Several etiological factors have been implicated for the lack of osseointegration, including implant surface contamination during placement, overheating of bone, insufficient bone quantity, poor bone quality, lack of primary stability, and improper immediate occlusal loading scheme [43]. This complication can be prevented by ensuring anchorage of the zygomatic implant is obtained in more portions of the cortical bone, sufficient irrigation is performed during its placement, and immediate loading is accomplished only if primary stability is achieved [45]. In fact, recent evidence shows that the use of an immediate load protocol (ILP) with zygomatic implants can contribute to immediate zygomatic implant stability by utilizing the stability of the other implants placed simultaneously (either standard anterior maxillary implants or the use of four zygomatic implants [quad‐zygoma option]). It has been suggested that if a total of 120 NCm 2torque is present from all implants within the arch, an ILP can be used successfully. Also, when using zygomatic implants, it is important to investigate the presence of an oroantral fistula in cases of loss of implant osseointegration [47]. If the implant is not osseointegrated and there is a presence of oroantral communication, the implant should be removed and the oroantral communication should be closed with a buccal fat pad procedure. Once healed, the zygomatic implant can be replaced in three to four months [47].
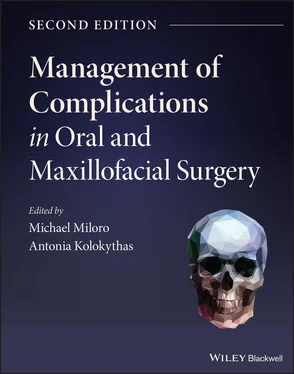
Mucositis and peri‐implantitis have also been associated with zygomatic implants. The extrasinus technique has reduced the incidence of maxillary sinusitis while allowing more buccofacial (as opposed to palatal) placement of the zygomatic implants, but has shown to cause other adverse outcomes such as mucositis and peri‐implantitis, since a significant portion of the implant is located under the mucosa outside of the bony housing [48]. To mitigate this issue, surgeons [48] have utilized the buccal fat pad to cover the facial surface of the zygomatic implants, which not only provides thickness to the gingiva on the buccal implant surface, but also prevents gingival recession ( Figure 3.23). As with other implant treatment plans, zygomatic implants should follow a restoratively driven plan for the location of the zygomatic implants, and a more buccal positioning of the implant allows improved prosthetic reconstruction, and avoids impingement of the prosthesis on the tongue space and speech interferences when the implants are placed in a more palatal position [49].
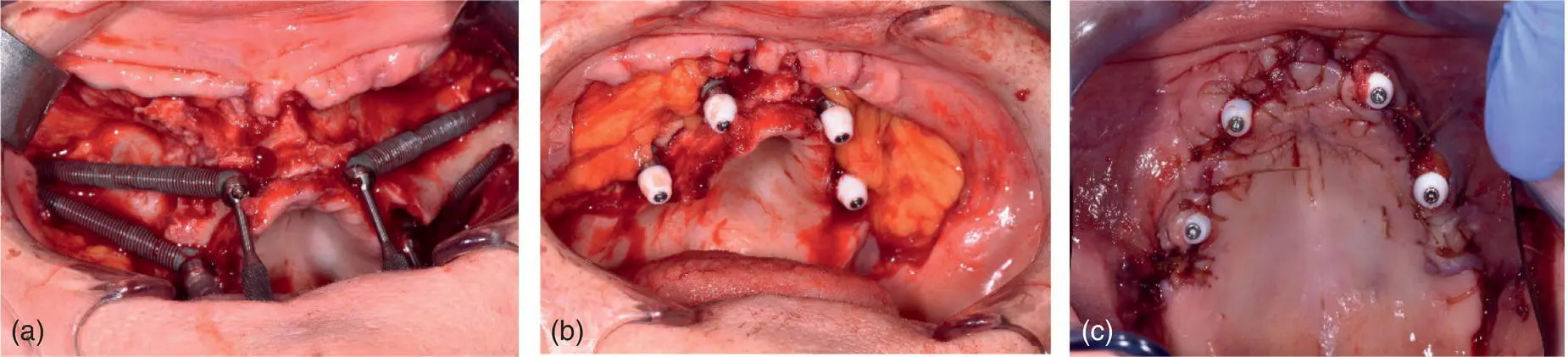
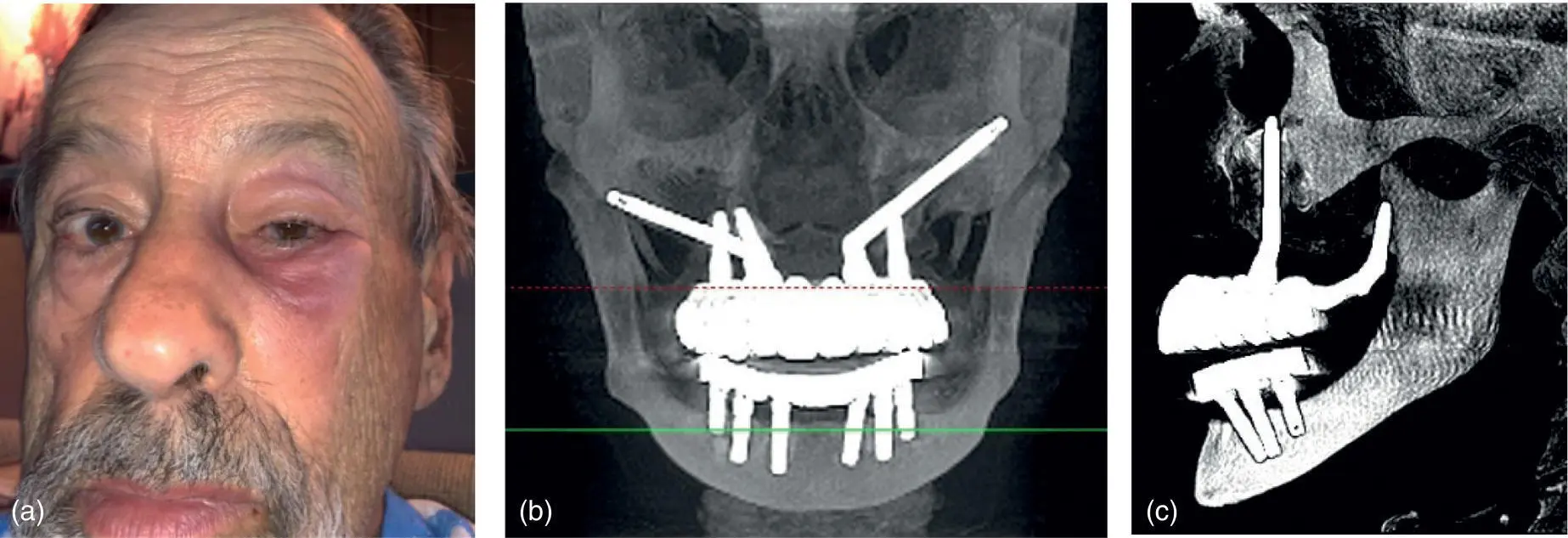
In rare instances, aseptic necrosis of the zygoma bone in the region of the apical portion of the zygomatic implant can result in a cutaneous fistula. If only a small area of the implant is involved, this complication can be managed with an excision of the fistula and resection of the protruding apical portion, without sacrificing the implant and prosthetic restoration. Other unusual complications of zygomatic implants include penetration of the implant in the orbital and intracerebral cavities, and fungal infection of the maxillary sinus leading to aspergillosis [4550–52] ( Figure 3.24). One case report [53] has documented a 61‐year‐old women who suffered an accidental penetration of the right lateral orbital wall with a zygomatic implant that led to a sudden intraoperative hemorrhage from the lateral canthus of the right eye. After surgery, she had limitation in the movement of the right eye and binocular horizontal diplopia, and she required an emergent hospital admission, ophthalmology consultation, and removal of the zygomatic implant [54]. The ideal way to handle this complication is with prevention, meticulous planning, and a strict adherence to proper surgical protocol. It has been suggested [55] to use the infraorbital nerve as a reference point in maintaining the oblique direction of the drill while making the osteotomies in the superior aspect of the zygomatic bone. If this path drifts posteriorly into the infratemporal fossa, brisk bleeding may be encountered ( Figure 3.25). If the direction is straighter and anterior, the implant may enter the orbit [56]. To prevent inadvertent entry into the orbital and intracranial cavities, a clear view of the path of the drills and implant is essential while performing this procedure. The zygomatic implant drill tip should be visualized when it exits the zygomatic bone or zygomaticomaxillary buttress to ensure that it has not entered the orbit, cranium, or pterygomaxillary or infratemporal fossae ( Figure 3.26). Of course, zygomatic implant placement is a technically challenging procedure and should be performed only by surgeons with the proper training. As with the prevention and treatment of all dental implant complications, surgical experience is paramount in minimizing morbidity and achieving a successful overall treatment outcome.
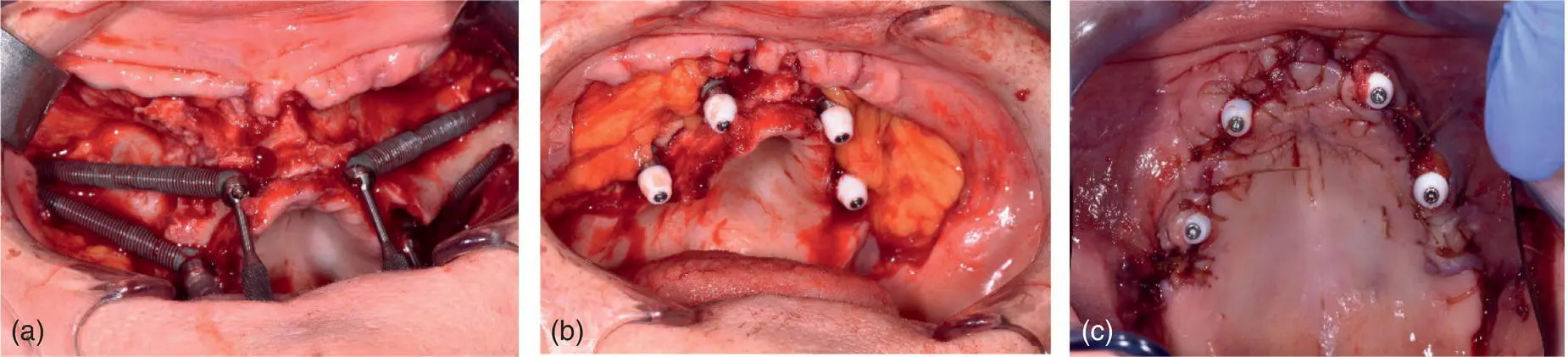
Fig. 3.23. (a–c) Quad‐zygoma implants with buccal fat pad coverage.
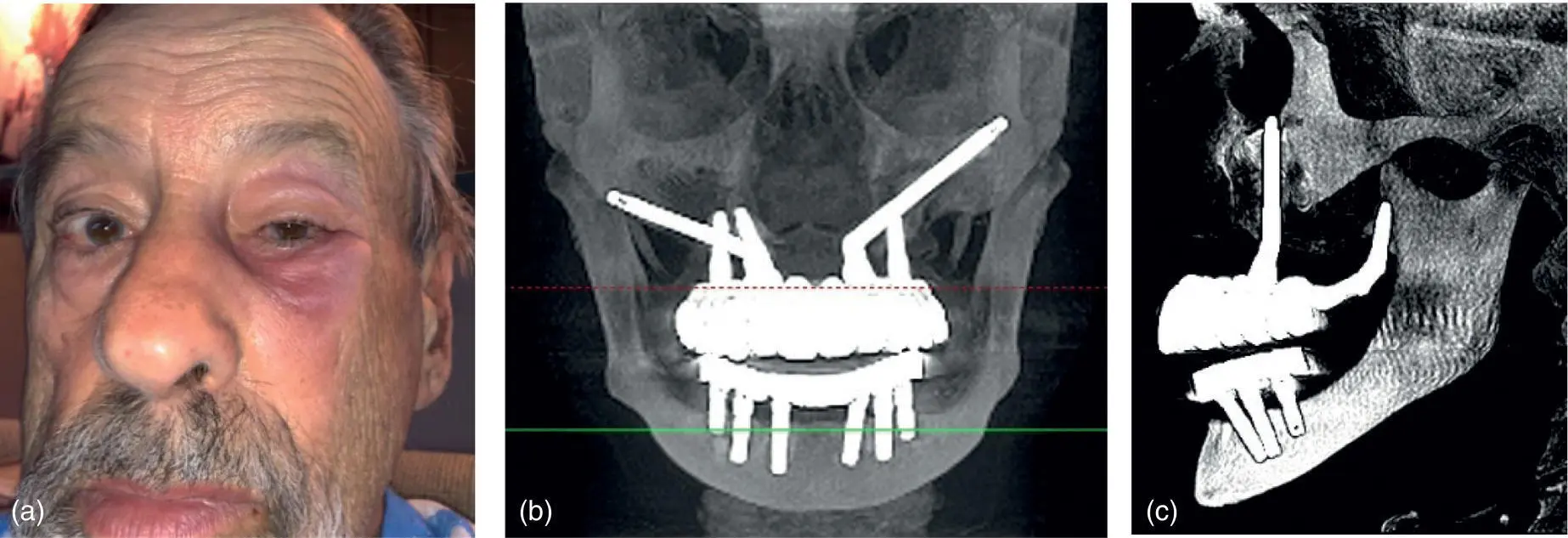
Fig. 3.24. (a–c) Zygomatic implant placed into left orbital cavity causing periorbital cellulitis.
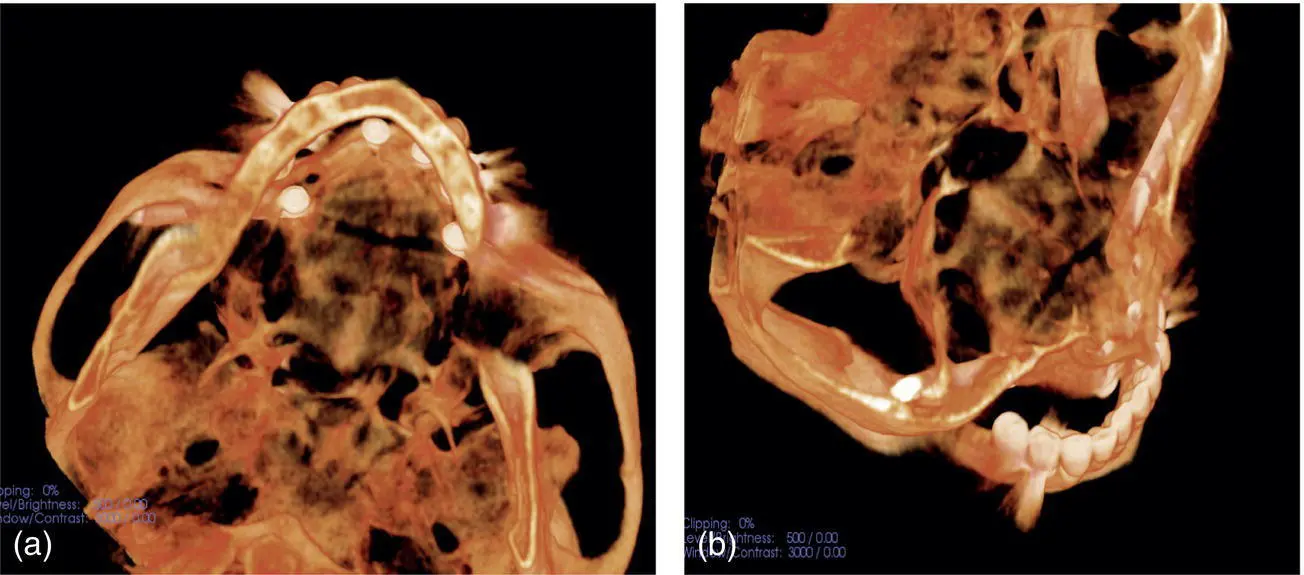
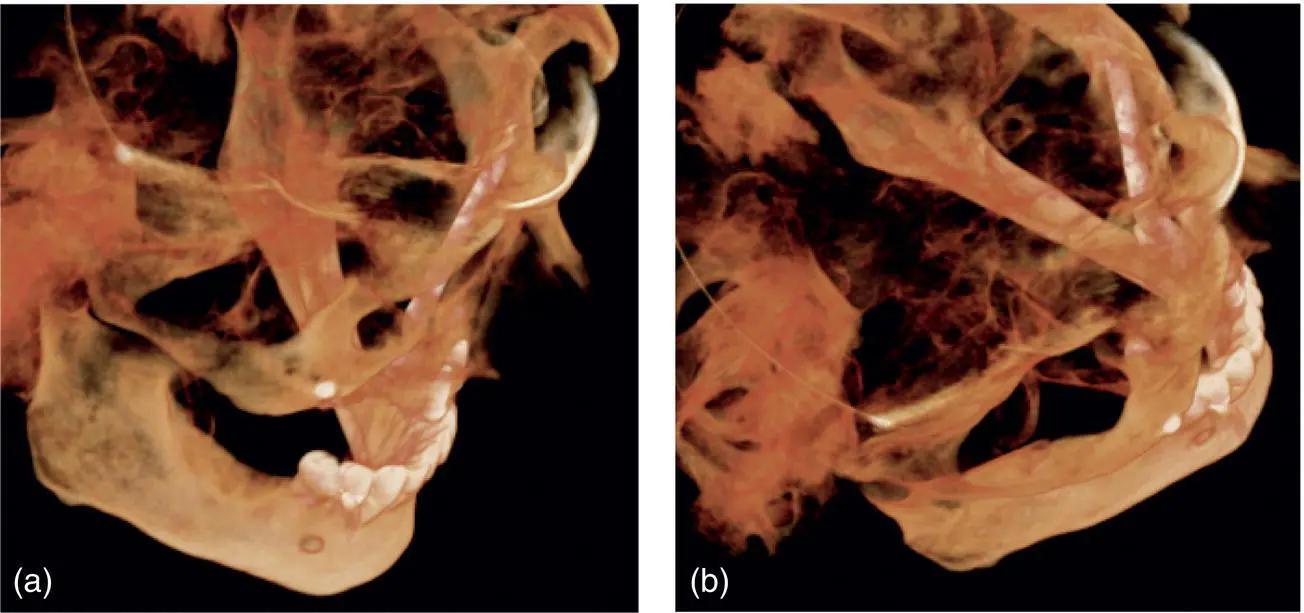
Fig. 3.25. (a, b) Zygomatic implant placed into right infratemporal fossa.
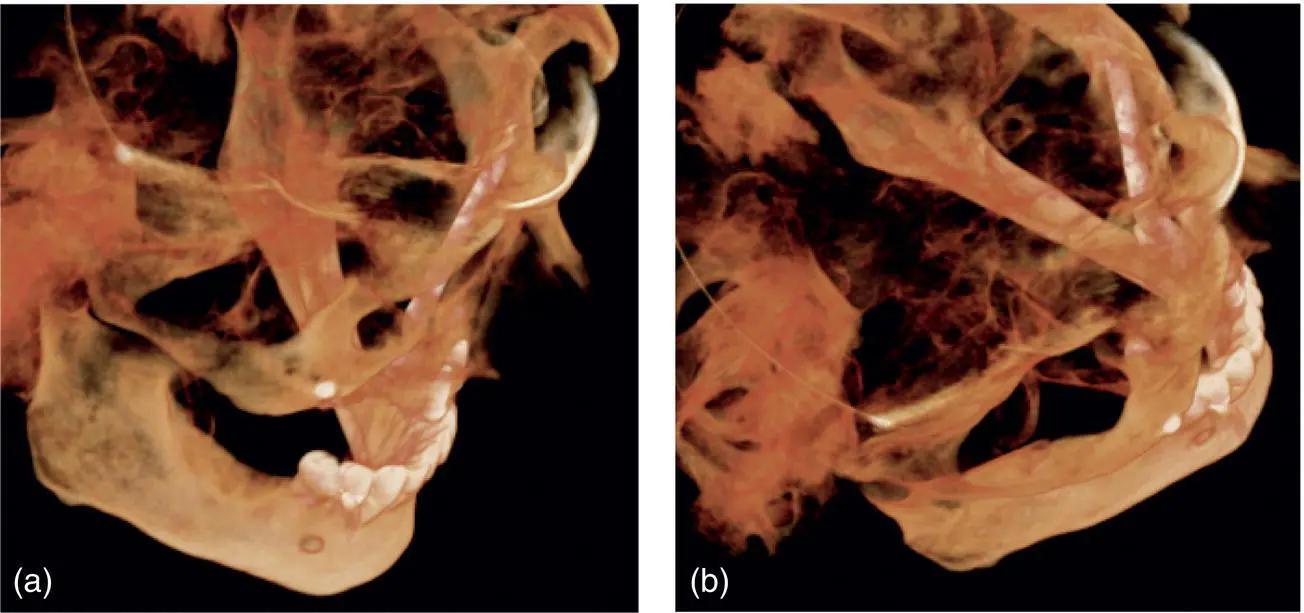
Fig. 3.26. (a, b) Following implant removal and replacement to engage the zygomatic bone.
Although a variety of minor and major complications may occur during the course of dental implant placement, with adequate planning and attention to detail during the implant surgery the majority of complications can be minimized. In addition, the prudent use of technological advancements in diagnostic imaging and 3D planning, as well as the use of computer‐generated guides and, on occasion, navigational assistance during the surgical execution, can also reduce the incidence of adverse events and ensure successful short‐ and long‐term outcomes from dental implant therapy and prosthetic reconstruction.
1 1. Klokkevold, P. and Han, T. (2007). How do smoking, diabetes, and periodontitis affect outcomes of implant treatment? Int. J. Oral Maxillofac. Implants 22: 173–206.
2 2. Moy, P., Medina, D., Shetty, V., and Aghaloo, T. (2005). Dental implant failure rates and associated risk factors. J. Oral Maxillofac. Implants 20: 569–577.
3 3. Martin R, Carter J, Barber HD. Fonseca R, Powers M, Barber HD Surgical Implant Failures. Chapter in Oral and maxillofacial surgery. WB Sauders Company Philadelphia. 2000; 1st ed. Vol 7.
4 4. Cochrane, D.L., Schou, S., Heitz‐Mayfield, L.J.A. et al. (2009). Consensus statements and recommended clinical procedures regarding risk factors in implant therapy. Int. J. Oral Maxillofac. Implants 24: 86–89.
5 5. Balshi, T. (1997). An analysis and management of fractured implants: a clinical report. J. Oral Maxillofac. Implants 11: 660–666.
6 6. Kim, B.S., Kim, Y.K., Yun, P.Y. et al. (2009). Evaluation of peri‐implant tissue response according to the presence of keratinized mucosa. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 107 (3): e24–e28.
7 7. Schrott, A.R., Jimenez, M., Hwang, J.W. et al. (2009). Five‐year evaluation of the influence of keratinized mucosa on peri‐implant soft‐tissue health and stability around implants supporting full‐arch mandibular fixed prostheses. Clin. Oral Implants Res. 20 (10): 1170–1177.
Читать дальше