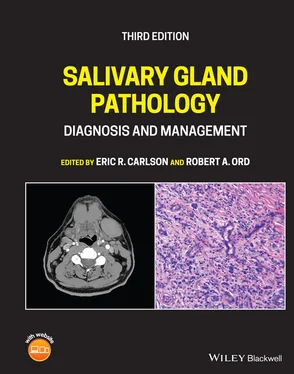
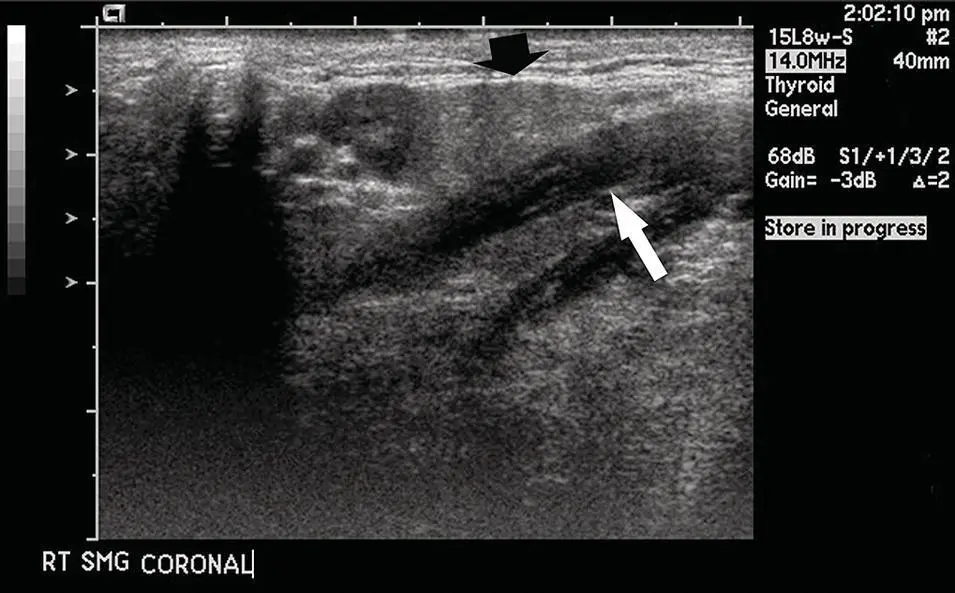
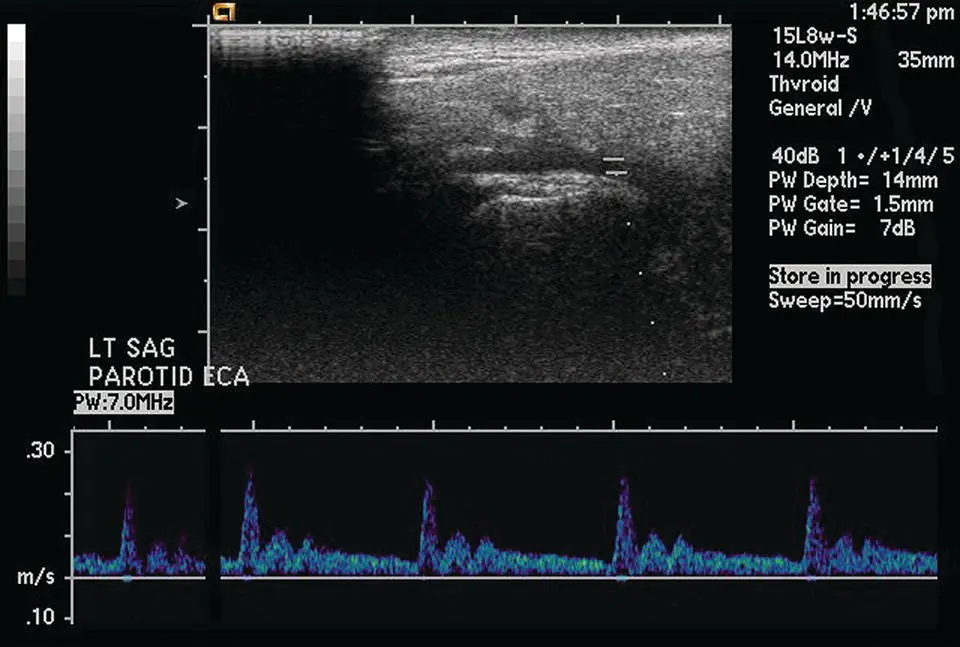
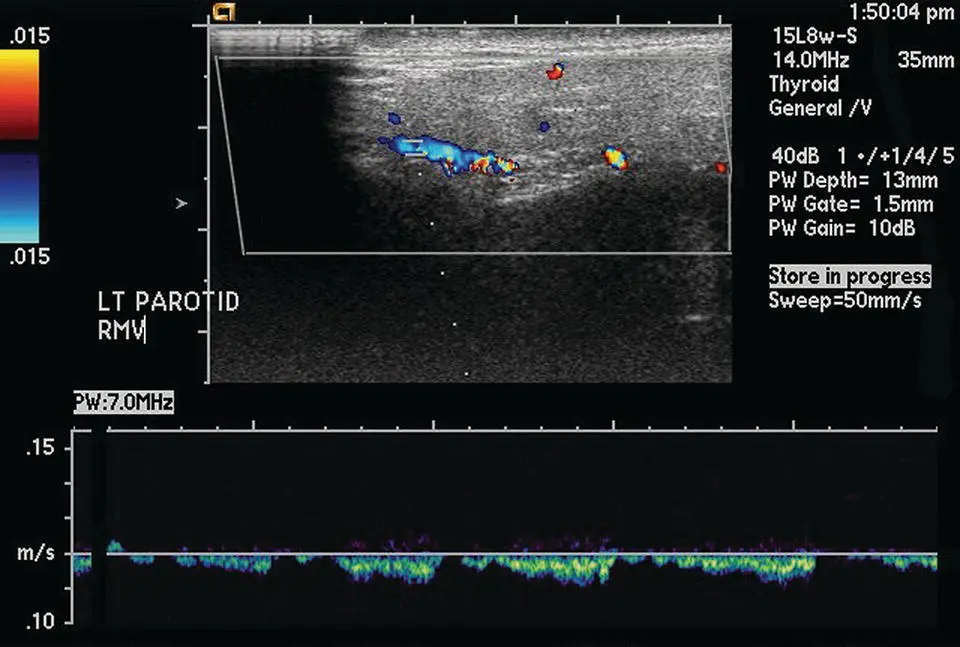
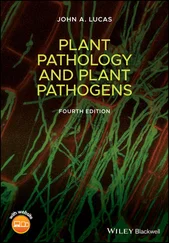
Ultrasound is performed infrequently for head and neck imaging relative to CT and MRI. Although US can depict normal anatomy and pathology in the major salivary glands, it is limited in evaluation of the deep lobe of the parotid and submandibular gland ( Figures 2.16and 2.17). US is operator dependent and takes significantly longer to perform on bilateral individual salivary glands when compared to contrast‐enhanced CT of the entire neck. US is quite effective at delineating cystic from solid masses, and determining degree of vascularity. US can be used to image calculi and observe the resulting ductal dilatation. Normal lymph nodes and lymphadenopathy can also be reliably distinguished. US can be used to initially stage disease. It is not, however, optimal for post‐therapy follow‐up, be it radiation or surgery. When compared with CT or MRI, US significantly lacks in soft‐tissue resolution and contrast. Because of its real‐time imaging capability and ease of handheld imaging, US is quite good at image‐guided fine needle aspiration and biopsy. The application of color Doppler or power Doppler US can distinguish arteries from veins, which are critical for image‐guided biopsy ( Figures 2.18and 2.19). Eighteen‐gauge core biopsies of the parotid may be safely performed under US guidance (Wan et al. 2004).
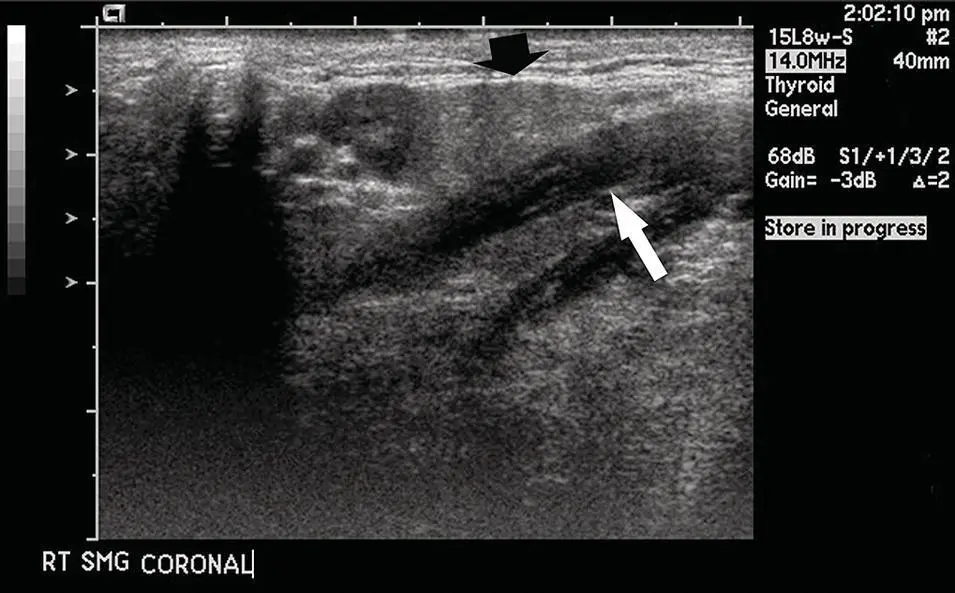
Figure 2.16. Ultrasound of the submandibular gland (black arrow) adjacent to the mylohyoid muscle (white arrow).

Figure 2.17. Ultrasound of the parotid gland demonstrating a normal intraparotid lymph node on a hyperechoic background. The lymph node is round and has a hypoechoic rim but demonstrates a fatty hyperechoic hilum (arrow).
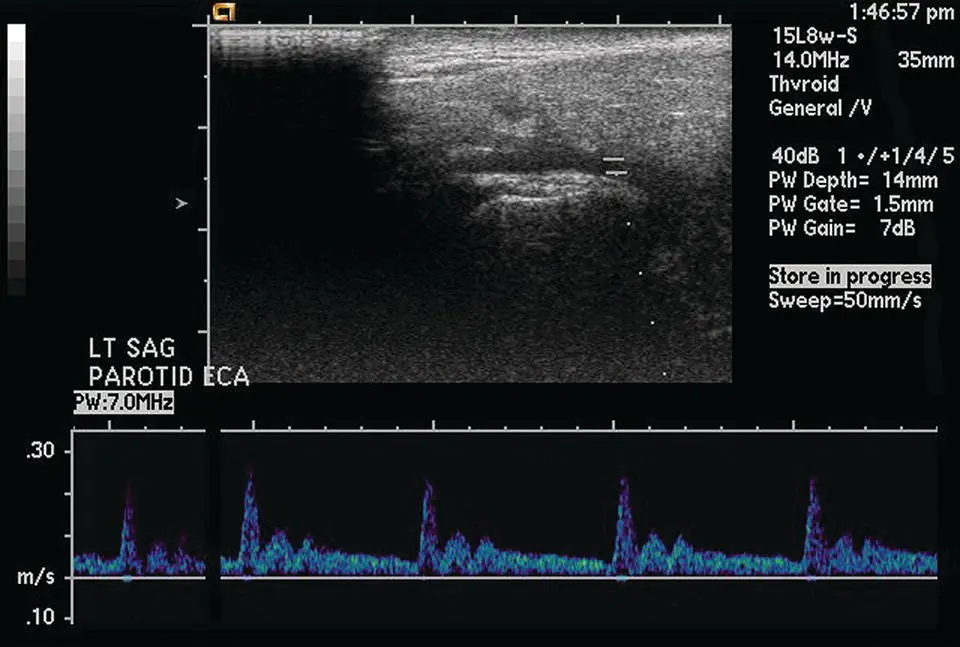
Figure 2.18. Ultrasound of the parotid gland in longitudinal orientation demonstrating the Doppler signal of the external carotid artery.
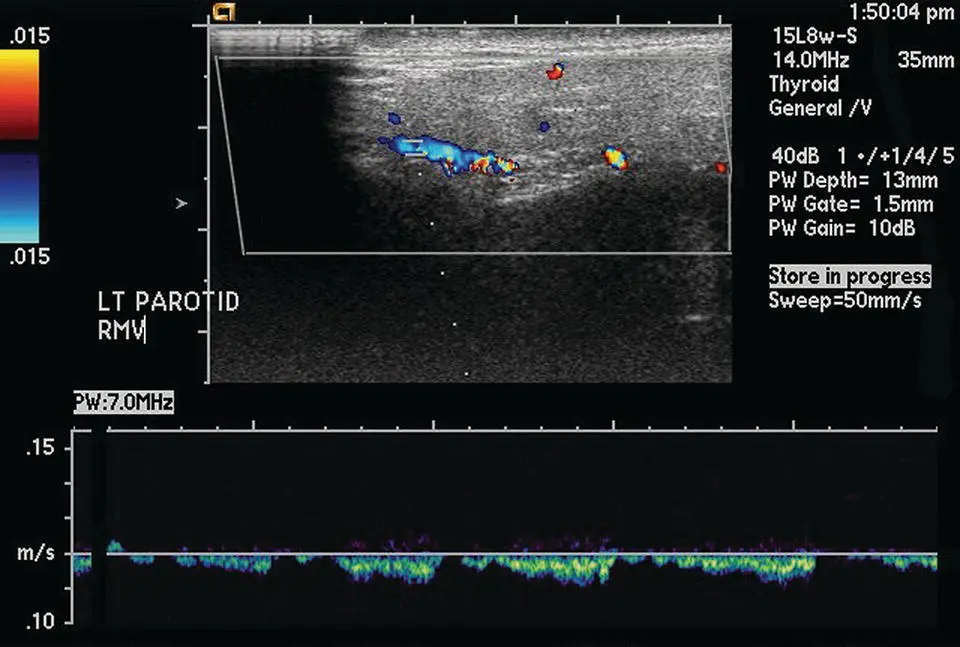
Figure 2.19. Ultrasound of the parotid gland in longitudinal orientation demonstrating the Doppler signal of the retromandibular vein.
Ultrasound (US) Technique
High‐frequency transducers such as 5, 7.5, or 10 MHz are typically applied to image superficial small parts. Real‐time imaging and image acquisition are performed by a technologist or physician. Doppler US may be applied to observe the vascularity of the glands (increased in inflammatory conditions) or tumors within the glands. Doppler US can easily determine arterial from venous channels.
Invasive salivary gland imaging was first introduced in 1904 when mercury was injected into surgical pathology and autopsy specimens. These injected tissue specimens were then visualized by X‐rays. Sialography development continued, and in 1925 potassium iodide solution was injected into a human parotid gland, thereby initiating the radiographic technique of human sialography. Many modifications of sialography have been introduced since that time. These progressive changes brought sialography into the realm of practical salivary gland imaging. Since the advent of CT and MRI, sialography has to some extent been replaced as a diagnostic tool in salivary gland imaging. Only within the last few years has there be resurgence in its use, particularly in the diagnosis and treatment of obstructive and metabolic salivary gland disease (Mosier 2009). The specific choice of imaging depends predominately on the patient's clinical presentation as well as the patient's specific needs (Burke et al. 2011).
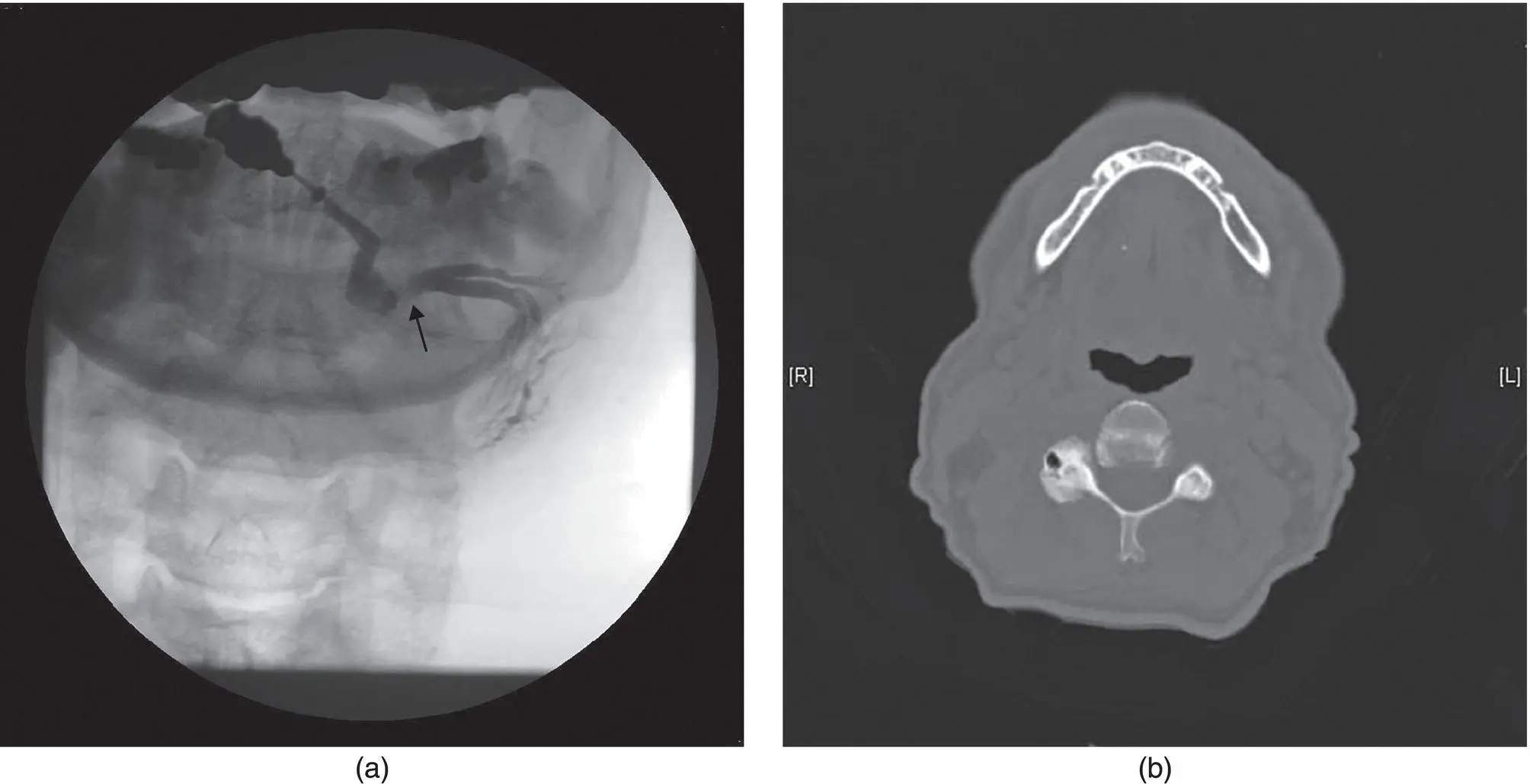
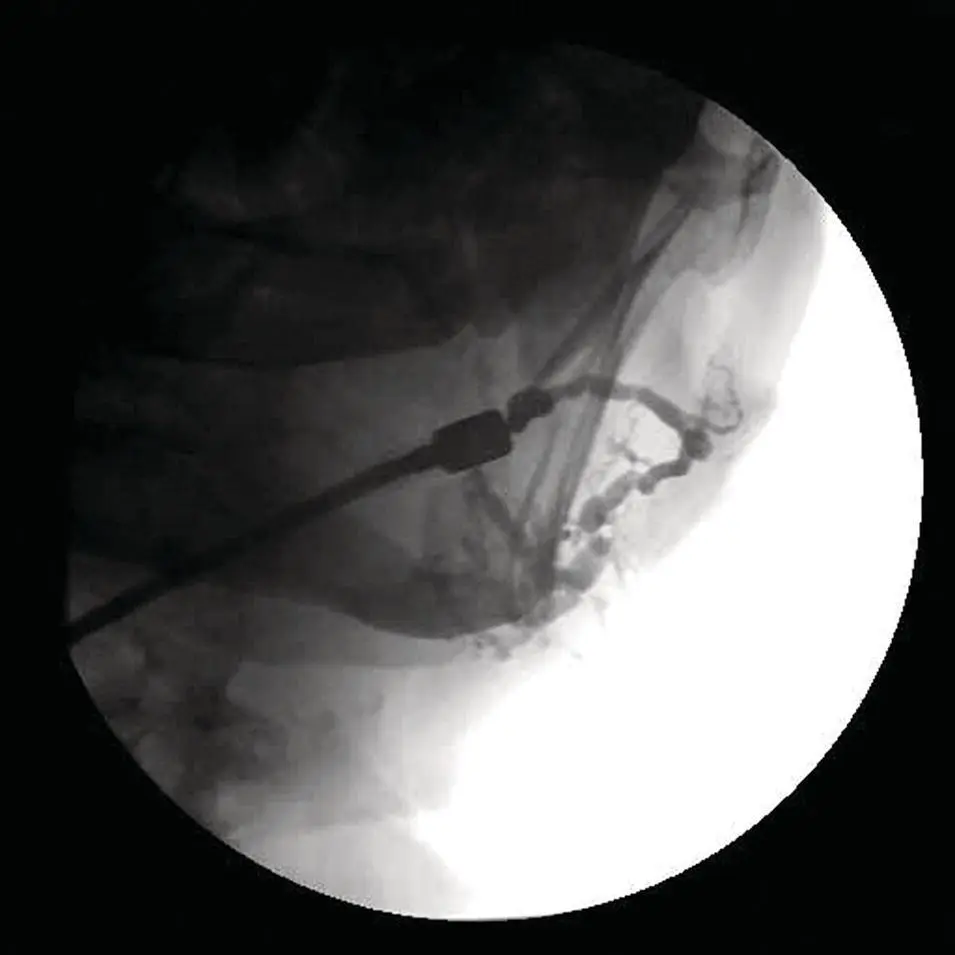
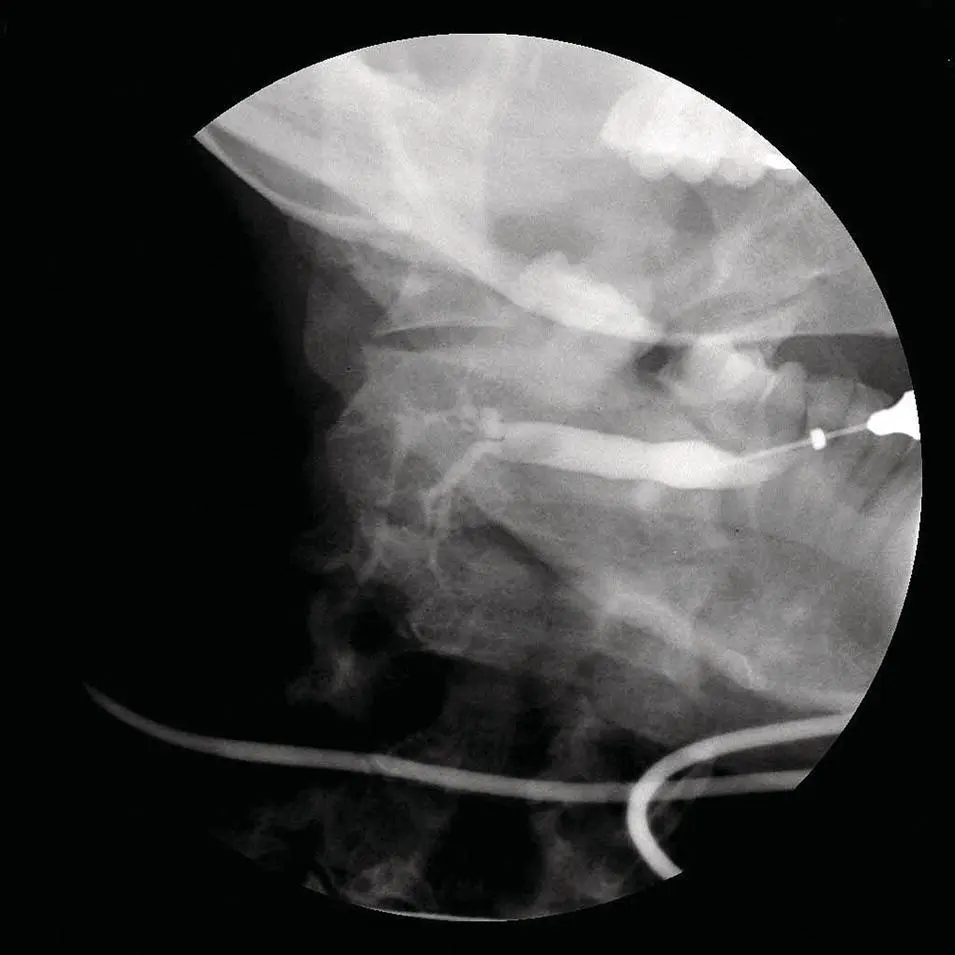
Most authorities believe the principal value of sialography is in the diagnosis of obstructive salivary gland disease. While most sialoliths are calcified and therefore opaque when visualized with X‐ray, 20% of submandibular and 40% of parotid stones are either non‐calcified or only partially calcified. Consequently, these stones are non‐opaque when examined by way of plain X‐ray and occasionally by CT imaging, as well (Sobrino‐Guijarro et al. 2013) ( Figure 2.20). Sialographic imaging was once essential in the delineation of benign and malignant masses, but imaging of such lesions has now been replaced by the more modern techniques of CT, US, and MRI. The major present‐day indications of sialography are: (i) ductal anomalies such as sialoceles or salivary fistulas, (ii) obstructive and restrictive disease ( Figure 2.21) including stones ( Figure 2.22), mucous plugs, and intraductal neoplastic or inflammatory lesions, and (iii) chronic systemic parenchymal diseases of salivary gland such as those seen with Sjögren syndrome or sarcoidosis (Hasson 2010).
The only two paired salivary glands for which conventional sialography is suitable are the parotid and the submandibular glands. Even though the anatomy of every individual gland varies with the patient being studied, each separate gland has a single primary duct that excretes saliva. It is through this solitary duct that contrast can be introduced and the various anatomic and pathologic variances be imaged.
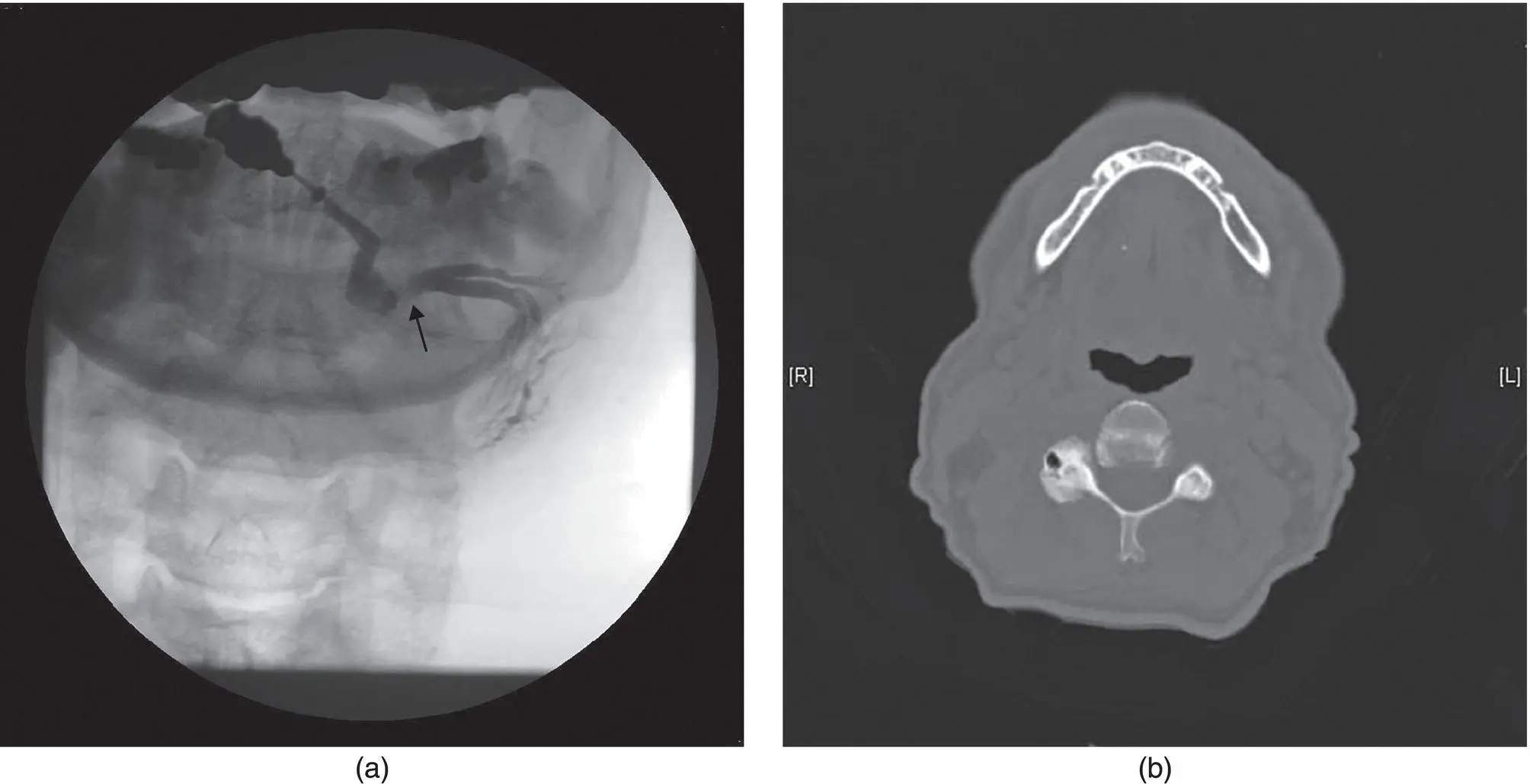
Figure 2.20. Submandibular sialogram (a). Note the continuity defect that represents a sialolith (arrow). The corresponding submandibular CT (b) demonstrates a partially calcified stone that is less impressive compared to the sialogram.
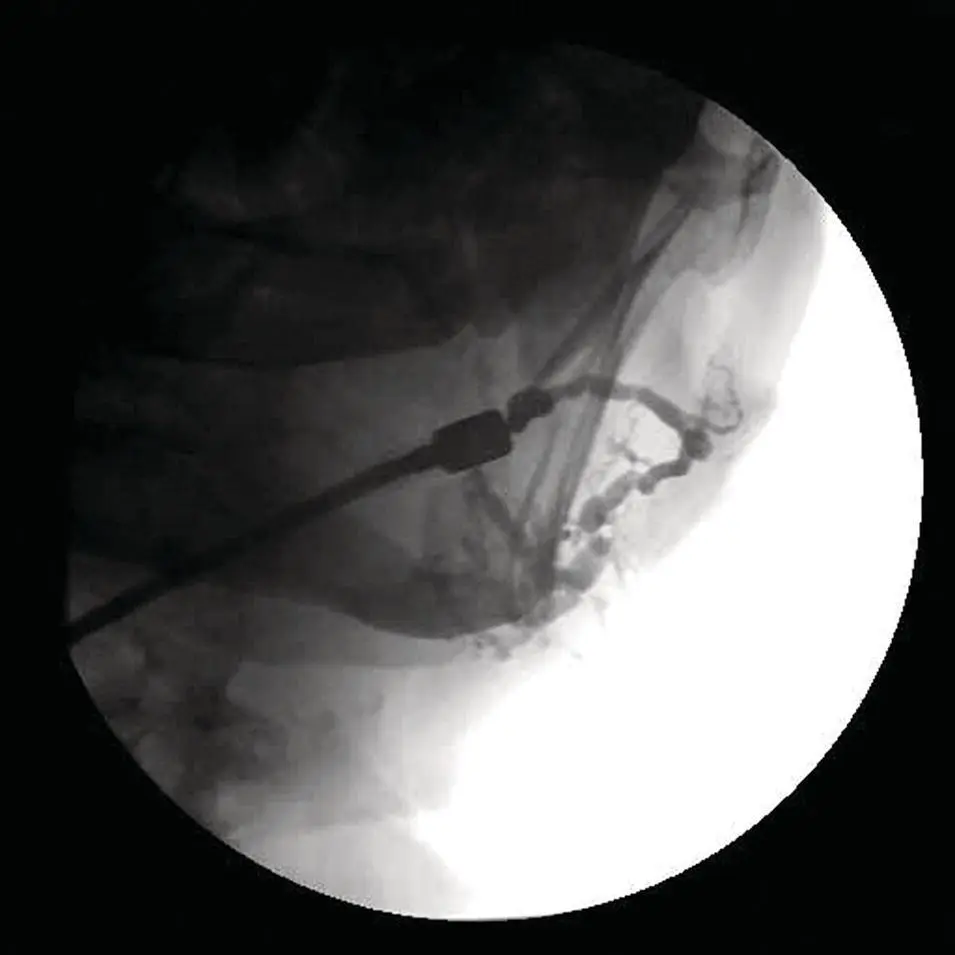
Figure 2.21. Parotid sialogram. Note the numerous areas of duct dilatation and stenosis. These features are diagnostic of obstructive disease.
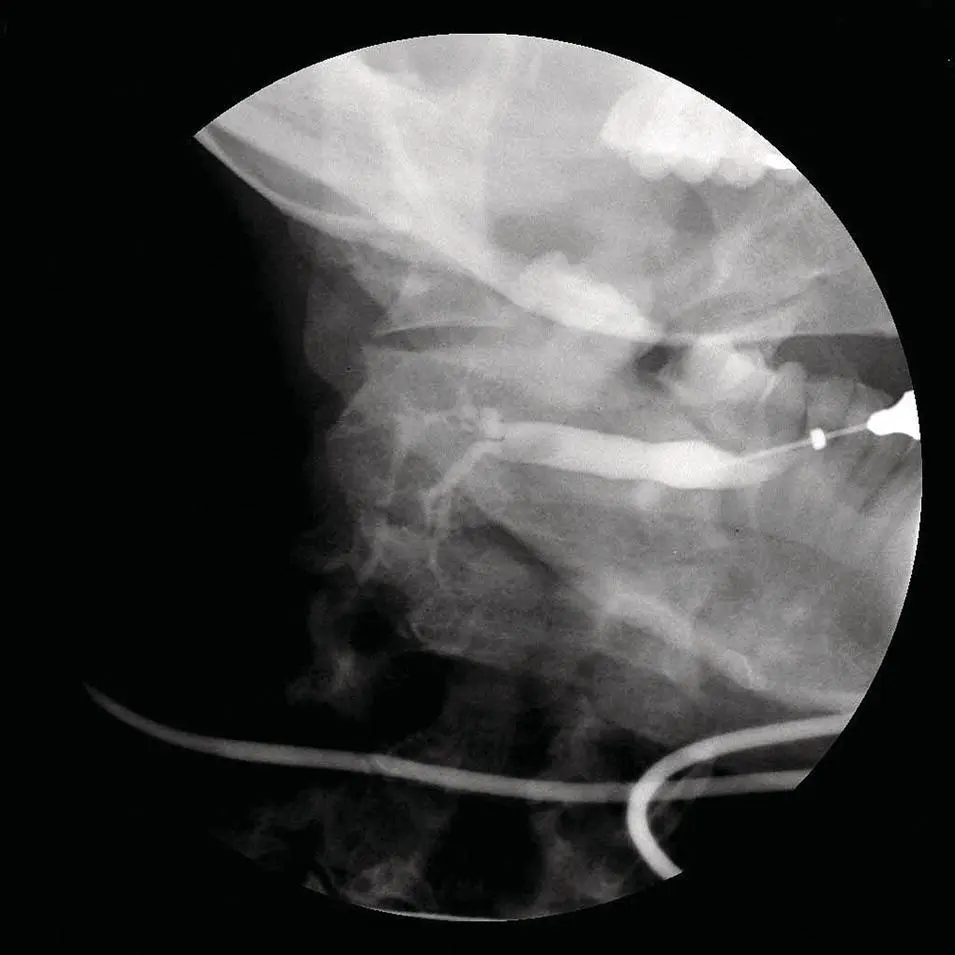
Figure 2.22. Submandibular sialogram: Note the “soft” noncalcified stone filling the duct.
Conventional sialography is a painless and minimally invasive technique that is generally quite successful. The mechanics of sialography are for the most part relatively simple. Initially, the patient is questioned regarding contrast allergies. In addition, it should be noted that the patient should not be imaged if there is evidence of an ongoing salivary gland infection, particularly acute inflammatory conditions or abscesses. Once the patient is placed supine on the examination table, they are given lemon juice to stimulate salivation. Using various sized lacrimal probes, the duct orifice is dilated for a length of 1–3 cm. Following dilation, a 23‐ to 25‐gauge catheter is placed into the main duct and 1–3 cc of contrast is infused into the gland taking great care not to damage the duct. Even though non‐water‐soluble contrast usually delineates ductal walls more distinctly, water‐soluble contrast also does quite well. In addition, the water‐soluble contrast leaves no residual opacity with which to contend thereafter. Following contrast administration, images are acquired in various views (frontal, lateral, etc.). The patient is once again given lemon juice, allowing the residual contrast to be expelled. If the patient experiences pain during the procedure, a local anesthetic such as lidocaine can be infused into the ductal system in the same manner as the contrast agent. Occasionally, radiologists will also inject corticosteroids into the primary duct, which potentially can decrease the inflammatory component of the imaging study.
Читать дальше