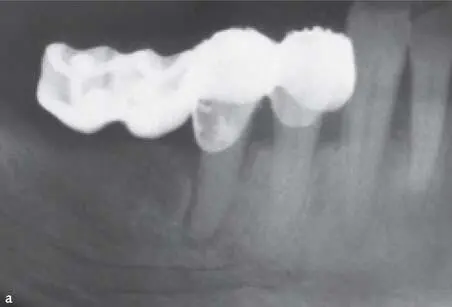
Vertical overlap
The vertical overlap is registered in millimeters. If a deep bite (Fig 1-2-12) is present it must be analyzed, whether it is a primary deep bite with a skeletal basis, or a secondary deep bite caused by a vertical collapse due to a loss of posterior teeth or significant tooth wear.

Fig 1-2-12 Partially edentulous patient with a combination of primary and secondary deep bite due to loss of molar support and significant tooth wear.
Horizontal overlap
The horizontal overlap is registered in millimeters (Fig 1-2-13).




Fig 1-2-13a to 1-2-13d Horizontal overbite can be registered by placing a finger on the buccal surface of the mandibular front teeth at the level of the incisal edge of the maxillary front teeth. The distance from the incisal edge of the mandibular teeth to the finger position, representing the overbite, can then be measured in millimeters with a periodontal probe.
Interocclusal rest space
The interocclusal rest space is evaluated. The normal distance between the occluding surfaces of the maxillary and mandibular teeth in resting position should be around 3 mm.
Crowding
Crowding of teeth and teeth that are in a reverse articulation (cross-bite) or out of occlusion (scissor bite) should be noted (Fig 1-2-14).

Fig 1-2-14 Patient with deep bite and premolars that are out of occlusion or in so-called scissor bite. A significant increase of the vertical dimension of the occlusion (VOD) is needed to restore this sextant.
Parafunctions
Any signs of bruxism or parafunctions should be evaluated and registered (Fig 1-2-15). Furthermore, signs of trauma from occlusion and the possible etiology should be evaluated. The manifestation of trauma from occlusion can be diagnosed through functional disturbances, through changes in the hard structure of teeth or through periodontal changes. Embodiment of trauma from occlusion on tooth structure can be excessive mechanical tooth wear, both attrition and abfraction, or even tooth fractures. The periodontal changes can be progressive tooth mobility due to widening of the periodontal ligament, dull percussion sound, soreness of teeth, tipping of teeth, root resorption, or hypercementosis.

Fig 1-2-15 Patient suffering from significant tooth wear due to bruxism and parafunctions.
Tooth mobility
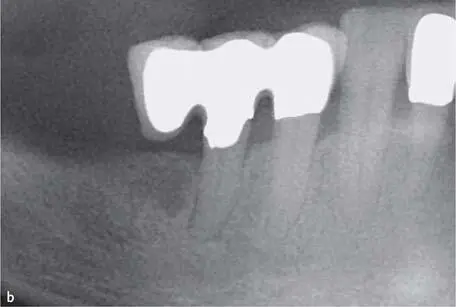
The etiology of increased tooth mobility has to be addressed. The most frequent reason for increased tooth mobility is reduced bone support due to periodontal disease. Other factors that can cause increased mobility are: occlusal trauma with widening of the periodontal ligament; overload due to poorly designed restorations (Fig 1-2-16); trauma, periodontal abscesses; orthodontic treatment; tumors; or combination of different factors.
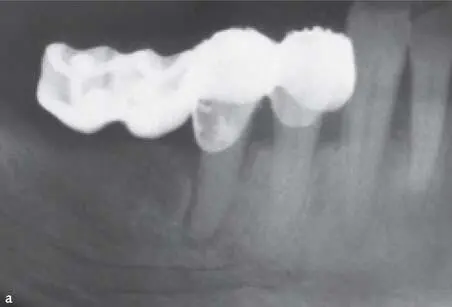
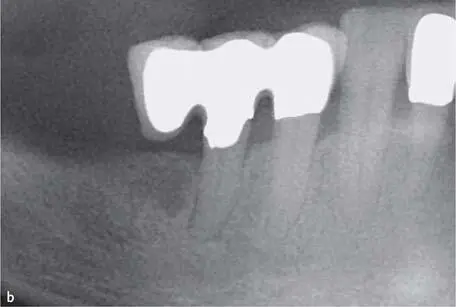

Fig 1-2-16a to 1-2-16c Overload due to extensive cantilever units, causing widening of the periodontal ligament of tooth 45 and increased mobility of the restoration. The problem disappeared after redesigning the restoration with a smaller cantilever unit that only had occlusal contact in MIP and without contact in lateral movements.
Temporomandibular disorders
The diagnosis of temporomandibular disorder (TMD) is based largely on history and physical examination findings. The symptoms of TMD are often associated with jaw movement (eg, opening and closing the mouth, chewing) and pain in the pre-auricular, masseter, or temporalis regions. Another source of orofacial pain should be suspected if the pain is not affected by jaw movement. Adventitious sounds of the jaw such as clicking or crepitus may occur with TMD, but do also occur in asymptomatic patients. The most common presenting signs and symptoms of TMD were facial pain, ear discomfort, headache, and jaw discomfort or dysfunction. Chronic TMD is defined by pain of more than 3 months’ duration.
Clinical examination that may support the diagnosis of TMD should be performed and registered. Such examinations are: abnormal or deviation in the mandibular movement; decreased range of motion measured in millimeters or by applying the three-finger rule; tenderness of masticatory, neck or shoulder muscles; pain with dynamic loading. A clicking, crepitus, or locking of the temporomandibular joint (TMJ) may accompany joint dysfunction. A single click during opening of the mouth may be associated with an anterior disc displacement. A second click during closure of the mouth results in recapture of the displaced disc; this condition is referred to as disc displacement with reduction. When disc displacement progresses and the patient is unable to fully open the mouth (ie, the disc is blocking translation of the condyle), this condition is referred to as closed lock. Crepitus is related to articular surface disruption, which often occurs in patients with osteoarthritis.
Design
Designing the occlusal scheme is a crucial Part of the treatment plan. The decision whether or not to apply a unilateral balanced occlusion (group function) or a mutually protected occlusion (canine guidance) depends on the initial occlusal situation of the natural dentition, the presence or absence of TMD, the position and extension of the planned restoration, the planned restoration material, and if the restoration is tooth- or implant-supported. There are some principal differences between tooth- and implant-supported restorations. The proprioception of an implant is 8.8 times lower than that of a tooth 45 , 46. Hence, almost nine times more load must be applied to an implant until the patient feels the load. Teeth under occlusal load move approximately 50 µm downwards within the alveola supported by the periodontal ligament. If the same load is applied to an osseointegrated implant it does not move due to the ankylosis. Due to this, some clinicians have fabricated implant-supported restorations in slight infraocclusion. This might make sense if a partially dentate patient is restored with occluding implant-supported restorations in both jaws. However, if an implant-supported restoration that articulates with natural teeth is made in infraocclusion, the antagonist teeth will tend to extrude into contact and the implant-supported restoration will end up in contact.
Читать дальше