Amputations by Improving |
£6m |
| Access to Multidisciplinary Foot |
|
| Teams |
|
| Improving Access to in‐patient |
£4m |
| Diabetes specialist nurses |
|
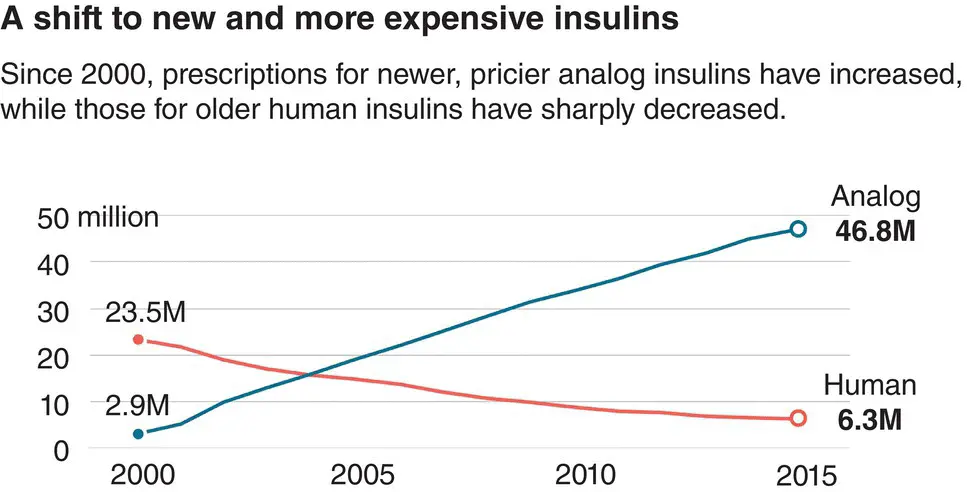
Figure 4.10 The shift towards using new, expensive analogue insulins. IMS Health.
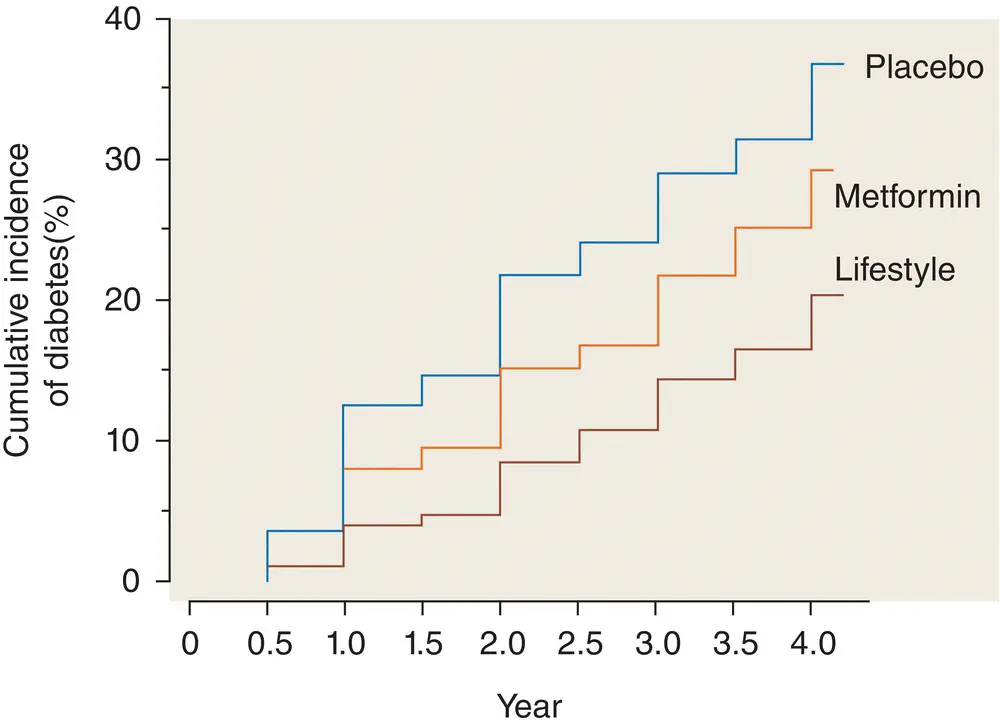
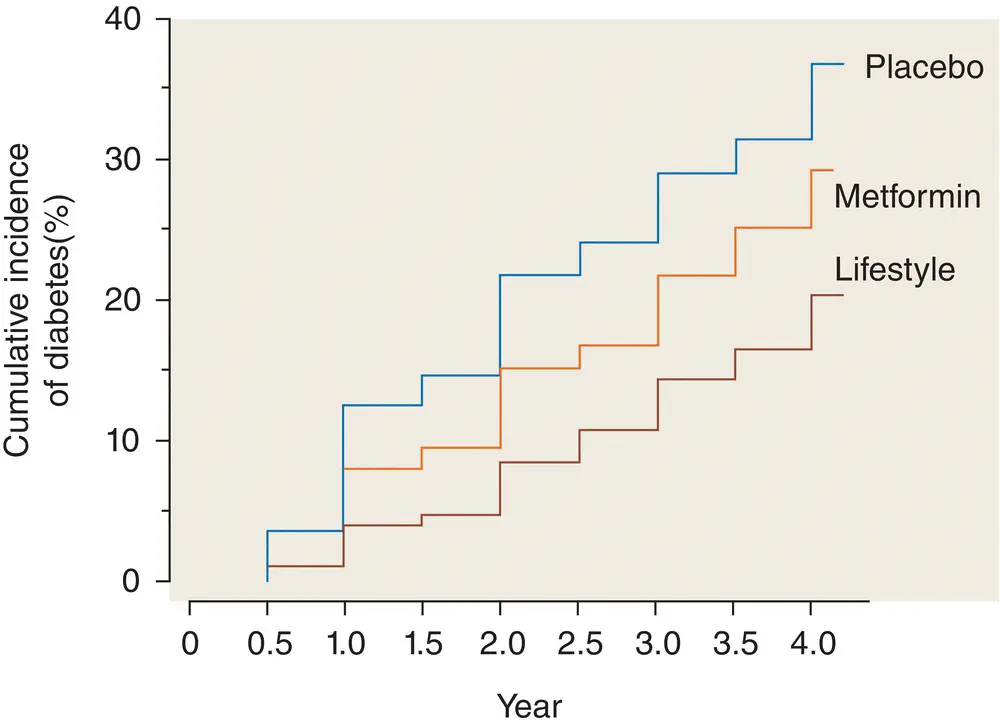
Figure 4.11 A structured lifestyle modification program (aimed at delivering >7% weight loss and 150 minutes of physical activity per week) is superior to drug treatment with metformin and placebo in diabetes prevention. Lifestyle intervention reduced the risk of type 2 diabetes by 58%.
Adapted from Diabetes Prevention Study. N Engl J Med 2002; 346: 393–403.
Commissioning diabetes services
Improving population metrics for the quality of diabetes care as well as clinical outcomes hinges on effective local and national commissioning of diabetes services. Public Health England uses a Diabetes Outcomes versus Expenditure (DOVE) scoring tool to judge how cost‐effective local Clinical Commissioning Groups (CCGs) are in procuring services for their population. Guidance has been produced ( Table 4.3).
Table 4.3 Top Tips For Commissioning Diabetes Services.
Adapted From: NHS Clinical Commissioners: Excellence in Commissioning Diabetes Care, April 2017
| Involve PatientsUse Data: to Identify local & national variations and to identify areas for interventionStrong Leadership: Especially from GP’sIdentify Diabetes Champions: Both in Primary & Secondary CareDevelop Partnerships: For example with industry to support implementationOutcome‐Based Approached: Collaborate with healthcare providers to move from activity to outcomes‐based approaches |
1 Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403.
2 Huxley R, Barzi F, Woodward M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta‐analysis of 37 prospective cohort studies. BMJ 2006; 332: 73–76.
3 Li G, Zhang P, Wang J, et al. The long‐term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention study: a 20‐year follow‐up study. Lancet 2008; 371: 1783–1789.
4 Patterson CC, Dahlquist G, Gyurus E, et al. Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005–2020: a multicentre prospective registration study. Lancet 2009; 373: 2027–2033.
1 Alexander GC, Sehgal N, Moloney R, Stafford R. National trends in treatment of type 2 diabetes mellitus, 1994–2007. Arch Intern Med 2008; 168: 2088–2094.
2 Bain SC, Feher M, Russell‐Jones D, et al. Management of type 2 diabetes: the current situation and key opportunities to improve care in the UK. Diab. Obes. Metab. 2016; 18:1157–1166.
3 Currie CJ, Peters JR, Tynan A, et al. Survival as a function of HbA1c in people with type 2 diabetes: a retrospective cohort study. Lancet 2010; 375: 481–489.
4 Goyder EC. Screening for and prevention of type 2 diabetes. BMJ 2008; 336: 1140–1141.
5 Jee SH, Sull J, Park J, et al. Body–mass index and mortality in Korean men and women. N Engl J Med 2006; 355: 779–787.
6 Rosella LC, Lebenbaum M, Fitzpatrick T, et al. Impact of Diabetes on healthcare costs in a population‐based cohort: a cost analysis. Diabet. Med 2016; DOI: 10.1111/dme.12858.
7 Selvin E, Steffes MW, Zhu H, et al. Glycated haemoglobin, diabetes and cardiovascular risk in nondiabetic adults. N Engl J Med 2010; 362: 800–811.
8 Zghebi SS, Steinke DT, Carr MJ, et al. Examining trends in type 2 diabetes incidence, prevalence and mortality in the UK between 2004 and 2014. Diab. Obes. Metab. 2017; doi: 10.1111/dom.12964.
Chapter 5 Normal physiology of insulin secretion and action, and the incretin effect
KEY POINTS
Islets of Langerhans in the endocrine pancreas contain β (insulin‐producing) and α (glucagon‐producing) cells that regulate glucose homeostasis. Pancreatic β cells may change in size, number, and function during normal ageing and development.
Insulin secretion is biphasic: an acute first phase response that lasts a few minutes followed by a more gradual sustained second phase. Glucose is the main stimulator of insulin secretion, but other hormones, nutrients and neurotransmitters play an important role in the regulation of insulin secretion.
The so‐called incretin effect (meal‐stimulated augmentation of insulin secretion) is diminished in type 2 diabetes, mainly because of reduced GLP‐1 secretion. The discovery, characterisation and clinical development of glucagon‐like peptides has been a major success over the last 30 years.
Insulin receptor signalling in key tissues (skeletal muscle, fat and liver) is complex, resulting in various biological effects of insulin on glucose, lipid and protein metabolism.
Islet structure and function
Insulin is synthesised in and secreted from the β cells within the islets of Langerhans in the pancreas. The normal pancreas has about 1 million islets, which are derived embryologically from endodermal outgrowths of the foetal gut. The islets can be identified easily with various histological stains with which the cells react less intensely than does the surrounding exocrine tissue ( Figure 5.1). Pancreatic islets vary in size from having a few dozen to several thousands of cells and they are scattered irregularly throughout the exocrine pancreas.
Читать дальше