Alloplastic bone substitutes
Alloplastic or synthetic bone substitutes have the advantage of not bearing any risk of disease transmission and are available in large quantities. Furthermore, it is theoretically possible to specifically design these biomaterials with material characteristics that meet the requirements for a specific clinical indication. Chemistry, phase distribution between crystalline and amorphous material, crystal size, gross morphology and size, particle size, pore size and interconnectivity, macro- and nanoporosity, and surface roughness and texture at the macroscale and nanoscale can be tailored. A greater understanding of the importance of the different material characteristics has helped us to understand why materials with identical chemical compositions and macromorphologies have performed so different biologically in vivo.
The synthetic biomaterials currently on the market can be divided into three groups: calcium phosphates (CaPs), bioactive glasses, and polymers (see Fig 2-22). Of these, CaPs—and especially HA and tricalcium phosphate (TCP)—have been most intensively studied due to their composition, which closely resembles the inorganic phase of bone. 117 In general, HA is considered to be osteoconductive and nonresorbable, whereas TCP also demonstrates osteoconductive properties but resorbs rapidly. Therefore, combinations of HA and TCP—biphasic calcium phosphates (BCPs)—have been investigated with the goal of benefitting from both the stable space-keeping properties of HA and the resorbable space-making properties of TCP. 118 By varying the HA:TCP ratio, it was possible to modulate the substitution rate and bioactivity of these biomaterials. 119 , 120 BCPs are a valuable alternative for clinicians and patients who are not comfortable with implantation of material of human or animal origin. Future perspectives may involve the development of a selection of two to three BCPs to fit individual clinical indications. A very interesting and promising research field is the development of biomaterials, particularly BCPs, that are osteoinductive. This biomaterial-induced or intrinsic osteoinduction should not be confused with the biomaterial-free induction of undifferentiated inducible osteoprogenitor cells. 121 Thus far, this intrinsic, biomaterial-dependent osteoinduction is considered unpredictable in various animal models and in humans. A mechanism for biomaterial-induced heterotopic ossification has been proposed, for example by Bohner and Miron. 121
Bioglasses are silica-based materials that were first introduced in the early 1970s. These glasses exhibit bone bonding as a result of the surface reactive silica, calcium, and phosphate groups that are characteristic of these materials. Silica is believed to play a critical role in bioactivity. Bioactive glasses are very biocompatible materials. Some experimental data support their use in GBR procedures such as ridge preservation and sinus augmentation. However, there are inherent limitations on the currently available bioglass products. Because of their granular and nonporous nature, they cannot reliably serve as space-maintaining devices, although macroporous glass ceramics are now also available. 122
Bone healing in membrane-protected defects without addition of a bone filler
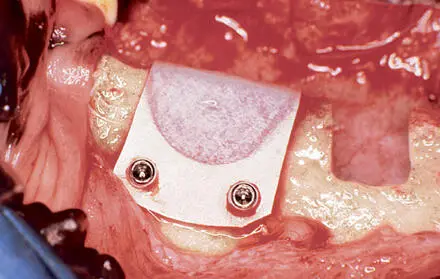
The histologic healing pattern of bone regeneration under a barrier membrane without addition of a bone filler was demonstrated by Schenk et al in a landmark experimental study. 123 Saddle-type defects were created in the mandibles of dogs two months after tooth extractions. The defects were covered with (test) or without (control) a barrier membrane (Fig 2-25). A standard ePTFE membrane and two different prototype ePTFE membranes reinforced with polypropylene mesh were used. The position of the membranes was secured by two miniscrews. No bone filler was used. However, intravenously aspirated blood was injected under each membrane. Histologic analysis was performed after healing periods of 2 and 4 months.
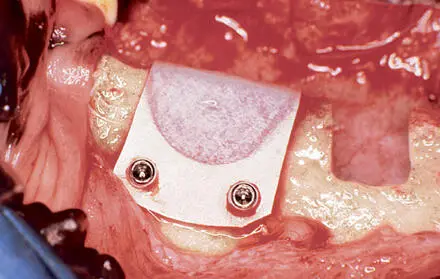
Fig 2-25Surgical procedure of GBR. Two defects were created in the exposed mandible of a dog 2 months after tooth extractions. The right defect is open, but the left one is covered with a nonresorbable ePTFE membrane. Miniscrews fix the membrane and mark the corners of the defect for radiography.
Healing without a barrier membrane
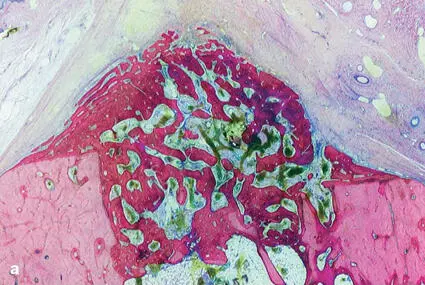
The control defects showed a consistent repair pattern in which bone formation was restricted to the defect margins, ie, mesial and distal walls of the defect and at the bottom of the defect (Fig 2-26a). Closure of the marrow space was completed after 2 months, but bone formation made no further progress. At 4 months, bone had slightly increased in density.
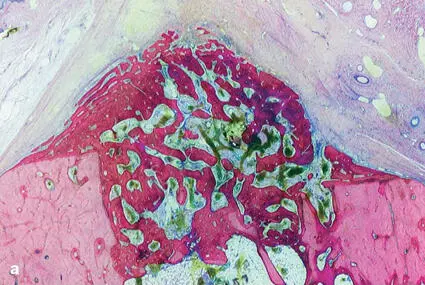
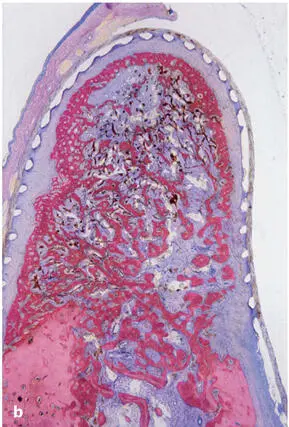
Fig 2-26Buccolingual ground sections through the central portion of (a) a control site (without membrane) and (b) a test site (with a nonresorbable ePTFE membrane) after 2 months. While a low bony cover seals off the marrow space at the bottom of the control defect, the regenerated bone completely fills the secluded space beneath the barrier membrane at the test site (undecalcified ground section; toluidine blue and basic fuchsin stain).
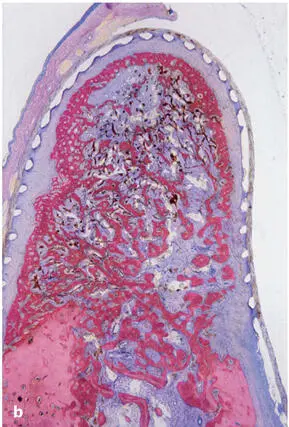
Healing under a barrier membrane
Membrane protection resulted in a dramatic change in bone regeneration. The membrane maintained the space created during surgery and clearly separated the outer compartment, constituting the oral mucosa, from the inner space, which was mainly accessible from the marrow cavity (Fig 2-26b). This inner compartment was initially filled with a blood clot, and at 2 months, remnants of the coagulum could still be recognized in the middle portion of the defect (Figs 2-27 and 2-28). 123 However, the hematoma was completely penetrated by granulation tissue and blood vessels. The majority of the secluded volume now consisted of a spongeous bony regenerate that enclosed, between its trabeculae, a labyrinth of tiny, interdigitating marrow spaces filled with hypervascularized, loose, soft connective tissue. Both the vessels and the fibrous tissue were in continuity with the original bone marrow at the bottom of the defect. Bone formation started, as in the controls, from the margins of the defects, where it spread over the openings of the marrow cavity (see Fig 2-28).
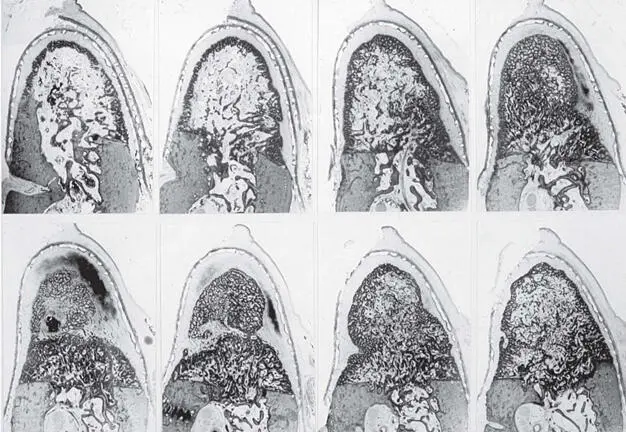
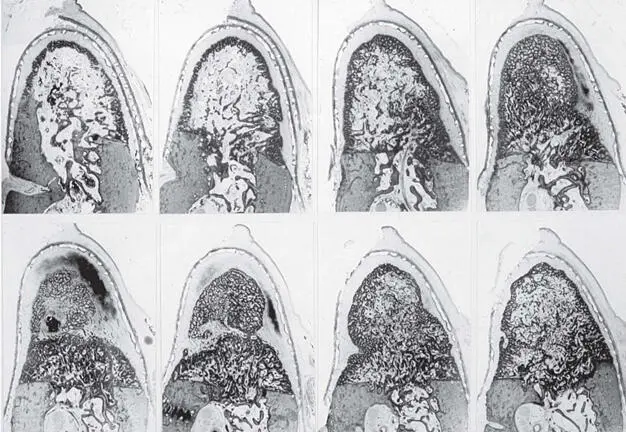
Fig 2-27Selected serial buccolingual sections, arranged in a mesiodistal sequence, of a membrane-covered defect after 2 months. (Reprinted with permission from Schenk et al. 123 )
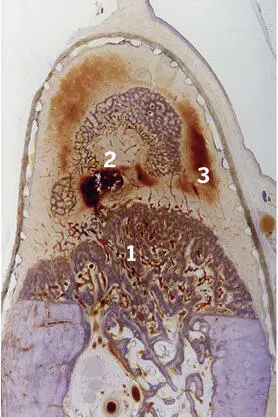
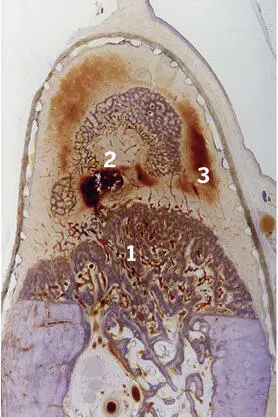
Fig 2-28The fifth section from Fig 2-27 to show (1) the bony cover of the bottom marrow space and (2) a tangential section through the top of the bony hill originating from the mesial wall of the defect, as well as (3) the associated hematoma.
Thus, there were basically three centers of bone formation, and these formed a dome-shaped seal over the openings of the marrow cavity. From these bony covers, bone further expanded into the center of the membrane-bound space. Both radiographs (Fig 2-29) and serial ground sections (see Fig 2-27) demonstrated this characteristic pattern of bone healing. 123 See Fig 2-28 for an illustration of the third center of bone formation at the bottom of the defect.
Читать дальше