1 ...7 8 9 11 12 13 ...25 The potential value of screening for diabetes is to facilitate early diagnosis and treatment. About 20% of newly diagnosed type 2 diabetic subjects already have evidence of vascular complications, such as retinopathy, the prevalence of which increases with diabetes duration. This suggests that complications begin about 5–6 years before a diagnosis is made, and that the actual onset of (type 2) diabetes may be several years before the clinical diagnosis.
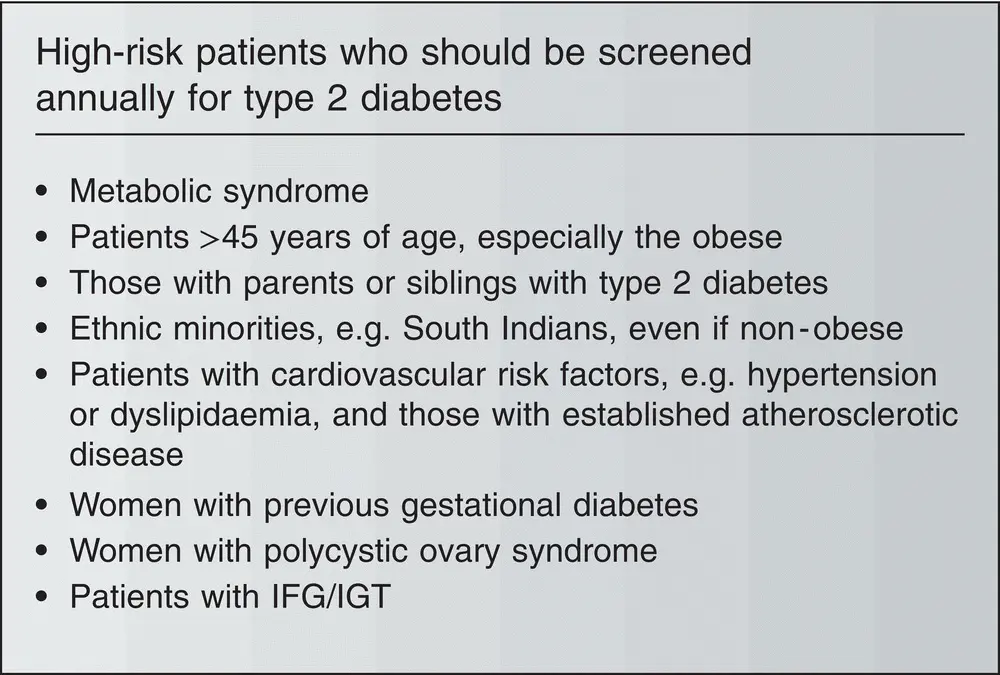
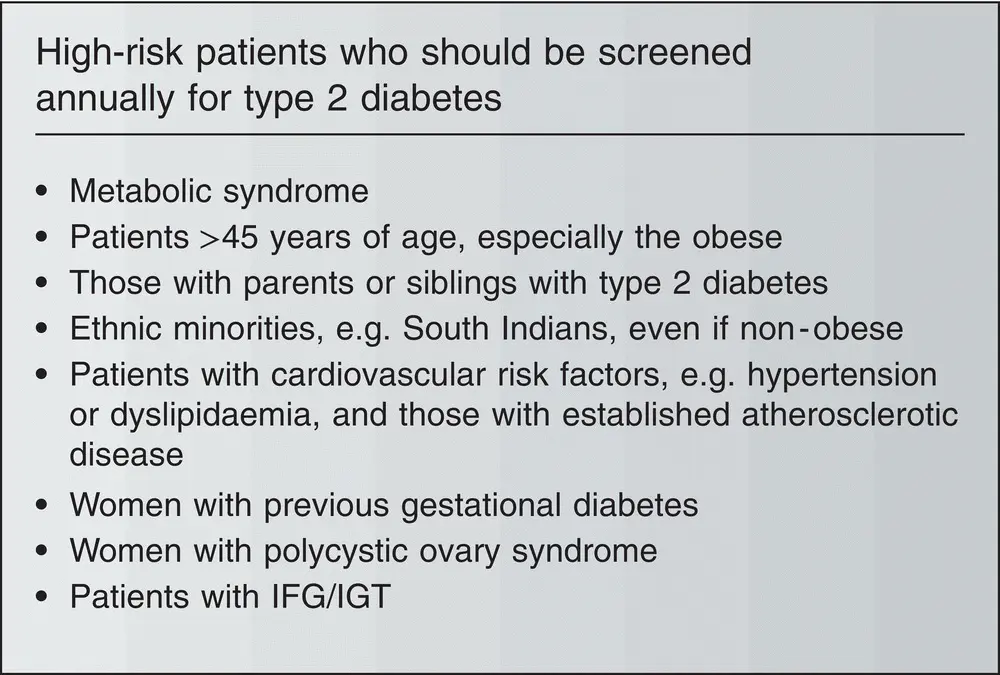
Figure 3.5 High‐risk patients who should be screened annually for type 2 diabetes .
In most countries, there is no systematic screening policy for diabetes, yet there are estimates that up to 50% of patients with diabetes are undiagnosed. Ad‐hoc screening of high‐risk groups is becoming more common. The fasting plasma glucose is simple, quick, acceptable to patients and of low cost, but can miss those with isolated post‐challenge hyperglycaemia and requires patient to be fasted. The OGTT is more difficult to perform, impractical for large numbers and expensive, but is the only way to identify post‐load hyperglycaemia. Screening should focus on high‐risk groups. HbA1c is widely used to screen individuals at high risk of developing diabetes.
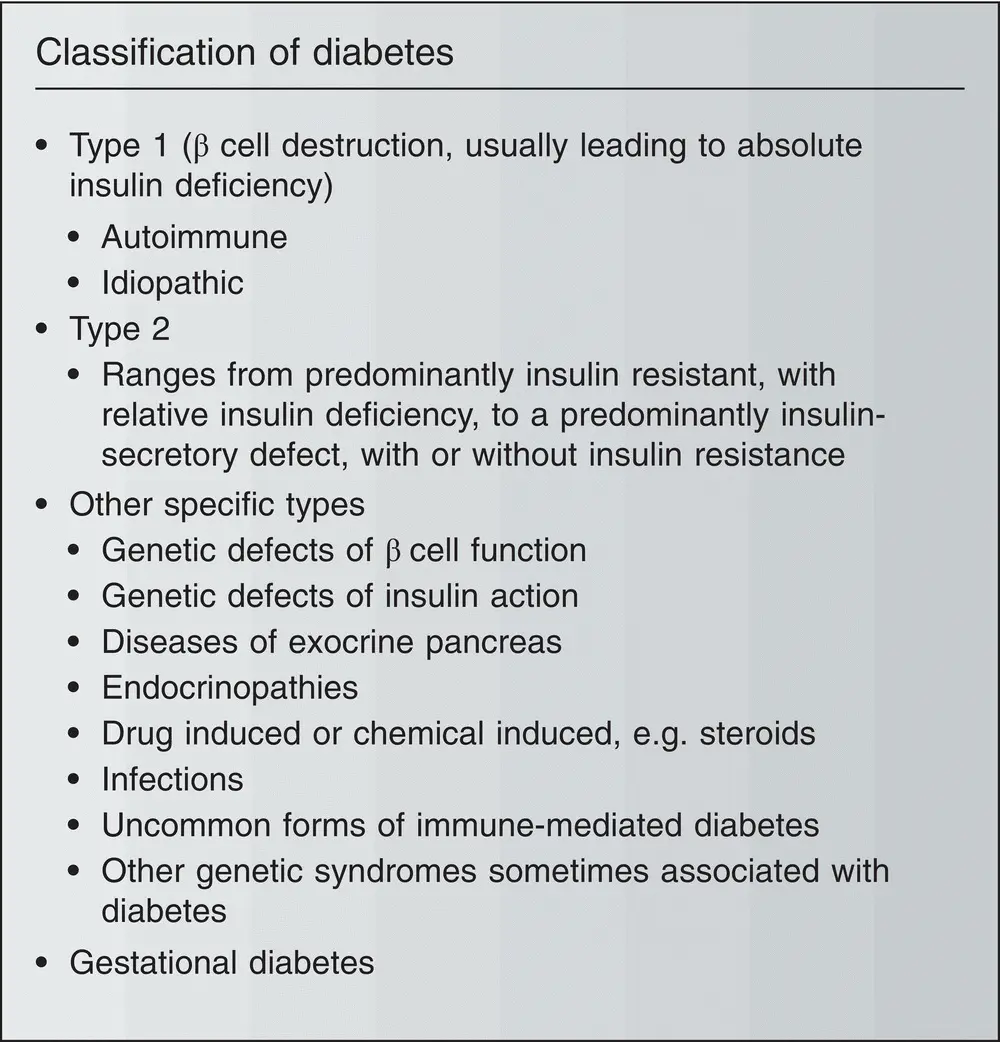
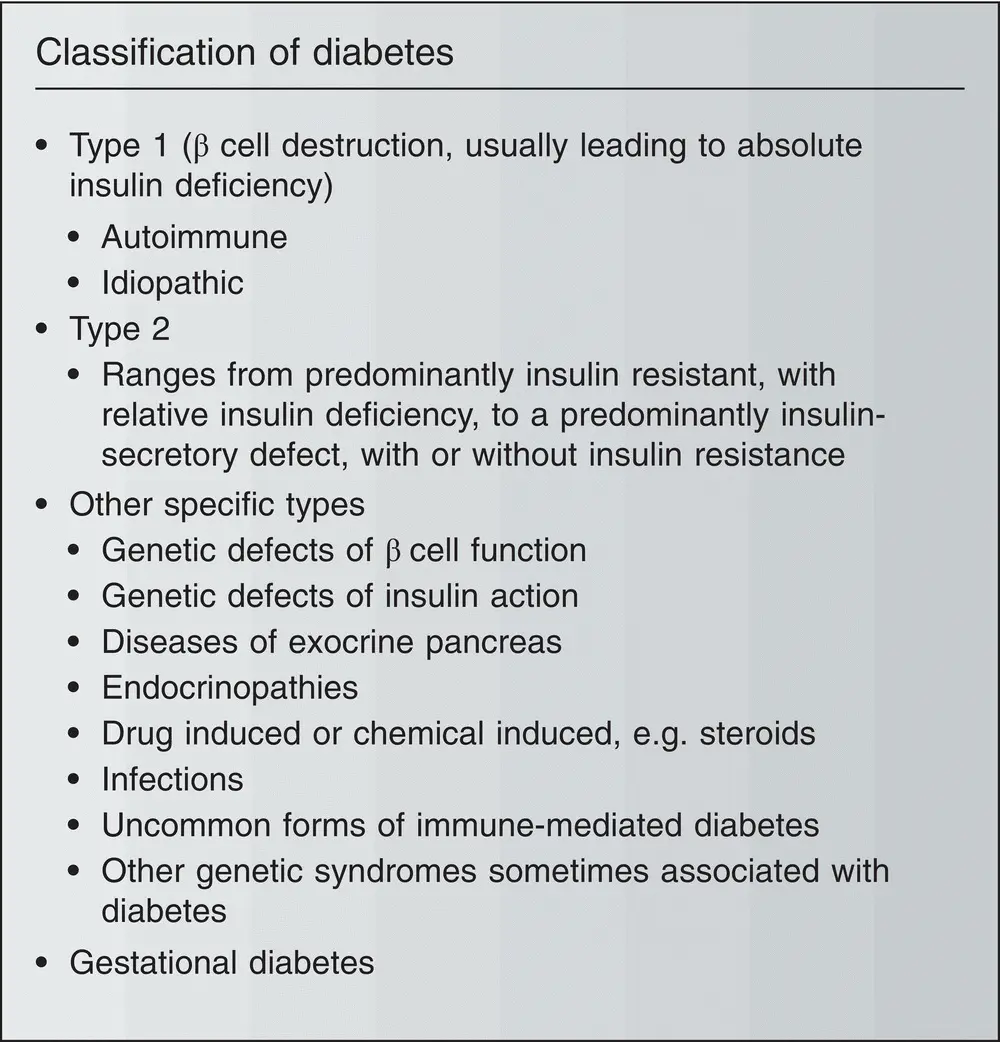
Figure 3.6 Classification of diabetes .
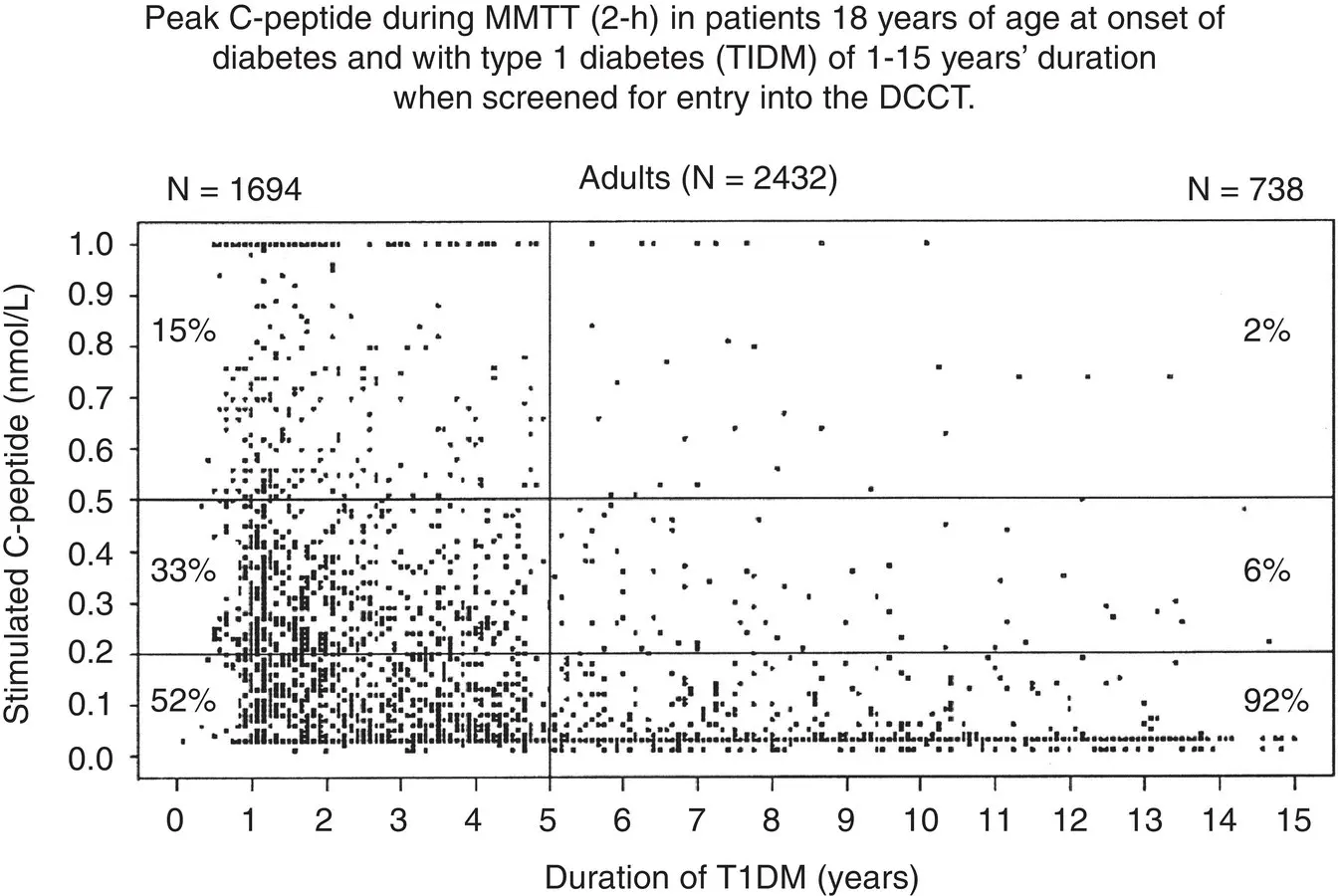
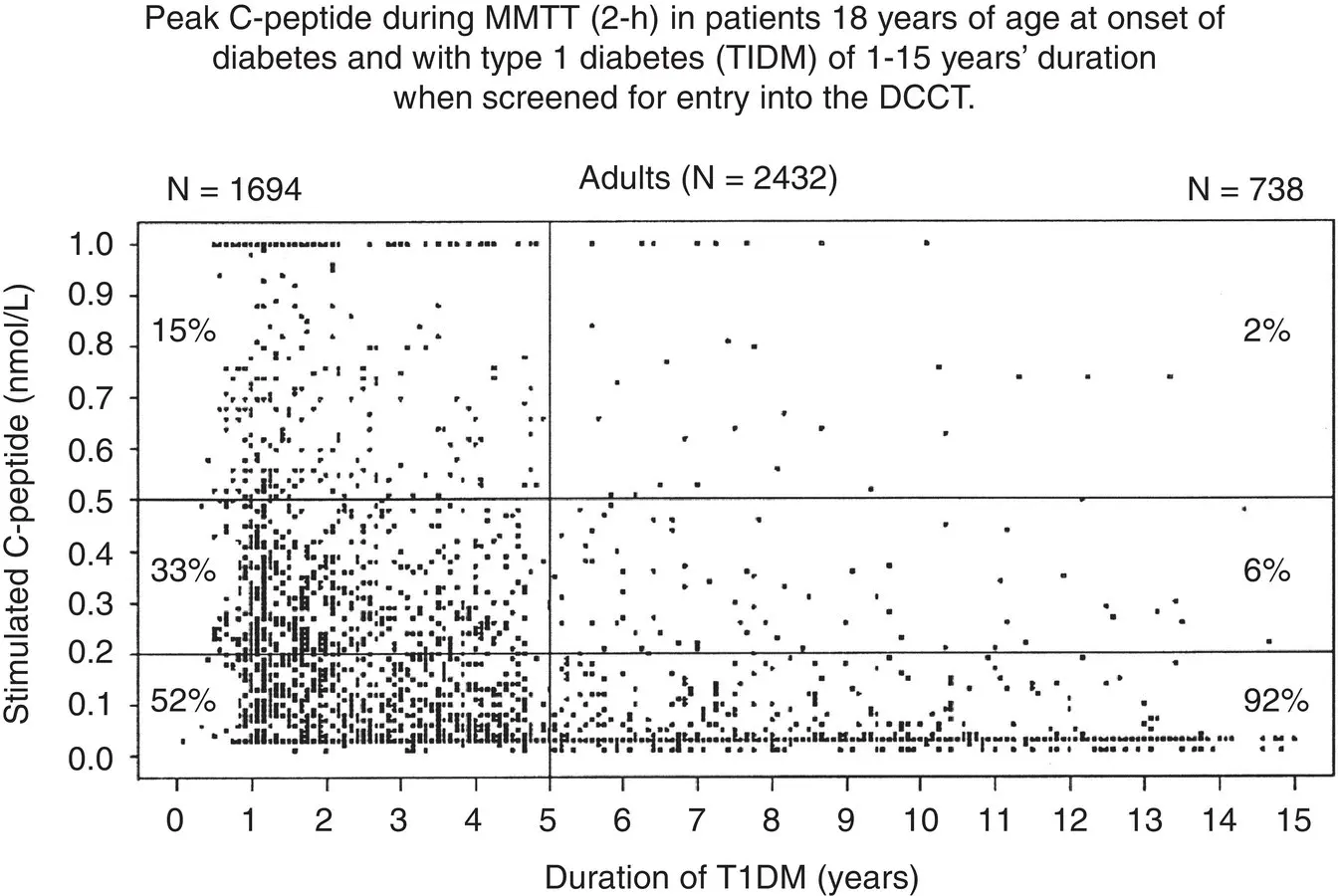
Figure 3.7Using C‐peptide to confirm type 1 diabetes based on residual beta cell function. MMT‐mixed meal tolerance test – i.e. patients ingested a standardized breakfast ingested over 10 min based on the total caloric need of the patient (25–30% of their daily caloric intake; 50% of the calories as carbohydrates). In routine practice this is utilised as a random ‘c‐peptide’ level.
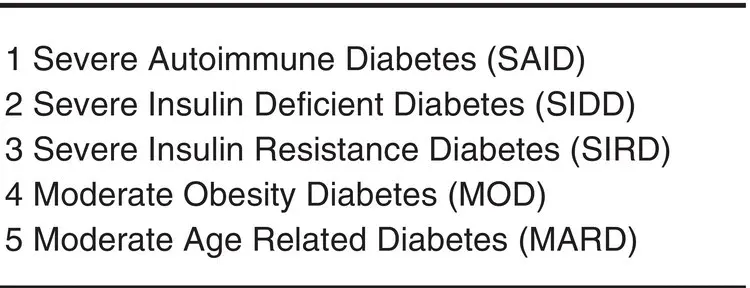
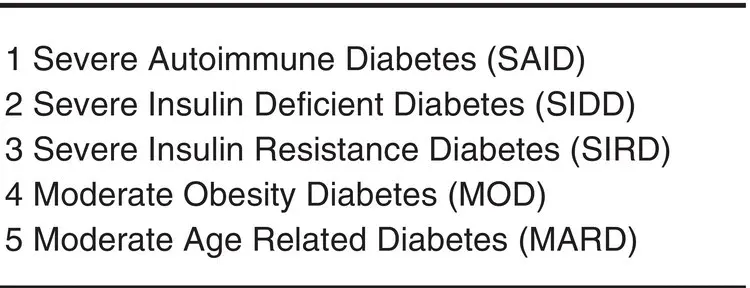
Figure 3.8Five replicable clusters of patients with diabetes.
Source: Adapted from Ahlqvist et al. Lancet Diabetes & Endocrinology, 1 March 2018.
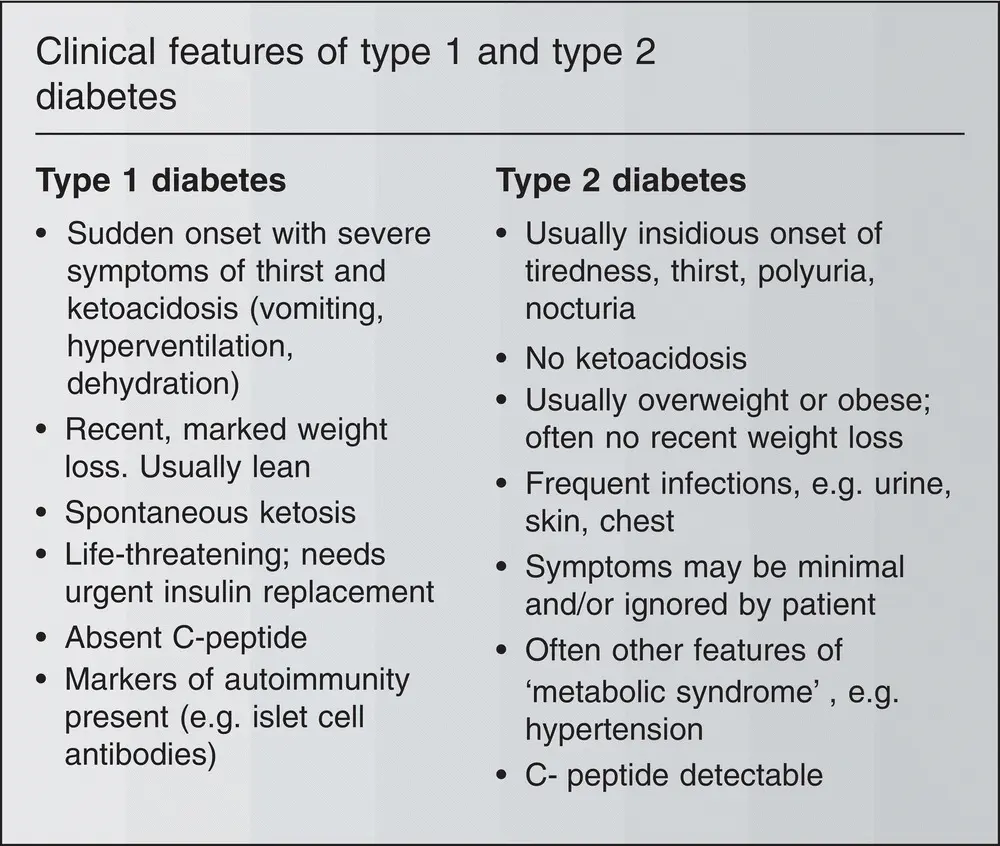
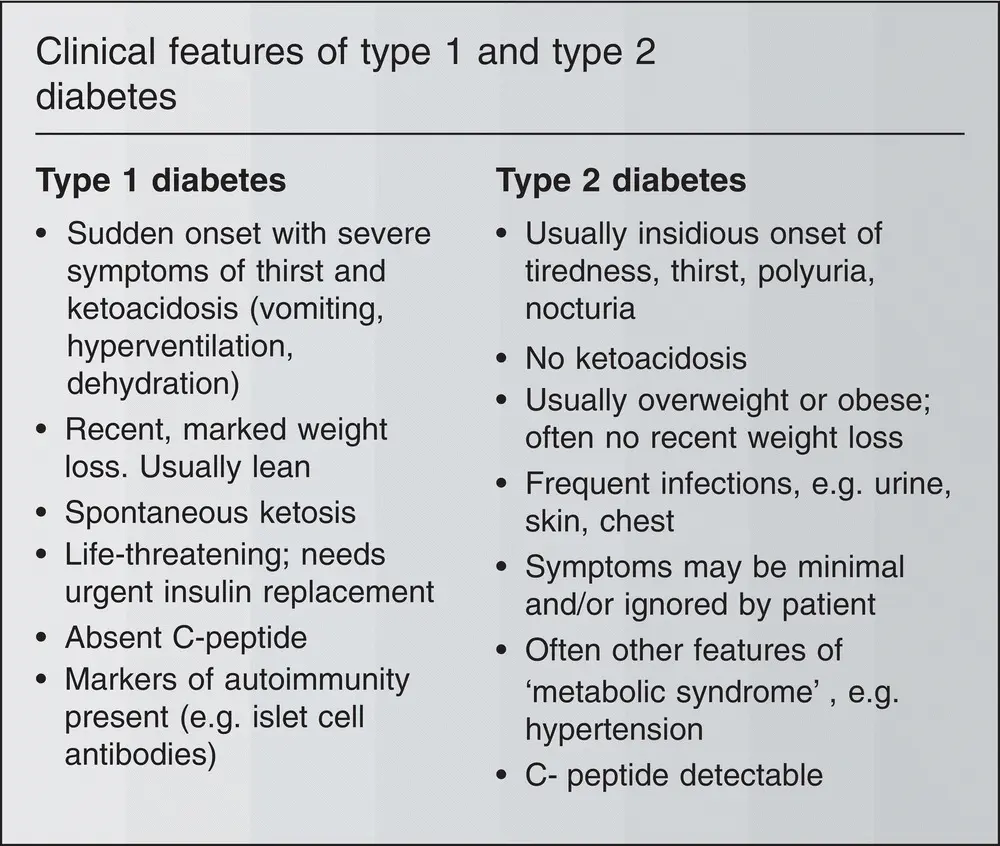
Figure 3.9Clinical features of type 1 and type 2 diabetes.
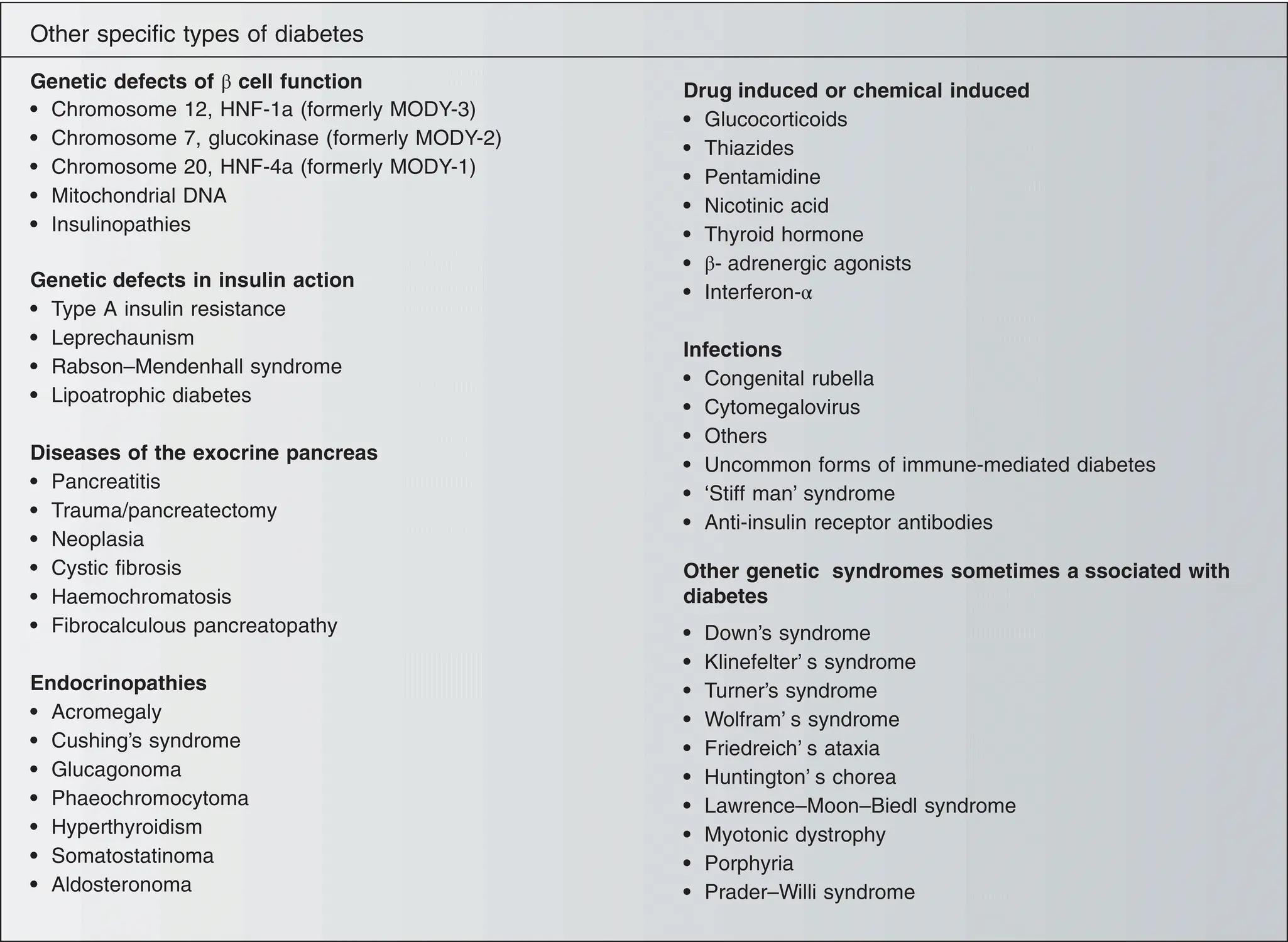
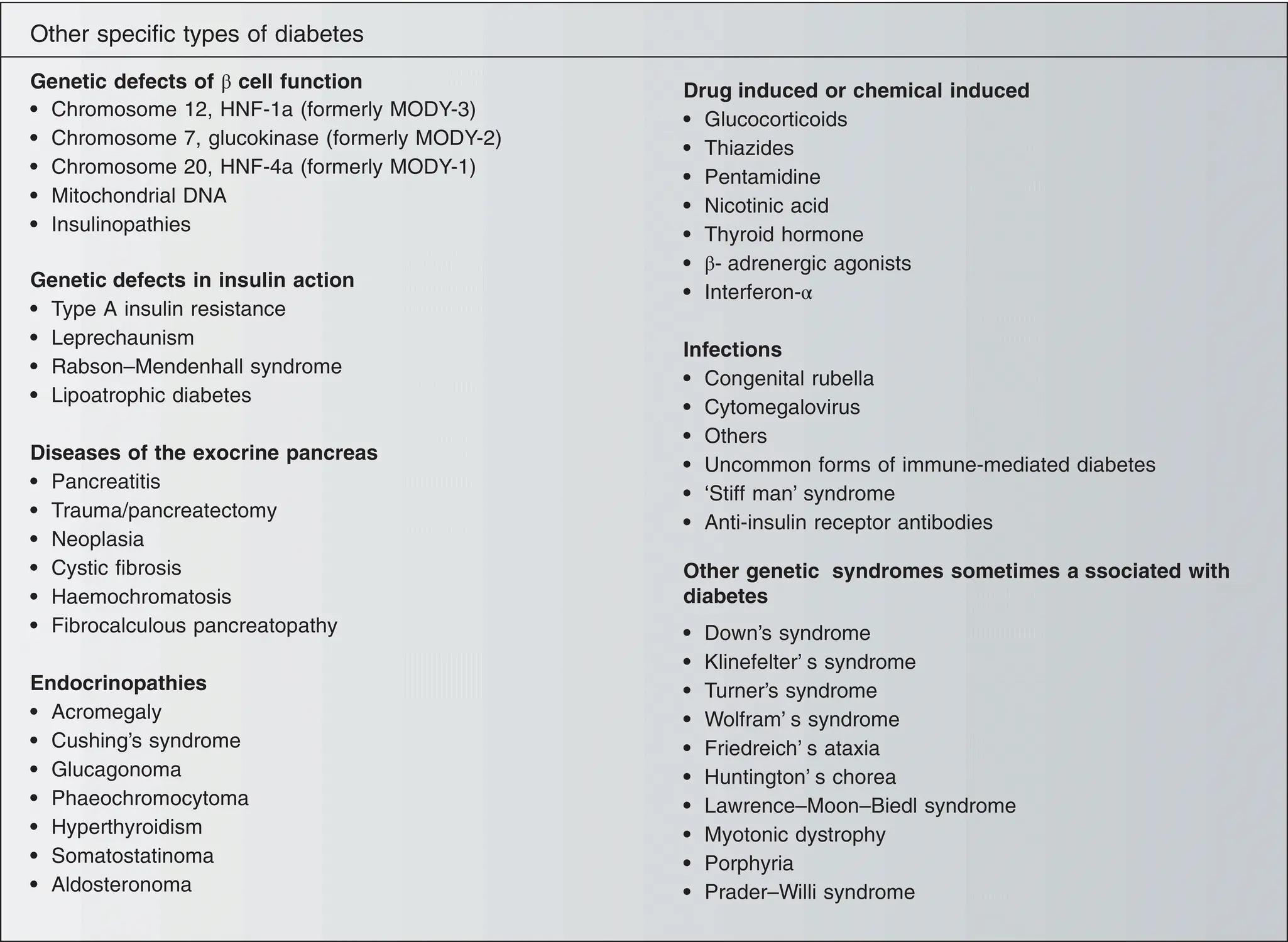
Figure 3.10Other specific types of diabetes.
Classification of diabetes
The current classification of diabetes is based on the aetiology of the disease. There are four categories:
Type 1 diabetes (caused by pancreatic islet cell destruction);
Type 2 diabetes (caused by a combination of insulin resistance and β‐cell insulin secretory dysfunction);
Other specific types of diabetes (caused by conditions such as endocrinopathies, diseases of the exocrine pancreas, genetic syndromes, steroid induced etc., see below);
Gestational diabetes (defined as diabetes that occurs for the first time in pregnancy).
Type 1 diabetes is subdivided into two main types: 1a or autoimmune (about 90% of type 1 patients in Europe and North America, in which immune markers, such as circulating islet cell antibodies, suggest autoimmune destruction of the β‐cells) and 1b or idiopathic (where there is no evidence of autoimmunity).
A steady increase (2.5–3% per annum) in the incidence of type 1 diabetes has been reported worldwide, especially among young children <4 years old. There are large differences between countries in the incidence of type 1 diabetes, e.g up to 10‐fold differences among European countries.
This classification has now replaced the earlier, clinical classification into ‘insulin‐dependent diabetes mellitus’ (IDDM) and ‘non‐insulin‐dependent diabetes mellitus’ (NIDDM), which was based on the need for insulin treatment at diagnosis. IDDM is broadly equivalent to type 1 diabetes and NIDDM to type 2 diabetes. One of the disadvantages of the old classification according to treatment was that subjects could change their type of diabetes – for example, some type 1a patients diagnosed after the age of 40 years masquerade as NIDDM, before eventually becoming truly insulin‐dependent (this is now classified as latent autoimmune diabetes in adults, LADA). Where diagnostic uncertainty exists between type 1 versus non type 1 diabetes, c‐peptide assessments can determine residual function beta cells (and insulin dependency to prevent ketoacidosis).
Various clinical and biochemical features can be used to decide whether the patient has type 1 or type 2 diabetes. The distinction may be difficult in individual cases.
A recent study have suggested a novel classification of adult onset diabetes according to patient characteristics (glutamate decarboxylase antibodies, age at diagnosis, BMI, HbA1c and homoeostatic model assessment 2 estimates of beta cell function and insulin resistance) and risk of diabetic complications.
1 Severe Autoimmune Diabetes (SAID)
2 Severe Insulin Deficient Diabetes (SIDD)
3 Severe Insulin Resistance Diabetes (SIRD)
4 Moderate Obesity Diabetes (MOD)
5 Moderate Age Related Diabetes (MARD)
Their study showed that individuals in cluster 3 (Most resistant to insulin) had significantly higher risk of diabetic kidney disease than individuals in cluster 4 and 5. Cluster 2 (insulin deficient) had the highest risk of diabetic eye disease. The largest cluster is cluster 5.
The category of ‘other specific types of diabetes’ is a large group of conditions, which includes genetic defects in insulin secretion [such as in maturity‐onset diabetes of the young (MODY) and insulinopathies], genetic defects in insulin action (e.g. syndromes of severe insulin resistance), pancreatitis, steroid induced and other exocrine disorders, hormone‐secreting tumours such as acromegaly (growth hormone) and Cushing’s syndrome (cortisol). Some cases are caused by the administration of drugs such as glucocorticoids. Some genetic syndromes are sometimes associated with diabetes (e.g. Down syndrome, Klinefelter’s syndrome and many more).
A 66‐year‐old retired policeman attends his family doctor for a routine BP check. He has had hypertension for 4 years. He reports incidentally that he has been feeling generally tired and lethargic. On further questioning, he admits to nocturia x3 and volunteers that in recent months he has been taking a glass of water to bed since he often wakes feeling thirsty. The GP notices that he had a cutaneous boil lanced 6 weeks ago. Apart from hypertension, there is no other significant past medical history, but his body weight has gradually risen (95kg, BMI 32). He takes an ACE inhibitor, lisinopril 10mg, for hypertension. His mother had type 2 diabetes, he is a non‐smoker and drinks 15 units of alcohol per week. His only exercise is golf, twice per week. The doctor takes a random venous blood sample, which shows a plasma glucose level of 13 mmol/L. Further blood tests show a normal haematology profile, normal electrolytes and renal function, HbA1c 8.3%, and fasting lipids show total cholesterol 6.6mmol/L, LDL‐cholesterol 4.3mmol/L, triglycerides 3.9mmol/L and HDL‐cholesterol 0.6mmol/L. Minor abnormalities of liver function are also noted (AST & ALT 2‐3x upper limit).
Читать дальше