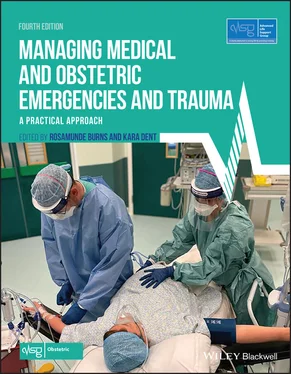
1 Cover
2 Title Page Managing Medical and Obstetric Emergencies and Trauma A Practical Approach FOURTH EDITION Advanced Life Support Group EDITED BY Rosamunde Burns Kara Dent
3 Copyright Page
4 Dedication
5 Working group for fourth edition
6 Contributors to fourth edition
7 Working group for third edition
8 Contributors to previous editions
9 Foreword to fourth edition
10 Preface to fourth edition
11 Acknowledgements
12 Contact details and further information Updates References On‐line feedback
13 How to use your textbookThe anytime, anywhere textbook
14 Abbreviations
15 PART 1: Introduction CHAPTER 1: Introduction CHAPTER 2: Saving mothers’ lives: lessons from the Confidential Enquiries2.1 Introduction 2.2 How the enquiries work 2.3 Lessons from the past 2.4 Recent lessons 2.5 Direct deaths 2.6 Indirect deaths 2.7 Coincidental deaths 2.8 Quality of care 2.9 The international dimension 2.10 Summary 2.11 Further reading CHAPTER 3: Structured approach to emergencies in the obstetric patient 3.1 Introduction 3.2 Resuscitation 3.3 Definitive care 3.4 Summary CHAPTER 4: Human factors 4.1 Introduction 4.2 Extent of healthcare error 4.3 Causes of healthcare error 4.4 Human error 4.5 Learning from error 4.6 Communication 4.7 Team working, leadership and followership 4.8 Situation (or situational) awareness 4.9 Improving team and individual performance 4.10 Summary 4.11 Further reading
16 PART 2: Recognition CHAPTER 5: Recognising the seriously sick patient 5.1 Introduction 5.2 Modified early‐warning systems 5.3 Summary 5.4 Further reading Appendix 5.1 Blood gas interpretation Appendix 5.2 Radiology in the pregnant woman CHAPTER 6: Shock 6.1 Introduction 6.2 Aortocaval compression and supine hypotension syndrome 6.3 Types of shock 6.4 Symptoms and signs of shock 6.5 Principles of treatment 6.6 Summary 6.7 Further reading CHAPTER 7: Sepsis 7.1 Introduction and definition 7.2 Sepsis in pregnancy 7.3 Pathophysiology of sepsis 7.4 Microbiology 7.5 Clinical issues and presentation 7.6 Monitoring, investigations and urgent treatment 7.7 Summary 7.8 Further reading Appendix 7.1 Viral rash in pregnancy CHAPTER 8: Intravenous access andfluid replacement 8.1 Intravenous access 8.2 Alternatives to peripheral venous access 8.3 Intravenous fluid administration 8.4 Types of intravenous fluid 8.5 Clinical signs guiding fluid replacement 8.6 Fluid administration in special circumstances 8.7 Summary 8.8 Further reading CHAPTER 9: Acute cardiac disease in pregnancy 9.1 Introduction 9.2 Cardiac disease 9.3 Chest pain 9.4 Summary 9.5 Further reading
17 PART 3: Resuscitation CHAPTER 10: Airway management and ventilation 10.1 Introduction 10.2 Airway assessment 10.3 Airway management 10.4 Advanced airway techniques 10.5 Management of ventilation 10.6 Summary 10.7 Further reading Appendix 10.1 Practical procedures CHAPTER 11: Cardiopulmonary resuscitation in the pregnant patient 11.1 Introduction 11.2 Management of CPR 11.3 Follow the advanced life support algorithm 11.4 Physiological changes in pregnancy affecting resuscitation 11.5 Perimortem caesarean section 11.6 Communication, teamwork and human factors 11.7 Summary 11.8 Further reading CHAPTER 12: Amniotic fluid embolism 12.1 Introduction 12.2 Incidence of AFE 12.3 Clinical manifestations 12.4 Symptoms and signs 12.5 Diagnosis of AFE 12.6 Management of AFE 12.7 Summary 12.8 Further reading CHAPTER 13: Venous thromboembolism 13.1 Introduction 13.2 Pathophysiology of thromboembolism 13.3 Clinical presentation of pulmonary embolism 13.4 Management of thromboembolism 13.5 Investigations for patients with a possible pulmonary embolism 13.6 Treatment of thromboembolism 13.7 Summary 13.8 Further reading CHAPTER 14: Resuscitation of the neonate at birth 14.1 Introduction 14.2 Normal physiology 14.3 Pathophysiology 14.4 Equipment for newborn resuscitation 14.5 Strategy for assessing and resuscitating a neonate at birth 14.6 Laryngeal masks 14.7 Tracheal intubation 14.8 Preterm neonates 14.9 Actions in the event of poor initial response to resuscitation 14.10 Birth outside the delivery room 14.11 Communication with the parents 14.12 Summary
18 PART 4: Trauma CHAPTER 15: Introduction to trauma 15.1 Introduction 15.2 Aetiology and epidemiology 15.3 Obstetric complications of trauma 15.4 Organisation of trauma care 15.5 Trauma call timeline for a pregnant trauma patient 15.6 Damage control resusucitation 15.7 Interventional radiology 15.8 Summary 15.9 Further reading CHAPTER 16: Domestic abuse 16.1 Introduction 16.2 Domestic abuse and pregnancy 16.3 Summary 16.4 Useful contacts 16.5 Further reading CHAPTER 17: Thoracic emergencies 17.1 Introduction 17.2 Initial assessment and management of thoracic emergencies 17.3 Life‐threatening chest injuries 17.4 Potentially life‐threatening chest injuries 17.5 Summary 17.6 Further reading Appendix 17.1 Practical procedures CHAPTER 18: Abdominal trauma in pregnancy 18.1 Introduction 18.2 Trauma to the uterus 18.3 Primary survey and resuscitation 18.4 Secondary survey 18.5 Summary 18.6 Further reading CHAPTER 19: The unconscious patient 19.1 Introduction 19.2 Principles of treatment of the unconscious patient 19.3 Primary survey and resuscitation 19.4 Assessment of fetal well‐being and viability 19.5 Secondary survey 19.6 Types of head injury 19.7 Summary 19.8 Further reading CHAPTER 20: Spine and spinal cord injuries 20.1 Introduction 20.2 Immobilisation and motion restriction techniques 20.3 Evaluation of a patient with a suspected spinal injury 20.4 Principles of treatment in spinal injuries 20.5 Summary 20.6 Further reading CHAPTER 21: Musculoskeletal trauma 21.1 Introduction 21.2 Primary survey 21.3 Secondary survey 21.4 Summary 21.5 Further reading CHAPTER 22: Burns 22.1 Introduction 22.2 Pathophysiology of burns 22.3 Primary survey and resuscitation 22.4 Secondary survey 22.5 Definitive care 22.6 Summary 22.7 Further reading
19 PART 5: Other obstetric medical and surgical emergencies CHAPTER 23: Abdominal emergencies 23.1 Introduction 23.2 Pathophysiology of abdominal pain in pregnancy 23.3 Clinical approach to diagnosis: history, examination and investigations 23.4 Clinical management of abdominal emergencies 23.5 Summary 23.6 Further reading CHAPTER 24: Diabetic emergencies 24.1 Introduction 24.2 Pathophysiology of DKA 24.3 Presentation of DKA 24.4 Treatment of DKA 24.5 Hypoglycaemia in pregnancy 24.6 Summary 24.7 Further reading CHAPTER 25: Neurological emergencies 25.1 Introduction 25.2 Headache 25.3 Primary headache 25.4 Secondary headache 25.5 Differential diagnosis of seizures in pregnancy 25.6 Acute management of a seizure 25.7 Summary 25.8 Further reading CHAPTER 26: Perinatal psychiatric illness 26.1 Introduction 26.2 Mental health problems in pregnancy 26.3 Mental health problems after delivery 26.4 Confidential Enquiries into Maternal Deaths (CEMD) 26.5 Management of mental health problems 26.6 Labour ward crises 26.7 Neonatal paediatricians 26.8 Summary 26.9 Further reading
20 PART 6: Obstetric emergencies CHAPTER 27: Pre‐eclampsia and eclampsia 27.1 Introduction 27.2 Pre‐eclampsia 27.3 Management of severe pre‐eclampsia 27.4 Management of eclampsia 27.5 HELLP syndrome 27.6 Summary 27.7 Further reading CHAPTER 28: Major obstetric haemorrhage 28.1 Introduction 28.2 Major obstetric haemorrhage (MOH) 28.3 Maternal signs of shock 28.4 Management of major obstetric haemorrhage 28.5 Patients declining blood and blood products 28.6 Summary 28.7 Further reading CHAPTER 29: Caesarean section 29.1 Introduction 29.2 Surgical technique for caesarean section 29.3 Specific difficulties encountered at caesarean section 29.4 Audit standards 29.5 Summary 29.6 Further reading CHAPTER 30: Abnormally invasive placenta and retained placenta 30.1 Introduction 30.2 Abnormally invasive placenta 30.
Читать дальше