In the early twentieth century, several workers isolated impure hypoglycaemic extracts from the pancreas, including the Berlin physician Georg Zuelzer (1840–1949), the Romanian Nicolas Paulesco (1869–1931), and the Americans Ernest Scott (1877–1966) and Israel Kleiner (1885–1966).
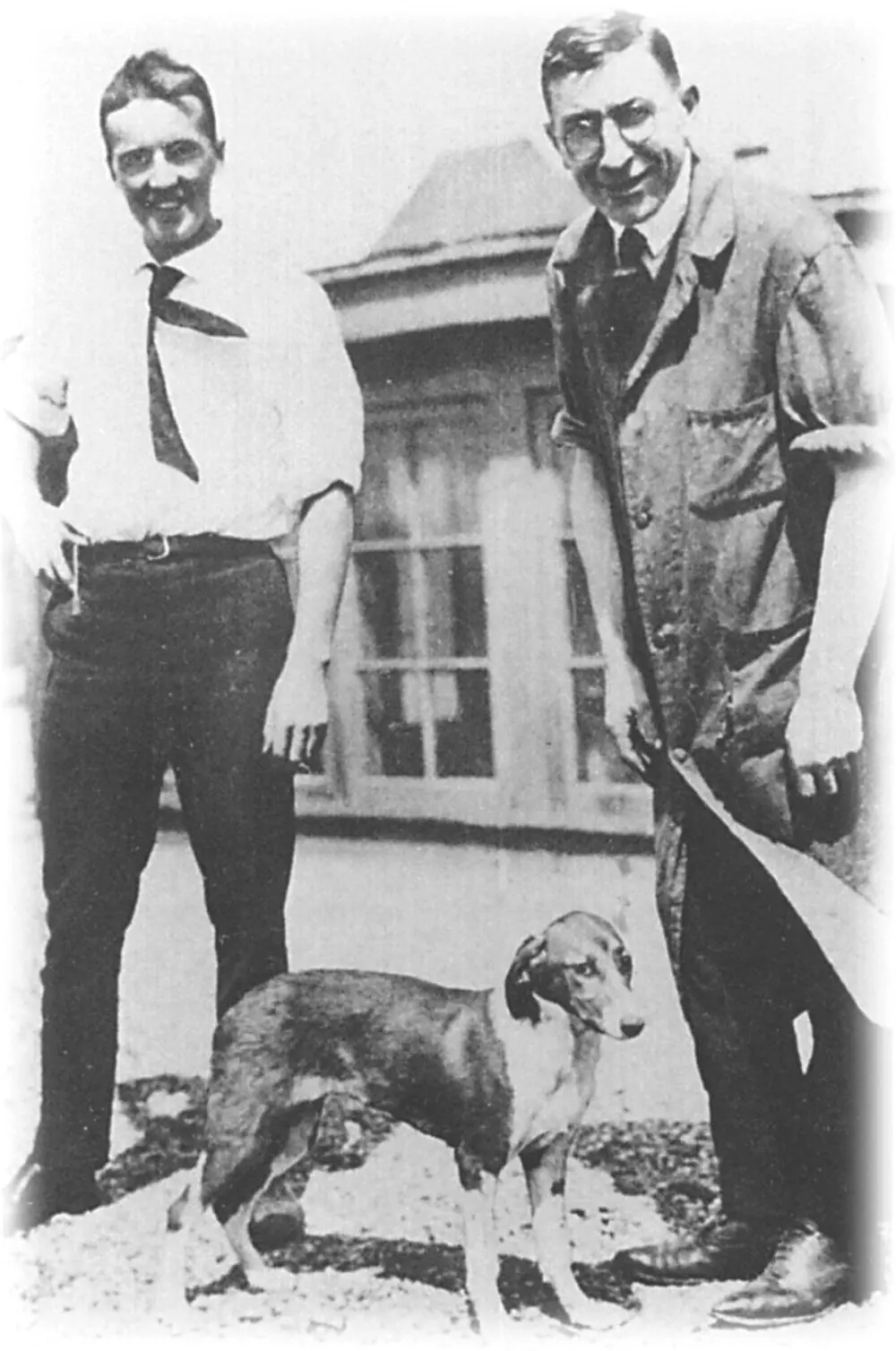
Insulin was discovered in 1921 at the University of Toronto, Canada, through a collaboration between the surgeon Frederick G Banting (1891–1941), his student assistant Charles H Best (1899–1978), the biochemist James B Collip (1892–1965) and the physiologist JJR Macleod (1876–1935). Banting and Best made chilled extracts of dog pancreas, injected them into pancreatectomised diabetic dogs, and showed a fall in blood glucose concentrations ( Figure 2.5).
Figure 2.4 Paul Langerhans. The Wellcome Institute Library, London, UK.
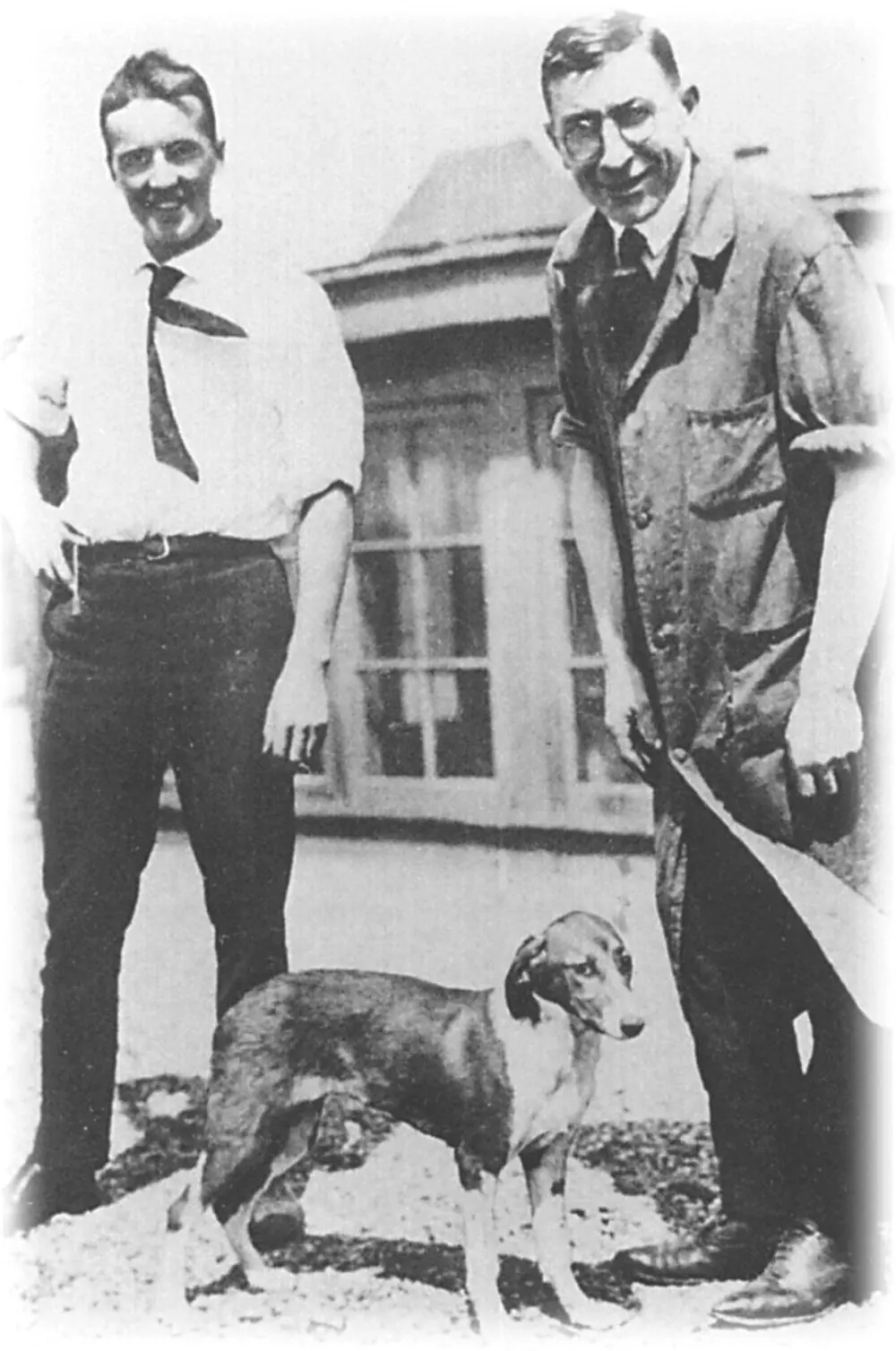
Figure 2.5 Charles Best and Frederick Banting in Toronto in 1922 (the dog is thought to have been called Marjorie). The Wellcome Institute Library, London, UK.
Banting and Best’s notes of the dog experiments refer to the administration of ‘isletin’, later called insulin at the suggestion of Macleod. They were unaware that the Belgian Jean de Meyer had already coined the term ‘insuline’ in 1909. (All these names ultimately derive from the Latin for ‘island’.)
Collip improved the methods for the extraction and purification of insulin from the pancreas, and the first person with diabetes, a 14‐year‐old boy called Leonard Thompson, was treated on 11 January 1922. A commercially viable extraction procedure was then developed in collaboration with chemists from Eli Lilly and Co. in the USA, and insulin became widely available in North America and Europe from 1923. The 1923 Nobel Prize for Physiology or Medicine was awarded to Banting and Macleod, who decided to share their prizes with Best and Collip.
The American physician Elliot P Joslin (1869–1962) was one of the first doctors to gain experience with insulin. Working in Boston, he treated 293 patients in the first year after August 1922. Joslin also introduced systematic education for his diabetic patients.
In the UK, the discovery of insulin saved the life of the London physician Robin D Lawrence (1892–1968), who had recently developed type 1 diabetes. He subsequently played a leading part in the founding of the British Diabetic Association now Diabetes UK.
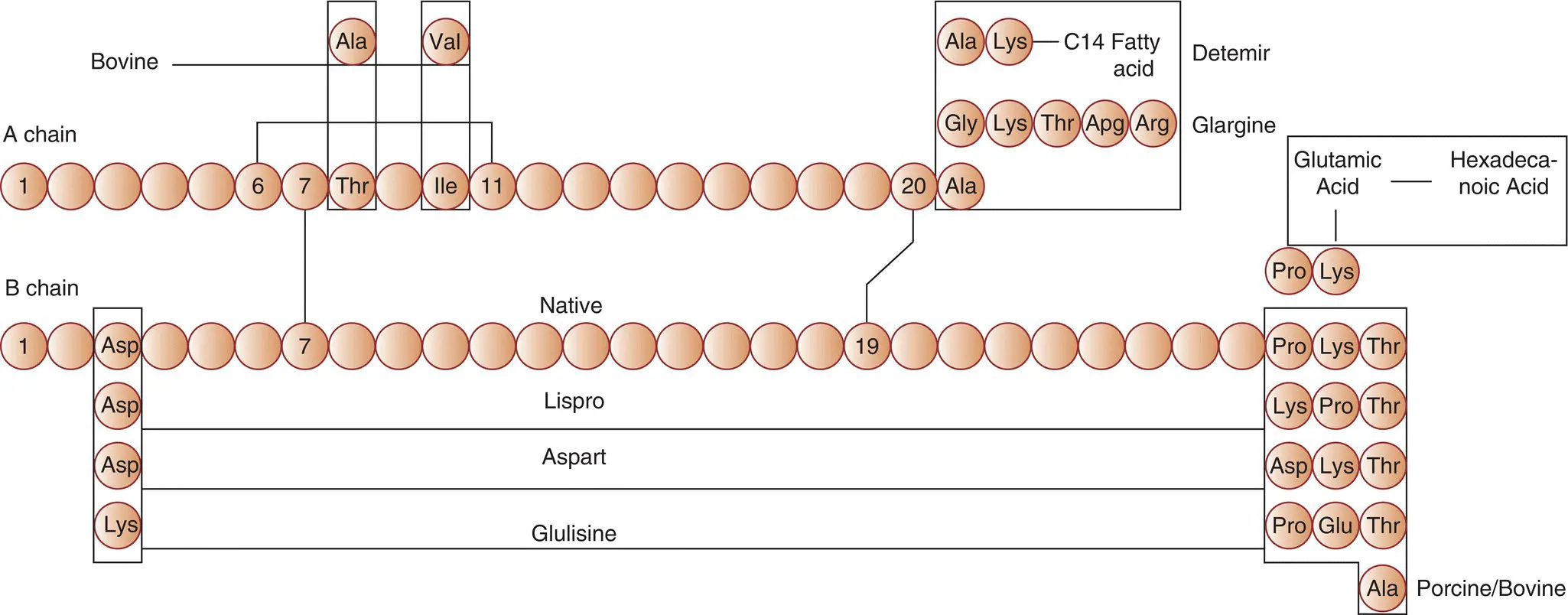
Among the many major advances since the introduction of insulin into clinical practice was the elucidation in 1955 of its primary structure (amino acid sequence) ( Figure 2.6) by the Cambridge UK scientist Frederick Sanger (b. 1918), who received the Nobel Prize for this work in 1958.
Oxford‐based Dorothy Hodgkin (1910–1994), another Nobel Prize winner, and her colleagues described the three‐dimensional structure of insulin using X‐ray crystallography (1969). In total, there have been five Nobel Prizes awarded for scientific discoveries related to diabetes and carbohydrate metabolism.
By the 1950s, it was accepted that tissue complications, such as those that occur in the eye and kidney, continued to develop in long‐standing diabetes, in spite of insulin treatment. The definitive proof that normalisation of glycaemia could prevent or delay the development of diabetic complications had to wait until 1993 for type 1 diabetes (the Diabetes Control and Complications Trial in North America) and 1998 for type 2 diabetes (the UK Prospective Diabetes Study – UKPDS).
Until the 1980s, insulin was derived only from animal pancreata, in increasingly more refined preparations. Using additives such as protamine or zinc, the subcutaneous absorption could be delayed, thus providing 24‐hour availability using 2–4 injections a day of different preparations.
With the development of genetic engineering, it became possible to produce human insulin and subsequent further manipulations of the molecule have led to a wide range of preparations ( Figure 2.6) with different absorption profiles ( Chapter 10). There has been extensive research into an orally effective form of insulin but a continuing dependence upon subcutaneous injection as the main route of administration is likely for the foreseeable future.
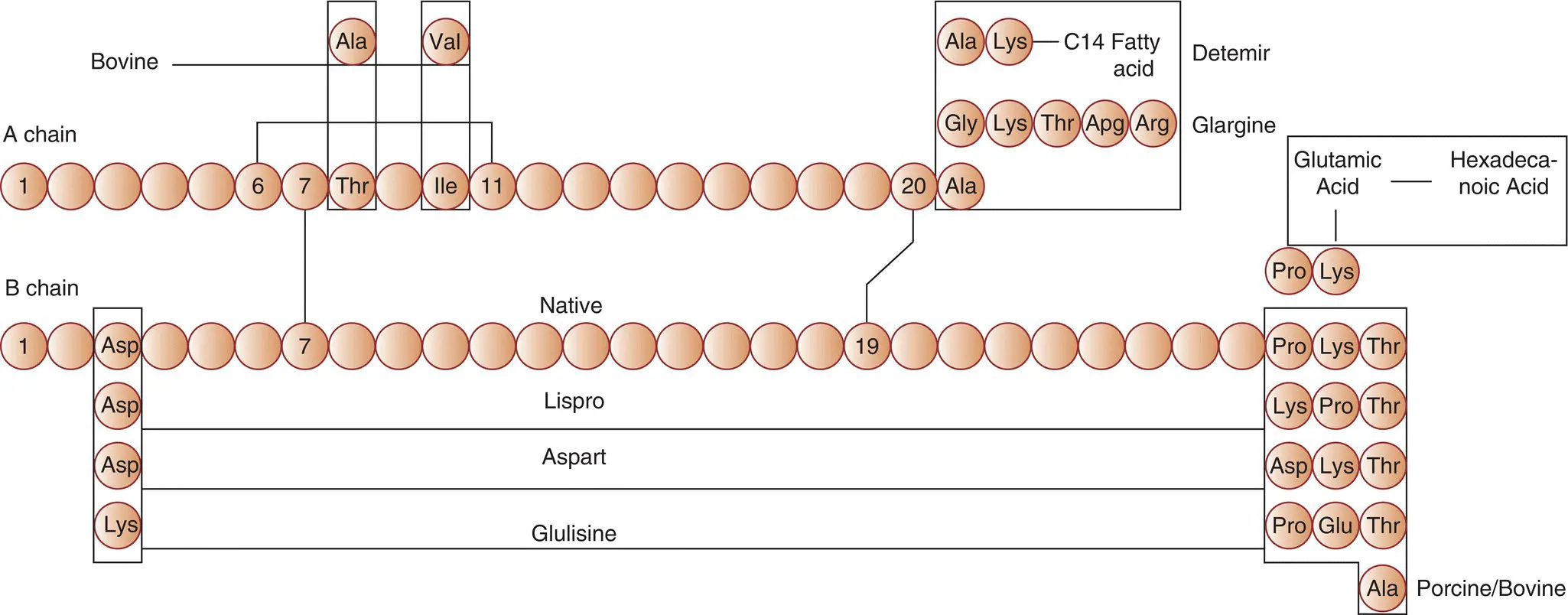
Figure 2.6 Schematic amino acid sequence of human insulin; porcine and bovine insulin; the short‐acting insulin analogues aspart, lispro, and glulisine; and the long‐acting analogues glargine, detemir, and degludec.
In the 1980s, capillary blood glucose testing was a major breakthrough for patients allowing them to precisely assess their blood glucose levels and check for hypoglycaemia. Modern meters allow downloading of results enabling better informed modification of insulin regimens.
The rapid evolution of insulin delivery devices and continuous subcutaneous glucose sensing over the last decade has led to the production of closed loop systems which are effectively acting as an artificial pancreas. These systems are revolutionising the management of type 1 diabetes, although their cost poses significant challenges for health care funders and has inevitably limited their use.
In type 2 diabetes oral agents have been available since the 1950s, bur the last few decades have seen the production of many different classes of compound that affect insulin secretion, its efficacy and sensitivity, as well as whole body glucose dispersal and excretion. This has led to the development of personalised diabetes therapy based upon the likely defect in the individual patient. This concept of personalised medicine forms the basis of recent guidelines for type 2 diabetes ( Chapter 11).
1 Bliss, M. The Discovery of Insulin. Toronto: McLelland and Stewart, 1982.
Chapter 3 Diagnosis and classification of diabetes
Diabetes mellitus is diagnosed by identifying chronic hyperglycaemia. The World Health Organisation (WHO) and the American Diabetes Association (ADA) use a fasting plasma glucose (FPG) of 7 mmol/L or higher to define diabetes ( Table 3.1). This originates from epidemiological studies in the 1990s which appeared to show that the risk of microvascular complications (e.g retinopathy) increases sharply at a FPG threshold of 7 mmol/L ( Figure 3.1). Lately, the notion of a clear glycaemic threshold separating people at high and low risk of diabetic microvascular complications has been called into question. The relationship between plasma glucose and microangiopathy is likely to be continuous, thus a FPG of 7 mmol/L is an arbitrary cut‐off for defining diabetes which may be lowered in the future.
There are currently 34.2 million people in the USA with diabetes (10.5% of the population). Approximately 7 million of these are not yet aware that they have diabetes. The total number of people with diabetes worldwide is projected to increase from 171 million in 2000 to 366 million in 2030. A key demographic change to the rising prevalence of diabetes worldwide is an increasing proportion of people >65 years of age.
Table 3.1 Diagnostic criteria for Type 2 diabetes.
| Diabetes may be diagnosed based on plasma glucose criteria, either the fasting plasma glucose (FPG) or the 2‐h plasma glucose (2‐h PG) value after a 75‐g oral glucose tolerance test (OGTT) or A1C criteria. |
| Criteria for the diagnosis of diabetes. |
| FPG ≥126 mg/dL (7.0 mmol/L). Fasting is defined as no caloric intake for at least 8 h. * |
| 2‐h PG ≥200 mg/dL (11.1 mmol/L) during an OGTT. The test should be performed as described by the WHO, using a glucose load containing the equivalent of 75 g anhydrous glucose dissolved in water. * |
| A1C ≥6.5% (48 mmol/mol). The test should be performed in a laboratory using a method that is NGSP certified and standardized to the DCCT assay. * |
| In a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a random plasma glucose ≥200 mg/dL (11.1 mmol/L). |
*In the absence of unequivocal hyperglycemia, results should be confirmed by repeat testing.
Читать дальше