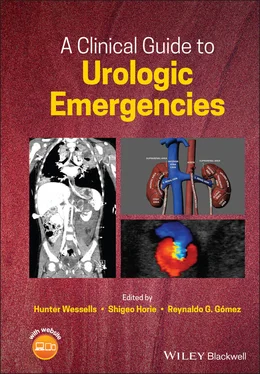
A Clinical Guide to Urologic Emergencies
Здесь есть возможность читать онлайн «A Clinical Guide to Urologic Emergencies» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:A Clinical Guide to Urologic Emergencies
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:5 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 100
- 1
- 2
- 3
- 4
- 5
A Clinical Guide to Urologic Emergencies: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «A Clinical Guide to Urologic Emergencies»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
A Clinical Guide to Urologic Emergencies
www.wiley.com/go/wessells/urologic A Clinical Guide to Urologic Emergencies
A Clinical Guide to Urologic Emergencies
A Clinical Guide to Urologic Emergencies — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «A Clinical Guide to Urologic Emergencies», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
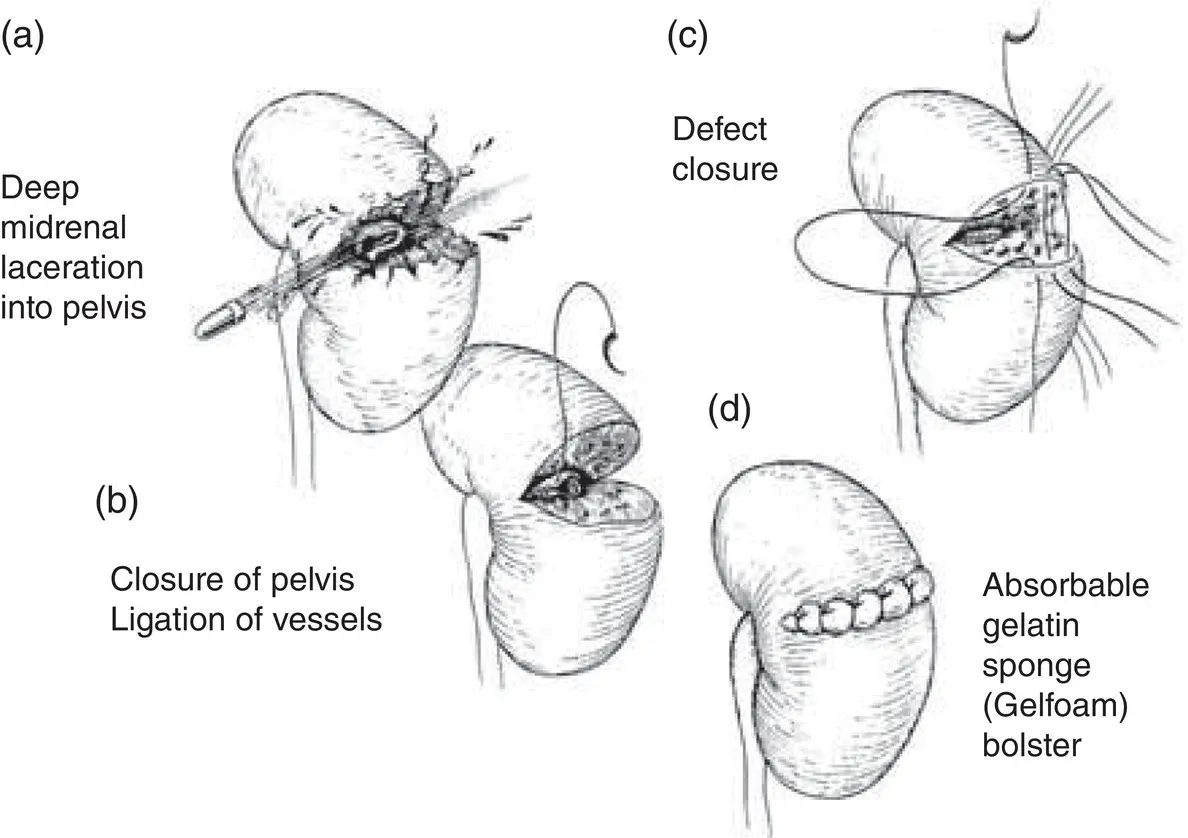
Figure 2.5Renorrhaphy. (a) Deep midrenal laceration into pelvis. Basic reconstructive principles of renorrhaphy include (b) closure of pelvis and ligation of vessels, (c) defect closure, and (d) placement of Gelfoam ®bolsters.
Source: from Buckley and McAninch [48], with permission.
Regardless of approach, after vascular control, the renal fascia is opened and the kidney is dissected from the surrounding hematoma. Renal reconstruction is then performed. The principles include complete renal exposure, debridement of nonviable parenchyma, suture ligation of bleeding vessels, closure of any collecting system injuries, and re‐approximation of the parenchyma (see Figure 2,5). For injuries to the renal pelvis, a ureteral stent should be placed. This can be placed antegrade via the collecting system defect. Then the renal pelvis should be repaired with a fine, absorbable suture (i.e. 5–0 PDS: polydioxanone suture). Collecting system defects with overlying renal parenchyma, even large ones, do not require routine stenting. Omental flaps may be used for coverage of the repair.
All sutures during the renorrhaphy should be absorbable. The renorrhaphy is performed using an absorbable suture (i.e. 2–0 polysorb) in interrupted horizontal mattress fashion. Pledgets made out of Surgicel can be used to prevent tearing of the sutures from the renal parenchyma. Some urologists place a bolster dressing in the renorrhaphy bed with a hemostatic agent such as Gelfoam or Surgicel (see Figure 2.6). A closed suction drain should be placed in the retroperitoneum but not directly on the renorrhaphy site.
Thrombosis of the renal artery and vein should be managed conservatively. Although surgical revascularization has a high technical success rate, most patients have irreversible ischemic damage or delayed thrombosis [39, 40]. These repairs should only be attempted on patients with solitary kidneys or if they have bilateral occlusion.
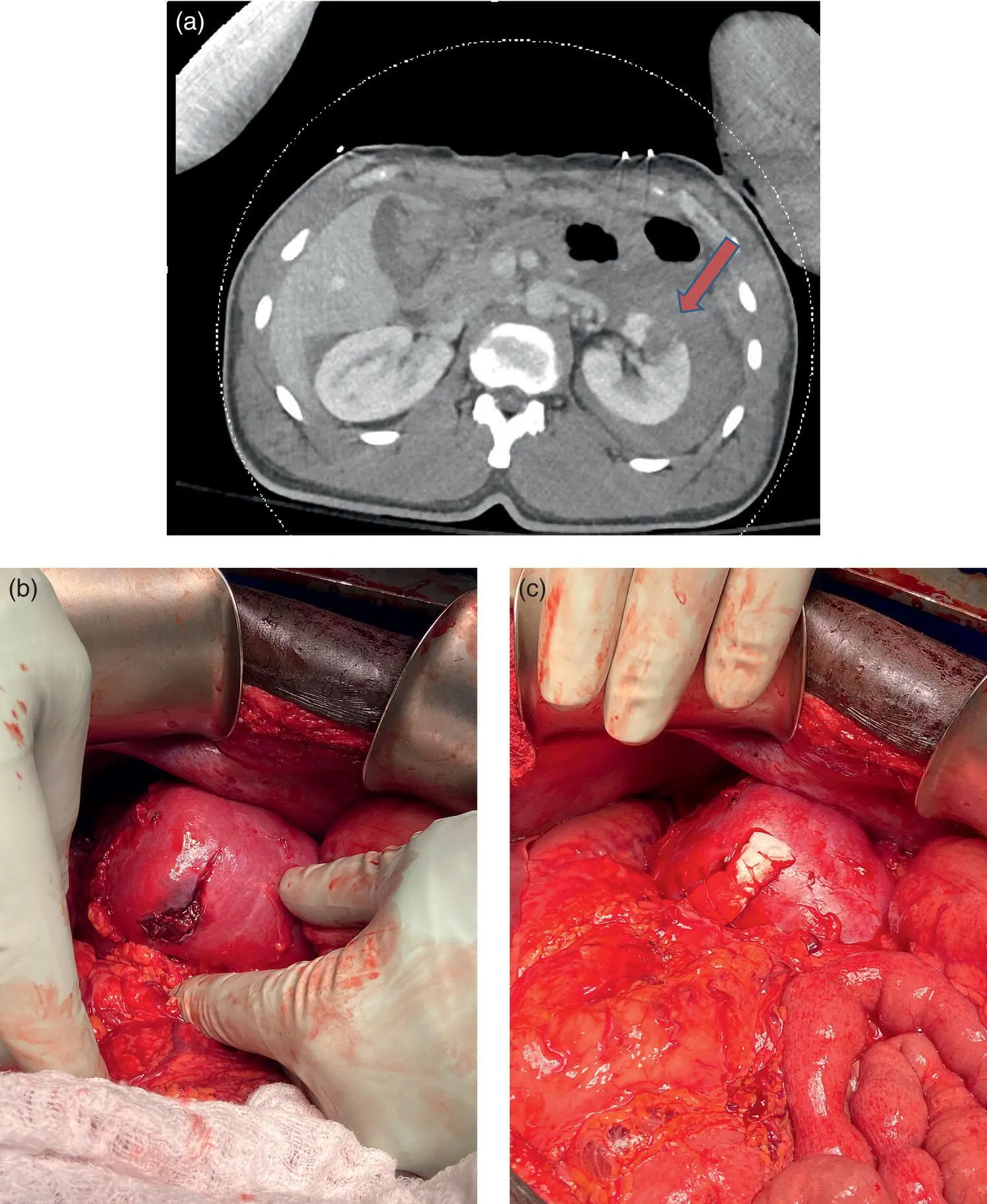
Figure 2.6 Forty‐four‐year‐old male who sustained a GSW with a grade III left renal laceration. While undergoing exploratory laparotomy for multiple abdominal organ injuries, the urology service was consulted for management of his renal injury. (a) Pre‐operative CT scan demonstrated a left grade III renal injury without collecting system injury (delayed imaging not shown). (b) Intra‐operative photo showing the anterior‐medial renal laceration. (c) This was repaired by renorrhaphy. Final appearance shows interrupted 4‐0Vicryl sutures over a Gelfoam ®bolster.
Source: photo courtesy of Alexander Skokan, MD, University of Washington.
Indications for nephrectomy include an unreconstructable kidney, significant vascular injury, or an unstable patient who cannot tolerate an attempted repair. In the civilian trauma literature, the nephrectomy rate for PRI ranges from 19 to 31% [8, 41, 42].
For the recent military conflicts in the Middle East, renal trauma comprised 29.6% of the GU injuries, with a 65.5% nephrectomy rate [13, 43]. These rates are much higher than civilian penetrating trauma and seem dissonant with the protective effects of body armor. These high nephrectomy rates are driven by two variables unique to expeditionary medicine: (i) high kinetic energy weapons, such as assault rifles and improvised explosive devices which rendered the majority of the kidneys unreconstructable; and (ii) the unique logistical limitations of battlefield to intercontinental evacuation. The combat damage control paradigm involves up to 10 stages to allow for battlefield evacuation, multiple surgeries and resuscitations, and intercontinental transport, which may contribute to higher nephrectomy rates independent of the mechanistic differences of the PRI [44]. Furthermore, expeditionary surgical teams do not have the same access to resources such as blood products and intensivists. These factors contribute to more aggressive measures to gain definitive hemodynamic stability, even in light of damage control principles.
Complications
Persistent urinary extravasation can lead to urinoma and perinephric abscesses. These can be managed using maximal drainage with the placement of an internal ureteral stent and percutaneous drainage of the abscess or urinoma. Stents are usually left for six weeks with at least seven days of Foley catheter drainage to prevent reflux of urine during voiding [45].
Delayed renal bleeding can occur in up to 23.5% of patients who undergo NOM [46]. This usually occurs within the first seven days after injury and the majority of these cases can be managed by angiography with embolization. Renin‐mediated hypertension (Page kidney) from chronic ischemia or compressive hematoma is rare.
Conclusion
During his analysis of GU trauma during World War II, Army urologist and veteran James Kimbrough stated that “conservative treatment has proved sufficient in renal damage [47].” Indeed, the management pendulum of penetrating renal trauma seems to be returning to what was discovered during the two World Wars. Urologists must be prepared with a treatment algorithm should patients fail NOM or have complications, including renorrhaphy and nephrectomy.
References
1 1 Centers for Disease Control and Prevention (2017). “Injury Prevention & Control: Data & Statistics.”. https://www.cdc.gov/injury/wisqars/pdf/leading_causes_of_death_by_age_group_2017‐508.pdf.
2 2 World Health Organization (2014). “Injuries and Violence: The Facts.” http://www.who.int/violence:injury_prevention/media/news/2015/Injury_violence:facts_2014/en.
3 3 World Health Organization (2004). “The Global Burden of Disease: 2004 Update.” doi: https://doi.org/10.1016/S0140‐6736(02)51408‐2.
4 4 Meng, M.V., Brandes, S.B., and McAninch, J.W. (1999). Renal trauma: indications and techniques for surgical exploration. World Journal of Urology 17 (2): 71–77. https://doi.org/10.1007/s003450050109.
5 5 Smith, J., Caldwell, E., D'Amours, S. et al. (2005). Abdominal trauma: a disease in evolution. ANZ Journal of Surgery 75 (9): 790–794. https://doi.org/10.1111/j.1445‐2197.2005.03524.x.
6 6 Wessells, H., Suh, D., Porter, J.R. et al. (2003). Renal injury and operative management in the United States: results of a population‐based study. Journal of Trauma 54 (3): 423–430. https://doi.org/10.1097/01.TA.0000051932.28456.F4.
7 7 Mann, U., Zemp, L., and Rourke, K.F. (2019). Contemporary management of renal trauma in Canada: a 10‐year experience at a level 1 trauma centre. Canadian Urological Association Journal 13 (6): E177–E182. https://doi.org/10.5489/cuaj.5581.
8 8 Salem, M.S., Urry, R.J., Kong, V.Y. et al. Traumatic renal injury: five‐year experience at a major trauma centre in South Africa. Injury 51 (1): 39–44. https://doi.org/10.1016/j.injury.2019.10.034.
9 9 Colaco, M., Navarrete, R.A., MacDonald, S.M. et al. (2019). Nationwide procedural trends for renal trauma management. Annals of Surgery 269 (2): 367–369. https://doi.org/10.1097/SLA.0000000000002475.
10 10 Young, H.H. (1942). Wounds of urogenital tract in modern warfare. Journal of Urology 47 (2): 59–108. https://doi.org/10.1016/s0022‐5347(17)70776‐8.
11 11 Nnamani, N.S., Janak, J.C., Hudak, S.J. et al. Genitourinary injuries and extremity amputation in operations enduring freedom and Iraqi freedom: early findings from the Trauma Outcomes and Urogenital Health (TOUGH) Project. Journal of Trauma and Acute Care Surgery 81 (5): S95–S99. https://doi.org/10.1097/TA.0000000000001122.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «A Clinical Guide to Urologic Emergencies»
Представляем Вашему вниманию похожие книги на «A Clinical Guide to Urologic Emergencies» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «A Clinical Guide to Urologic Emergencies» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.