Dental esthetics has generally become a very important Part of well-being today 1 , 2. Patients research social media and the internet on methods of self-improvement. 3It has been shown that the improvement of dental esthetics contributes to self-improvement independent of culture or gender 1 , 2. Frequently, patients approach the dental office with a clear treatment goal in mind after having researched the internet. They won’t hesitate changing dentist to receive the desired treatment, if their current dentist is not willing to perform it due to medical/dental or other reasons. This can complicate the professional relationship with the patients today. A thesis, focusing on factors that influence the demands of patients for restorative treatment, demonstrated the importance of the relationship of confidence and competence between clinicians and dental technicians and patients 4.
Communication of the treatment goal and the individual treatment steps is crucial for the establishment of confidence between the restorative team and the patients. The discussion and the decision-making process between patients and the restorative team is simplified if the foreseen treatment goal has been visualized in the diagnostic phase, either by a conventional, manually made wax-up and set-up, or by virtual wax-ups and set-ups using CAD 5.
Hence, prior to any prosthetic treatment the patient-oriented treatment goal needs to be defined through comprehensive pre-treatment diagnostics (see also Part I, Chapter 4). Diagnostics is the key element to the execution of the treatment, the selection of the restorative material, and shared decision-making.
1.2.3 Esthetic requirements
From an esthetic point of view, the material selection depends on the color of the substrate, ie, the abutment tooth or the implant abutment, and the optical properties of the remaining dentition (technical factor, see Part I, Chapter 3).
In situations with no or only slight discoloration, all restorative materials can be used. The selection of the respective material depends more on factors like the available space and the region of the jaw (see decision trees, Part I, Chapter 12).
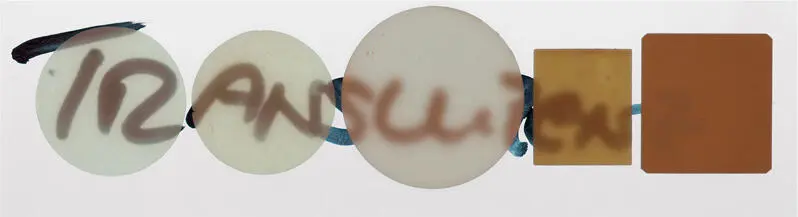
In situations with discoloration, however, the selection of the restorative material becomes more complex (Fig 1-2-1). Dental ceramics are translucent materials, and depending on the type of microstructure their translucency varies. Glass-ceramics are rather translucent and have low masking ability. In order to improve their masking ability, the thickness of the ceramic needs to be increased. Oxide ceramics have more opaque properties and, therefore, better masking quality (Fig 1-2-2).





Fig 1-2-1a to 1-2-1e Overview of different abutment teeth in the esthetic area displaying the potential differences in color of the substrate, that have to be considered at the restorative material selection.
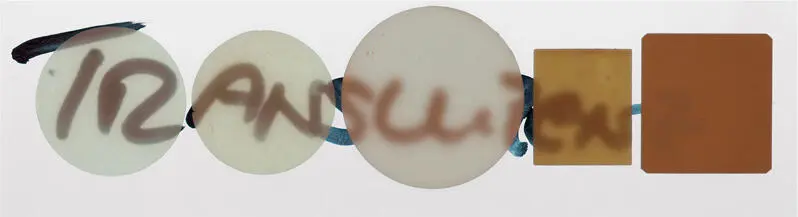
Fig 1-2-2 Translucency of different ceramic materials. From left to right; the leucite-reinforced glass-ceramic, feldspathic ceramic, zirconia, In-Ceram alumina, and In-Ceram zirconia samples have the same thickness (0.5 mm), and show obvious differences in translucency.
To mask the same discoloration different amounts of space may be required depending on the ceramic. It has been shown that a thickness of at least 1.2–1.5 mm of glass-ceramic is needed to cover dark discolorations 6. To mask discolorations with this type of ceramic induces a need for more invasive preparations. The same applies also to oxide ceramics like zirconia; however, this ceramic is also influenced by the color of the substrate and the cement used for the fixation of the restorations at thicknesses below 1 mm 7 , 8. In situations with intense dark discoloration, metal-ceramics may be the most appropriate material combination for the masking.
1.2.4 Amount and quality of tooth substance
The amount and the quality of the abutment tooth substance influence the selection of the restoration type (eg, overlay or crown), and of the respective restorative material. The conventional prosthetic treatment concepts are in transition today, shifting from full fixed/removable partial prostheses to less invasive, defect-oriented restoration types like veneers, overlays, partial crowns, or resin-bonded prostheses, where applicable.
One reason for this change of concepts is, that conventional tooth preparation for full crowns has been shown to lead to the of loss of abutment tooth vitality at rates between 2% to 4% after 5 years up to 10% at 10 years of restoration function 9 – 12(for further details see Part III). Hence, on the one hand biologic limitations exist at the tooth preparation and the amount of the tooth substance needs to be considered. On the other hand, the minimal material thickness values recommended for the respective restorative materials have to be taken into consideration. Table 1-1-1in Chapter 1summarizes the indications of the different types of restorative materials for conventional fixed partial dentures. Another reason for the change of concepts is, that significant improvements of the adhesive cementation means and methods have been made, widening the indications for esthetic materials that need adhesive cementation for good long-term stability 13.
The amount and the quality of the tooth substance have to be evaluated during treatment planning as Part of the decision-making process, influencing the type of restoration and the restorative material (including its fixation).
Amount of tooth substance
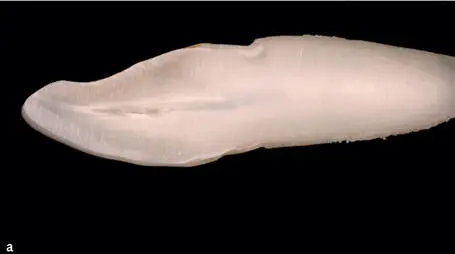
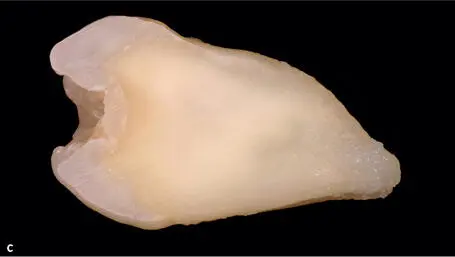
The mean thickness of the enamel and dentin, eg, at sound central incisors, varies between 1.8 mm for 10–19-year-old patients to 3.1 mm for 60-year-old patients 14(Fig 1-2-3).
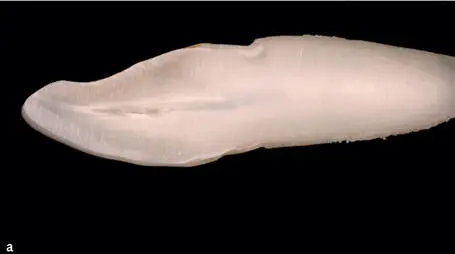

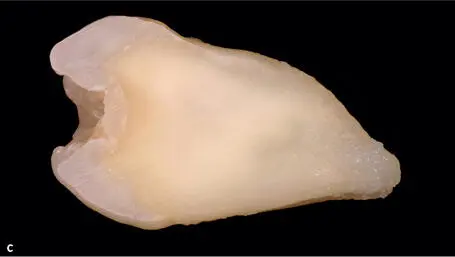
Fig 1-2-3a to 1-2-3c Cross-sections of anterior and posterior teeth, displaying the differences of the amounts of dentin and enamel surrounding the pulpal chambers.
A histologic investigation has examined the minimal thickness of dentin needed to avoid pulpal damage at different amounts of abutment tooth preparations 15. The researchers included vital teeth with poor prognosis in this investigation foreseen for extraction, and full-crown preparations were performed. Thereafter, the teeth were extracted and the pulpal tissues histologically examined. A correlation between the degradation of the pulpal tissues and the remaining thickness of the dentin after tooth preparation was performed. The study showed that a minimum remaining amount of dentin of 1 mm was crucial in order to avoid pulpal damage at tooth preparation. As a consequence, to avoid damage to the pulp a maximum of 0.7 mm (young patients) and up to 2.1 mm (elders) of (sound) tooth substance may be removed for restorative purposes. These values apply for sound healthy teeth which under normal conditions would not need to be restored. Still, the biologic limitations need to be considered when performing tooth preparations for restorative purposes.
Читать дальше