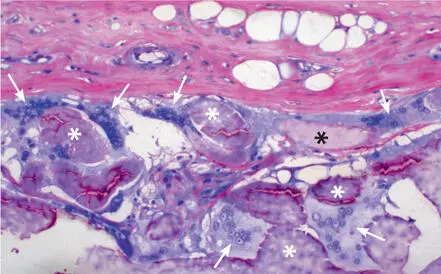
Synthetic polyesters used as barrier membrane biomaterials are polyglycolides (PGAs), polylactides (PLAs), or copolymers thereof. Other aliphatic polyesters used are polydioxanones 62 and trimethylene carbonates. 63 These synthetic biomaterials have both advantages and disadvantages. They can be made available in almost unlimited quantities. Another advantage is the ability of PGA, PLA, and their copolymers to completely biodegrade to carbon dioxide and water via the Krebs cycle. 64 Numerous factors are known to affect the degradation of bioresorbable polymers, such as their structure and chemical composition, molecular weight, shape, processing conditions, sterilizing processes, physicochemical factors, and mechanism of hydrolysis. 65 , 66 The use of these polymers as bone plates, screws, and delivery vehicles for drugs and growth factors has been associated with inflammatory and foreign-body reactions in orthopedic and maxillofacial surgery and implant dentistry (Fig 2-19). In certain cases, even surgical debridement and removal of the biomaterial may be required. 67 – 71
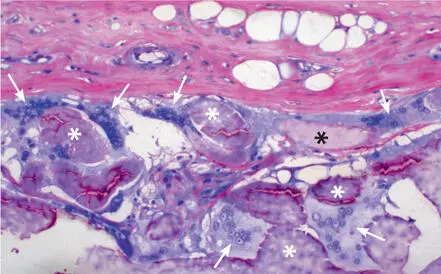
Fig 2-19GLTC membrane at 12 weeks. Numerous large multinucleated giant cells (arrows) are interposed between an amorphous matrix (asterisks) that partly replaces the membrane material (undecalcified ground section, toluidine blue and basic fuchsin surface stain).
Collagen membranes
Most natural resorbable membranes are made of collagen from animal tissues, although human sources exist as well. The collagen membranes have different tissue sources, including bovine tendon, bovine dermis, calf skin, porcine dermis, and human skin from cadavers. 72 Collagen is the most abundant extracellular matrix protein in the body. Collagen has important structural functions, and it also supports cell attachment, cell differentiation, tissue repair, and tissue regeneration. 73 , 74 Collagen-based biomaterials are widely used in biomedical applications since they closely mimic the extracellular environment. Furthermore, collagen has low immunogenicity and is hemostatic. 75
On the other hand, collagen membranes have unfavorable mechanical properties 76 and may provide an inadequate barrier function because they biodegrade too quickly through enzymatic activities of macrophages and polymorphonuclear neutrophils. 77 – 79 Biodegradation of collagen membranes into carbon dioxide and water is caused by endogenous collagenases. 75 To prolong the barrier function, a number of cross-linking technologies, such as ultraviolet light, formaldehyde, glutaraldehyde, diphenylphosphoryl azide, and hexamethylene diisocyanate, have been used. 80 , 81 The glutaraldehyde technique was reported to leave cytotoxic residues. 82 The degree of collagen cross-linking inversely affects the degradation rate. 83 Membrane ossification is a phenomenon observed in certain cross-linked collagen membranes. The modified collagen seems to trigger membrane ossification. 84 , 85
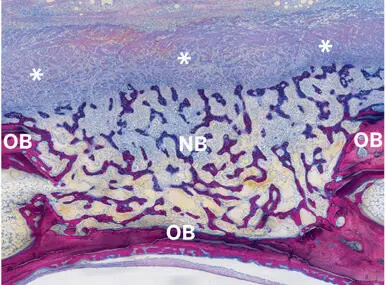
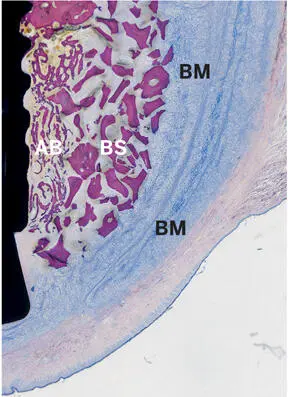
Non-cross-linked collagen membranes are currently the membrane of choice for most GBR procedures, whereas nonresorbable membranes made of dPTFE may be recommended for selected vertical augmentation procedures only. Figures 2-20 and 2-21 show two excellent regenerative outcomes when a non-cross-linked collagen membrane was used to cover a bone defect either created in the rabbit calvaria or lateral to a dental implant, respectively.
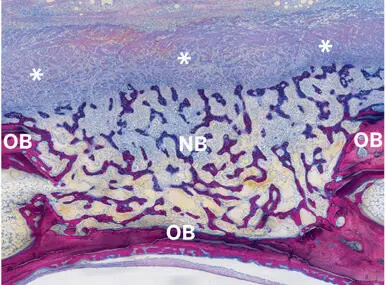
Fig 2-20Light micrograph illustrating a non-cross-linked collagen membrane (Bio-Gide, Geistlich) (asterisks) over a bone defect 2 weeks after its creation in the rabbit calvaria. New bone (NB) has loosely filled the defect space and has even surpassed the height of the pristine old bone (OB) (undecalcified ground section; toluidine blue and basic fuchsin stain).
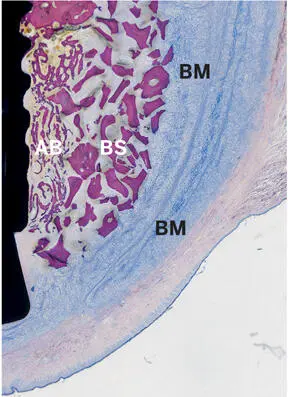
Fig 2-21Light micrograph illustrating a buccal peri-implant bone defect 3 weeks after augmentation with autogenous bone chips (AB), a bone substitute (BS) (Bio-Oss, Geistlich), and a non-cross-linked barrier membrane (BM) (Bio-Gide). The double-layered barrier membrane perfectly covers the augmented region and blocks off from the oral mucosa (undecalcified ground section; toluidine blue and basic fuchsin stain).
Bone grafts and bone substitute materials
Since most bioresorbable membranes, and to a lesser degree ePTFE membranes, are largely incapable of maintaining defect space due to lack of sufficient rigidity, these membranes are often used in combination with autogenous bone grafts, bone substitute materials, or composite grafts. Bone fillers, however, serve many more purposes, including the following:
Provide mechanical support to prevent membrane collapse
Stabilize the blood clot
Allow ingrowth of blood vessels
Act as an osteoconductive scaffold for bone ingrowth
May be osteoinductive
May contain bone cells
Become integrated in or replaced by bone
Protect the augmented volume from resorption
The clinical indications for using bone filler materials range from grafting minor peri-implant bone defects to the regeneration of large continuity defects. Considering this wide range of purposes, it is to be expected that one single material cannot fulfill all requirements. Therefore, it will often be necessary to combine two or more materials to obtain a successful and predictable treatment outcome.
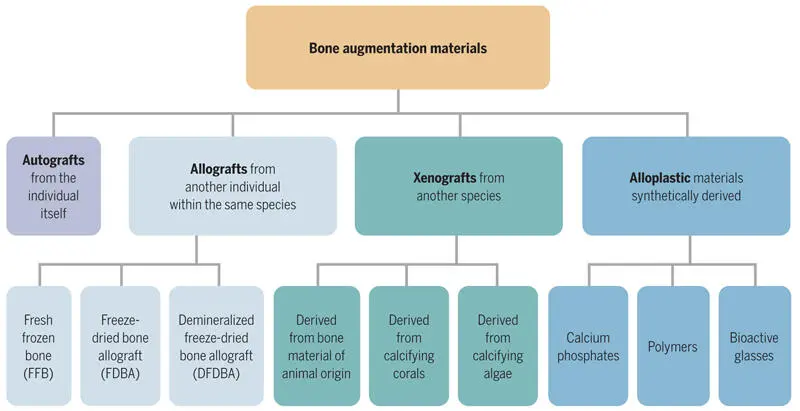
Bone filler materials can either be derived from the person being treated (autogenous bone grafts or autografts) or from an external source (bone substitute materials). The bone substitute materials are subdivided into allogeneic bone, xenogeneic bone, and alloplastic (synthetic) bone graft substitutes. Figure 2-22 shows a common classification of bone grafting materials. These materials possess different physical, chemical, and biologic characteristics. The biologic properties are commonly described as:
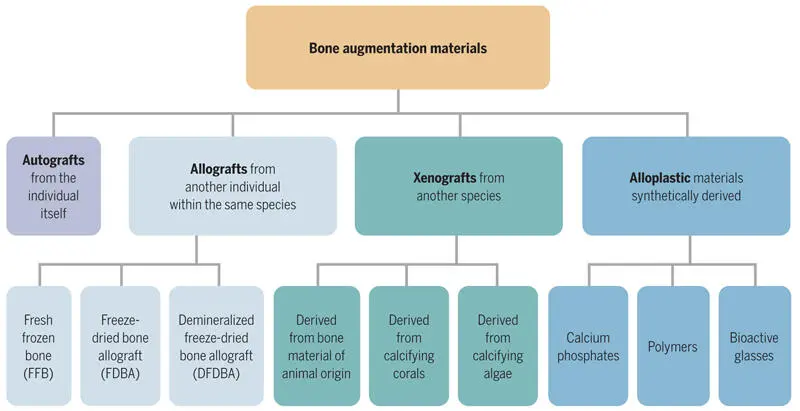
Fig 2-22Classification of bone augmentation materials.
Osteoconductive
Osteoinductive
Osteogenic
Osteoconductive materials possess a matrix that serves as a scaffold or framework. This matrix is used as a template and an enlarged solid base for bone deposition. Materials with osteoinductive properties contain proteins (BMPs) that stimulate and support proliferation and differentiation of uncommitted stem cells to become osteoblasts. Osteogenic means that the autogenous bone contains bone cells (bone-lining cells, osteoblasts, osteoblast uncommitted stem cells, and/or osteocytes) that are capable of directly or indirectly supporting bone formation at the transplantation site.
Autogenous bone grafts
Autogenous bone is a preferred bone graft material because it possesses osteoinductive, osteogenic, and osteoconductive properties. However, the harvesting of autogenous bone may require an additional surgical intervention, which increases the operative time, costs, intraoperative blood loss, pain, and recovery time. Moreover, it is associated with an increased risk of donor site morbidity (eg, increased postoperative pain, nerve injury, blood vessel injury, hematoma, infection, hernia formation, and cosmetic disadvantages). Finally, the supply of autogenous bone for grafting may be limited.
Читать дальше