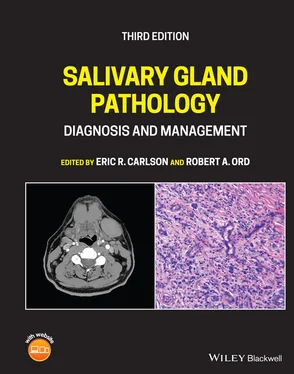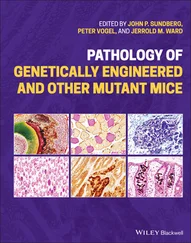
Figure 3.7. Axial (a) and coronal (b) CT scans of a patient with a hospital acquired parotitis. The degree of swelling led to the acquisition of these scans to rule out intraparotid abscess. No abscess was identified, thereby not requiring incision and drainage in this patient.
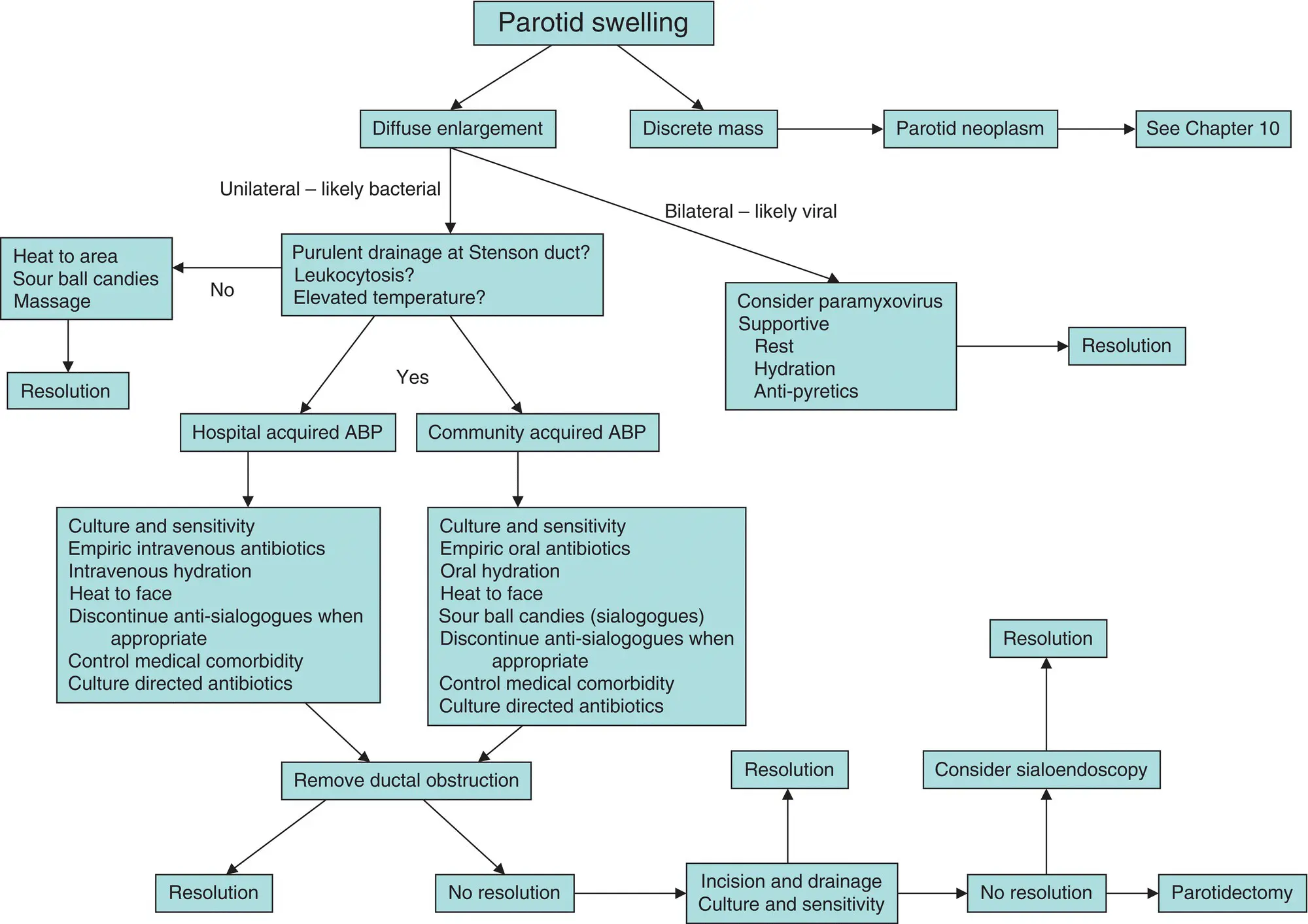
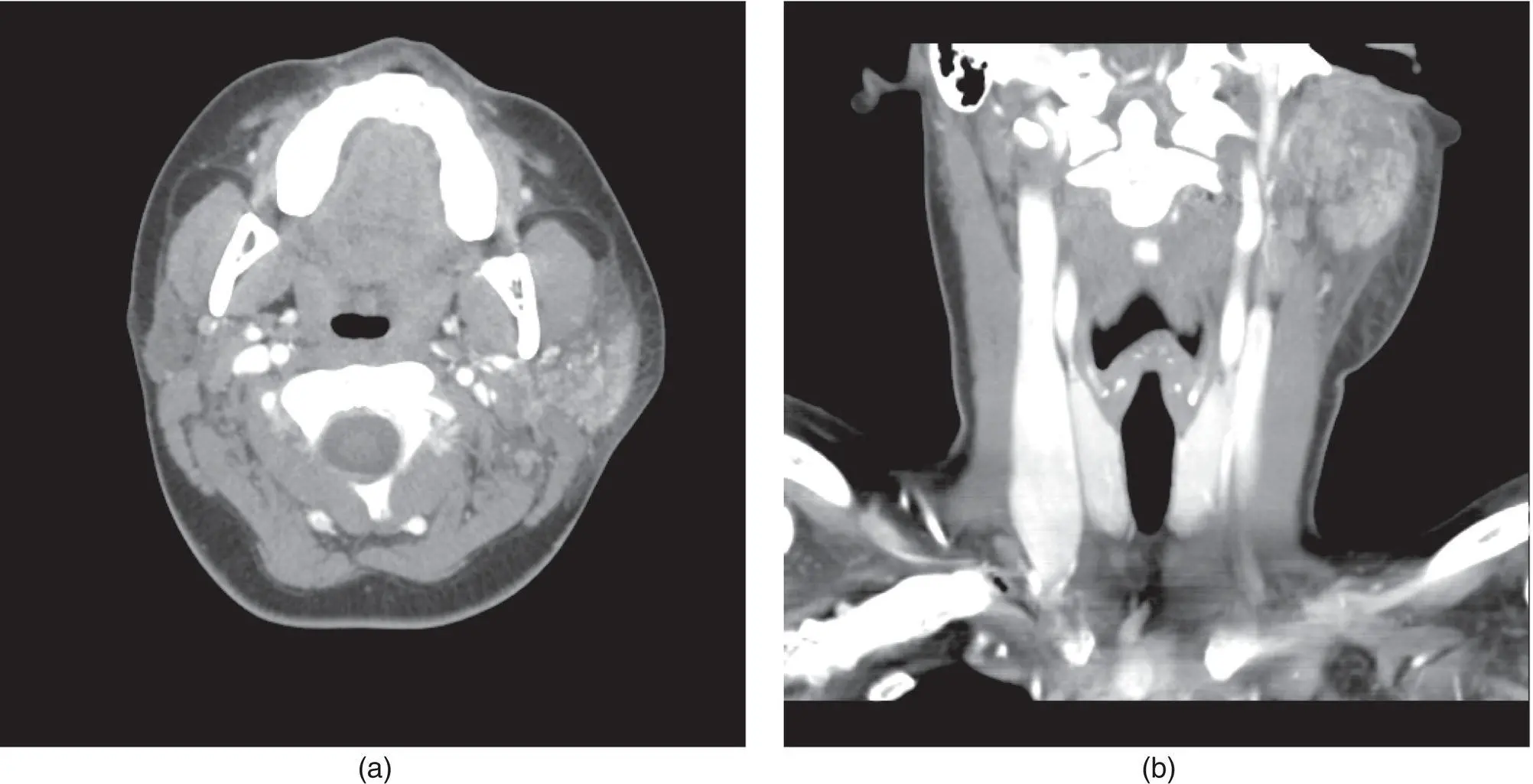
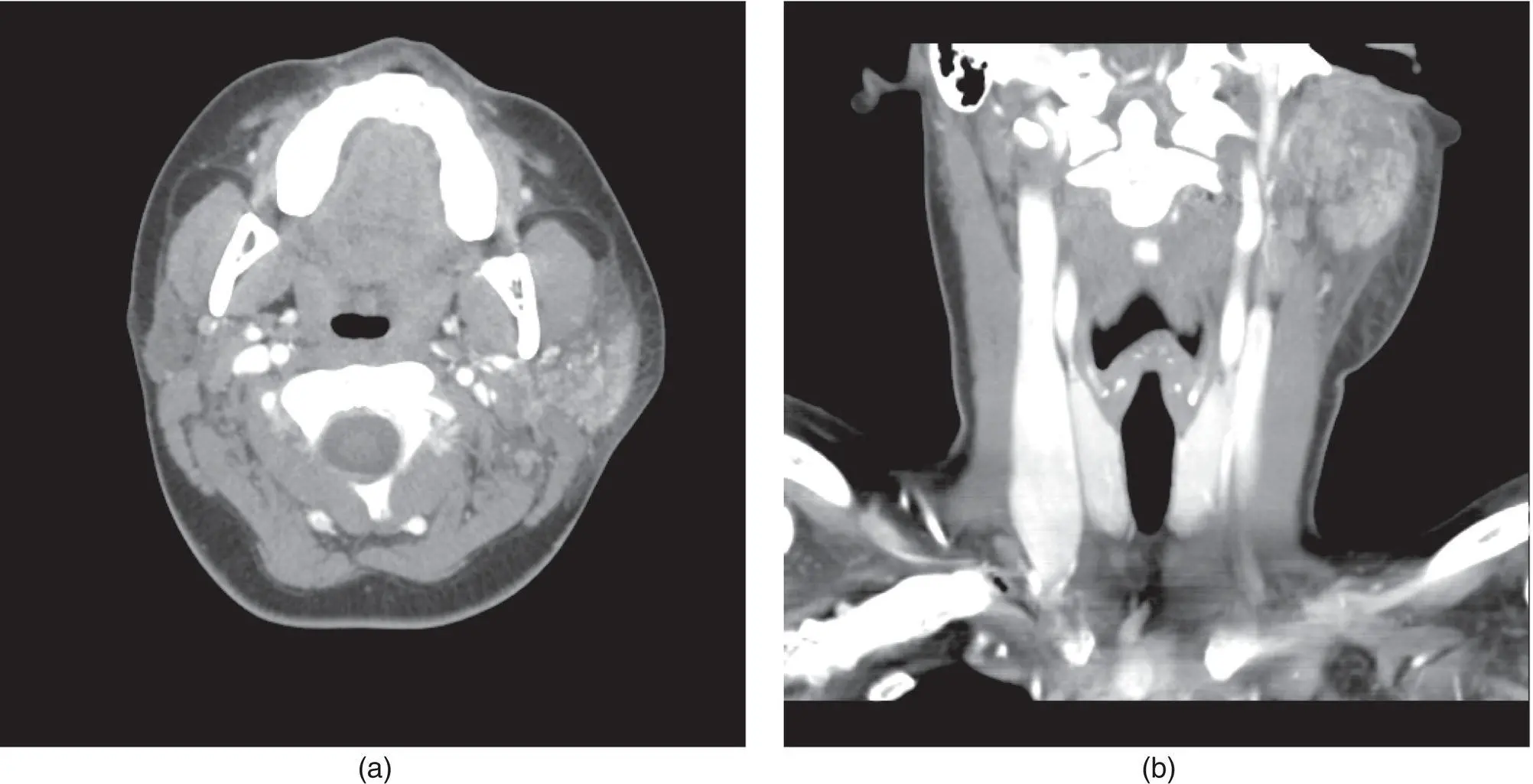
Figure 3.8. The algorithm for diagnosis and treatment of a unilateral or bilateral parotid swelling.
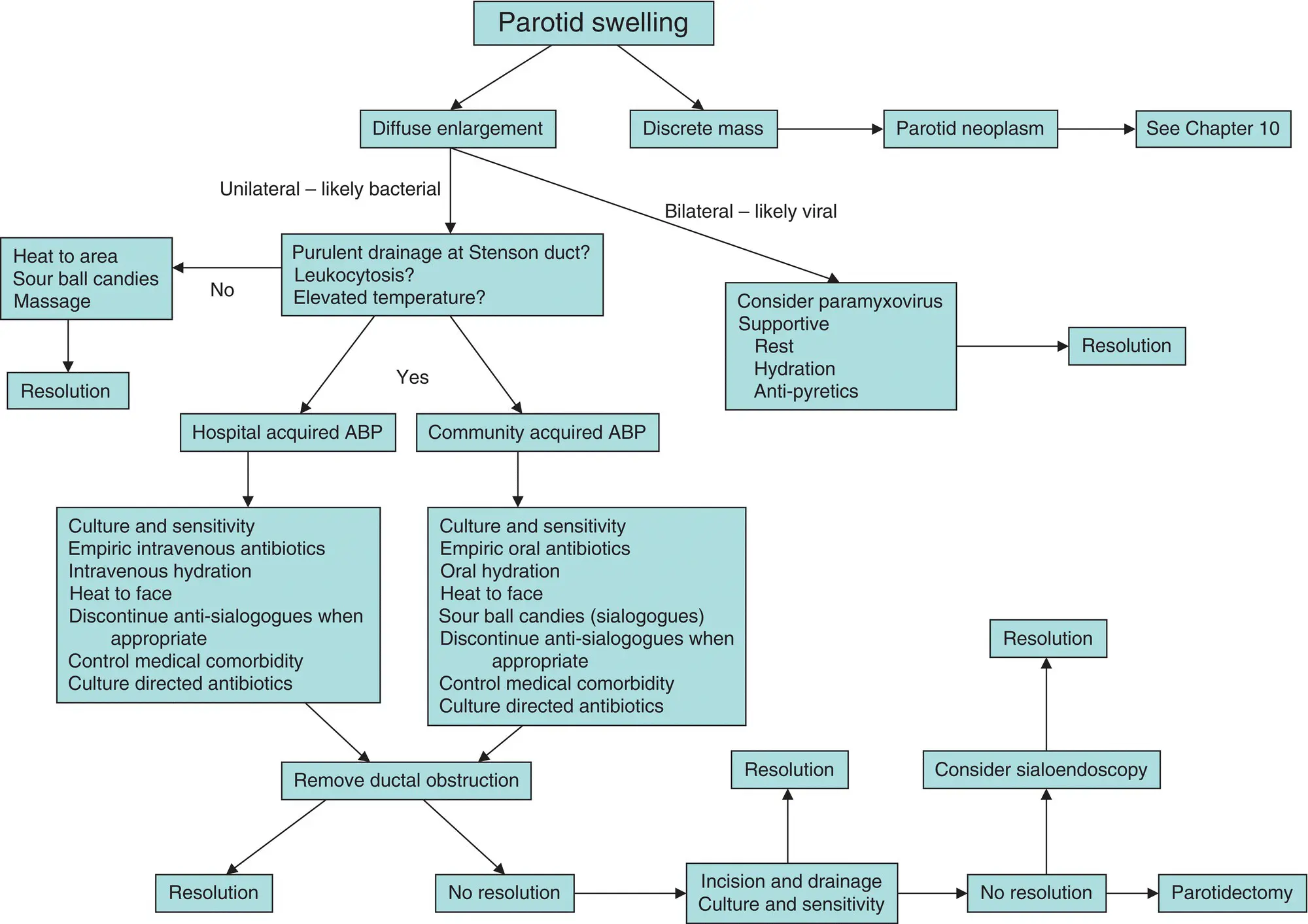
Imaging of outpatients with community acquired ABP is based on the severity of the clinical disease, its chronicity, and the clinician's suspicion for intraparotid abscess. Obtaining routine plain films, such as a panoramic radiograph, is certainly indicated to investigate for the presence of a sialolith. It may be acceptable, however, to defer special imaging studies in these patients until refractory infection develops. Patients with severe symptoms, fever, and concern for abscess formation within the parotid gland should be imaged with CT scans in an expedient fashion ( Figures 3.7and 3.9). Except in the presence of severe immunosuppression or other medical comorbidity, refractory infections are uncommonly seen in ABP.
The general principles of the management of hospital acquired ABP are identical to those of the community acquired ABP. As previously described, however, the risk factors differ. In these inpatients, rehydration should be performed with caution to avoid cardiac overload. Empiric intravenous antibiotics should be instituted in these patients, and confirmed as to their efficacy with culture and sensitivity of purulent parotid exudates whenever possible. The use of heat to the affected gland is appropriate in this setting, as well. The inpatient should be monitored closely for clinical improvement. Despite the institution of conservative measures, if the patient's course deteriorates within 48–72 hours as evident by increased swelling and pain, or an increase in white blood cell count, an incision and drainage procedure is indicated ( Figure 3.9). Such a procedure must be guided by CT scans to explore all loculations of pus. A needle aspiration of a parotid abscess is unlikely to represent a definitive drainage procedure, although it will permit the procurement of a sample of pus prior to instituting antibiotic therapy in preparation for incision and drainage.
CHRONIC (RECURRENT OR REFRACTORY) BACTERIAL PAROTITIS
Chronic bacterial parotitis occurs in at least three clinical settings. The first is in which the patient defers evaluation such that the condition has persisted for at least one month. The second includes the setting in which acute bacterial parotitis was managed conservatively, but without resolution (refractory sialadenitis). Finally, it is possible for a successfully treated parotitis to become recurrent such that periods of remission separate recurrent episodes of ABP. The parotid gland may demonstrate evidence of latent infection despite clinical resolution of the disease. The result is scarring in the gland such that function is impaired. Histology will show dilation of glandular ducts, abscess formation, and atrophy (Patey 1965). Pus is rarely observed in chronic bacterial parotitis (Baurmash 2004). Rather, there is a marked reduction of salivary flow, and the parotid secretions are viscous and milky in appearance. The microbiologic etiology of chronic bacterial parotitis is most commonly streptococci and staphylococci, but other organisms may be found as a function of the patient's immune status, the setting in which the parotitis originally occurred, and medical comorbidity. It has been suggested that the accumulation of a semisolid material that obstructs the parotid duct is the culprit in chronic bacterial parotitis (Baurmash 2004). The clinical course of the disease shows pain and swelling waxing and waning. As with acute bacterial parotitis, a screening panoramic radiograph or CT scans should be obtained to rule out the presence of a sialolith (Carlson 2009).
Treatment of Chronic Bacterial Parotitis
Treatment of chronic bacterial parotitis centers on palliative therapy with parotidectomy reserved as a last resort ( Figure 3.10). Effective treatment is centered on the gland inflammation as well as the precipitated intraductal material. Patients should be treated with culture‐specific systemic antibiotics, ductal antibiotic irrigations during periods of remission, analgesics, and avoidance of dehydration and anti‐sialogogue medications (Goldberg and Bevilacqua 1995). The identification of a sialolith should result in expedient removal. Sialendoscopy represents a technique that may obviate the need for aggressive surgical intervention (Nahlieli et al. 2006; Hasson 2007). Sialendoscopy is a minimally invasive procedure with a low rate of complications. A Danish study published in 2016 demonstrated a 26% reduction in the number of salivary gland excisions for benign processes after the introduction of sialendoscopy in 2004 compared to the five years prior (Rasmussen et al. 2016). Sialendoscopic findings of patients with chronic obstructive parotitis include ductal stricture, mucous plugs, and desquamative epithelial cells and inflammatory cells (Qi et al. 2005). A sialendoscopic procedure may address any or all of these problems, thereby sparing the gland ( Figure 3.11). If pain and swelling become intolerable for the patient, or if special imaging studies reveal abscess formation in the parotid gland, then nerve sparing parotidectomy is the treatment of choice ( Figure 3.12)
van der Lans et al. (2019) retrospectively reviewed 46 parotidectomies performed on 37 patients with chronic bacterial parotitis. Total parotidectomy was performed in 41 cases (89%) and superficial parotidectomy was performed in 5 cases (11%). No information was included in this report regarding the chronicity of symptoms, nor the type of symptoms in their cohort. Temporary paresis of the facial nerve was noted in 12 operations (26%) with a mean duration of 7.7 weeks, with no incidence of permanent paresis. Frey syndrome was noted after 20 parotidectomies. Recurrence of the parotitis was noted in six cases (15%) and was successfully treated with conservative measures in four patients. The authors concluded that parotidectomy is a safe and effective means to resolve chronic recurrent parotitis. These authors did not find differences in resolution of disease between superficial parotidectomy and total parotidectomy. Therein, they indicated that successful treatment is realized in removal of as much affected glandular tissue as possible while identifying and preserving the facial nerve.

Figure 3.9. A left facial abscess in a 45‐year‐old man with a two‐week history of left facial swelling and pain (a). Computerized tomograms (b and c) demonstrate an abscess within the tail of the left parotid gland. The patient underwent incision and drainage (d) in the operating room for a diagnosis of community acquired acute bacterial parotitis with abscess formation. Methicillin‐resistant Staphylococcus aureus species were cultured. He showed resolution of his disease at two months postoperatively (e and f).
Читать дальше