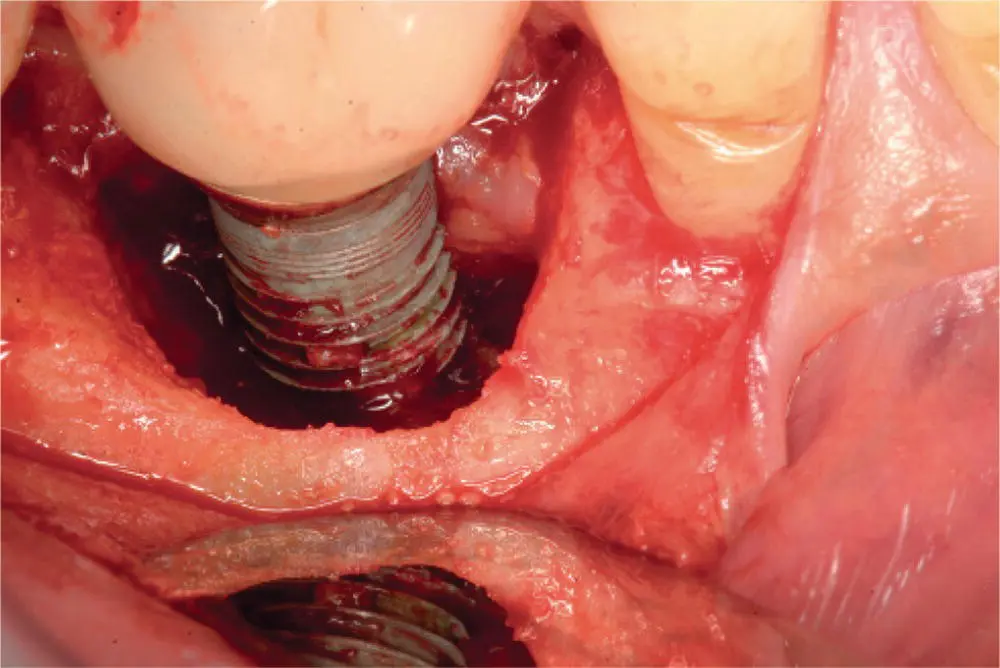
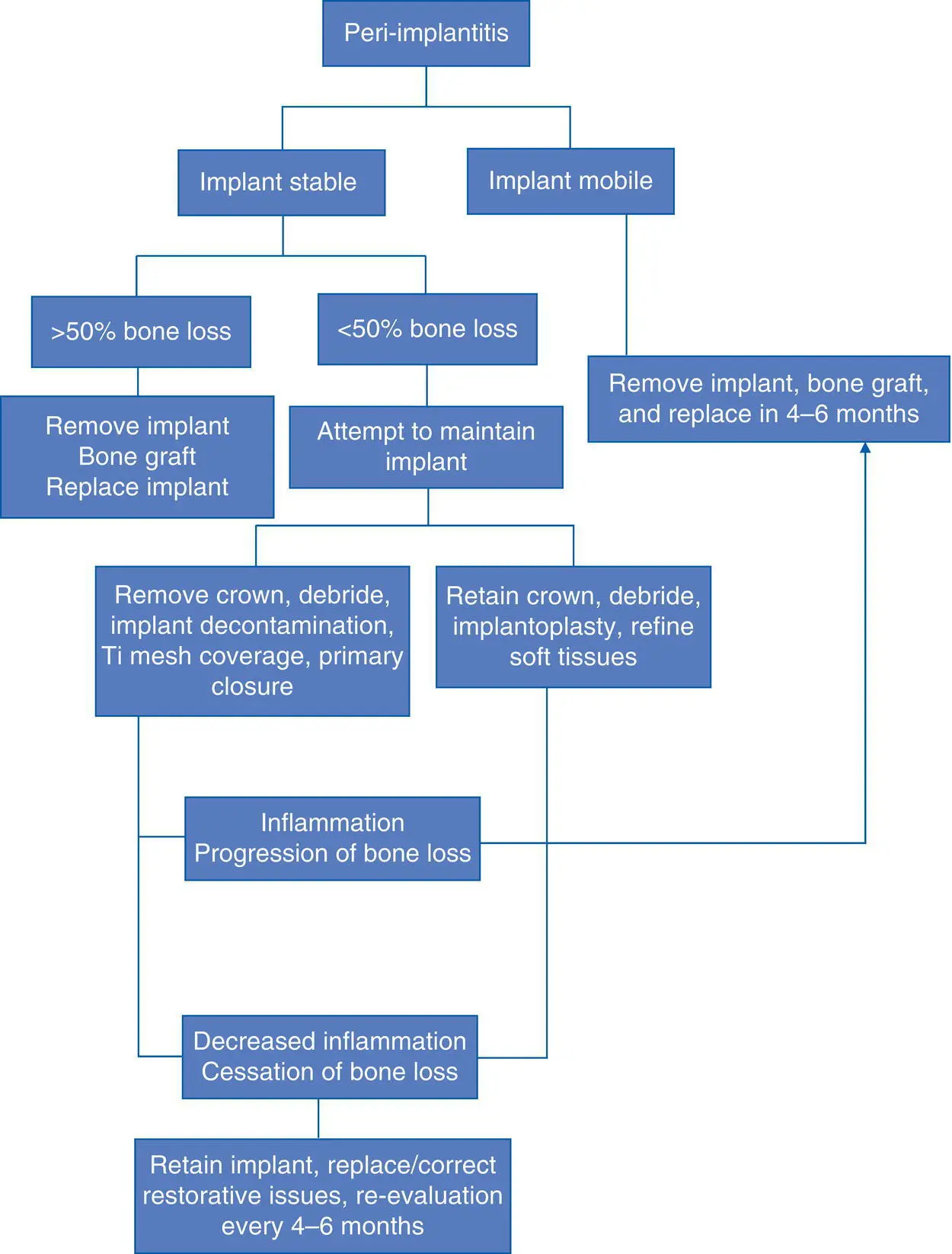
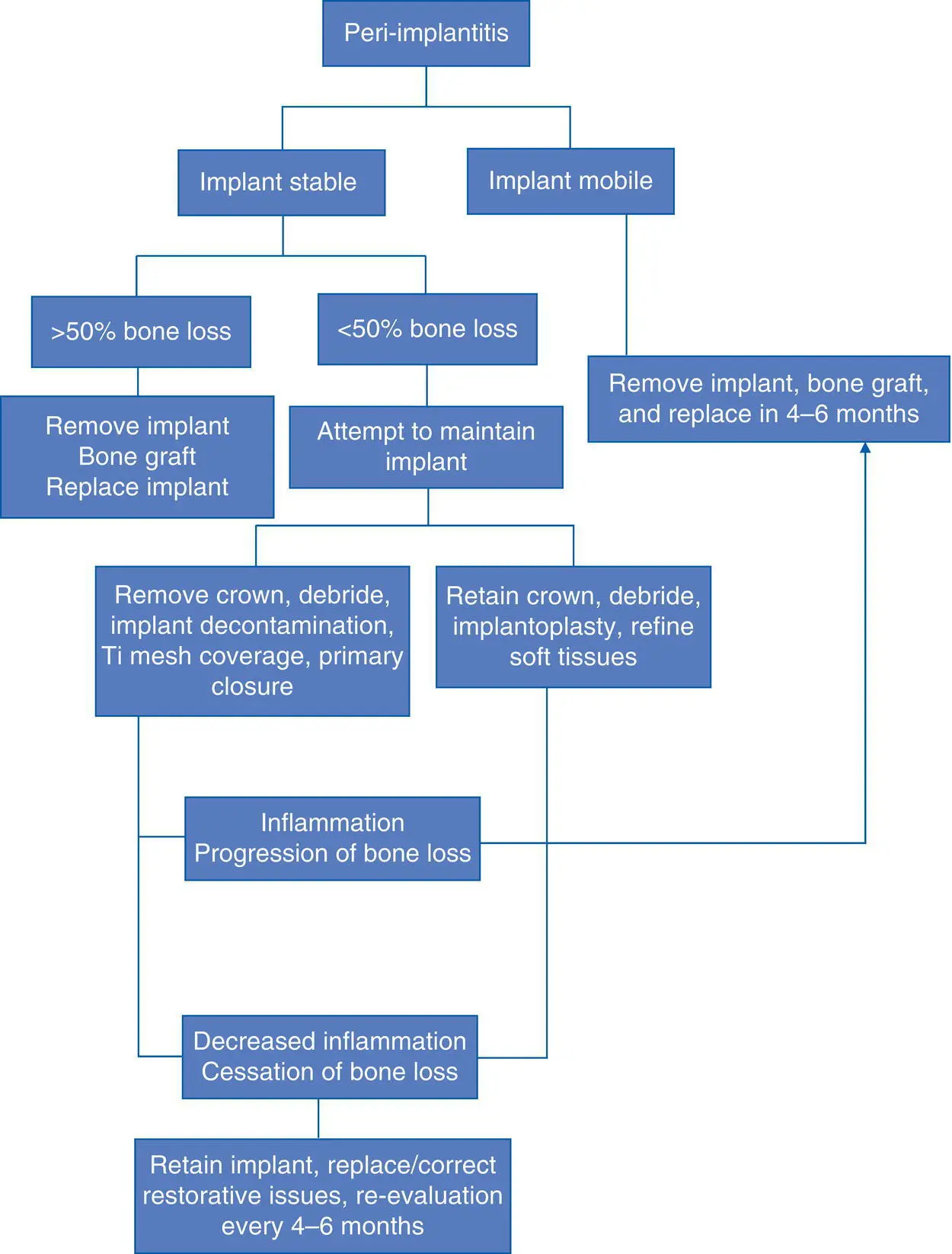
The phenomenon of peri‐implantitis is a well‐recognized and frustrating clinical problem for dental implant surgeons and patients. Part of this frustration lies in the fact that unlike periodontal disease, which is well defined and organized into categories, peri‐implantitis remains a rather ambiguous and debated term with variable clinical presentation. Some surgeons prefer the term “peri‐implantosis” since there are instances where there is bone loss surrounding an implant, but an absence of inflammation, so the term “peri‐implantitis” would not technically apply [35]. Most surgeons agree that for a diagnosis of peri‐implantitis to exist the presence of gingival recession and implant exposure and bone loss should be present. The distinguishing factor between peri‐implantitis and peri‐implant mucositis is that peri‐implantitis has bone loss around the implant ( Figure 3.16), while peri‐implant mucositis does not exhibit bone loss since the inflammation is confined to the mucosa ( Table 3.5). The bone loss in peri‐implantitis has been referred to as a “saucer‐shaped” bone defect around the implant on clinical examination and a peri‐implant radiolucency on radiographic imaging ( Figure 3.17). Peri‐implantitis often presents itself years after initial dental implant placement, and for this reason is included in the late‐stage infection category. Often, the peri‐implant bone loss is discovered incidentally on routine dental radiographs, and in the posterior region of the jaws, the presence of gingival inflammation, pain, BOP, purulence, and recession may go unrecognized by the patient for some time. Peri‐implantitis is believed to be due to biofilm formation on the implant surface with colonization by Staphylococcus aureus , which is an organism not typically seen with periodontitis. Risk factors include a history of periodontitis, smoking, poor oral hygiene, exposed implant threads, exposed surface coatings, and deep pocket depths. Treatment includes mechanical debridement with ultrasonic scalers or a titanium wire brush or the use of an erbium–YAG laser, implant surface decontamination with citric acid solution (5%), chlorhexidine irrigation, local antibiotics (25% tetracycline gel or fibers), systemic antibiotics (ornidazole or metronidazole), and improved oral hygiene that may be improved with an alteration in the prosthetic design (e.g., ridge‐lap prosthesis, or splinted prosthesis). Also, surgical reconstruction may include regenerative surgery with bone grafting, GBR, or connective tissue grafting, or resective surgery with osteoplasty and apically repositioned flaps. If there is retained cement in the area, it should be debrided. Of the options of debridement, resection, grafting, and GBR, bone grafting and GBR may have improved bone fill and pocket depth reduction in cases of peri‐implantitis.
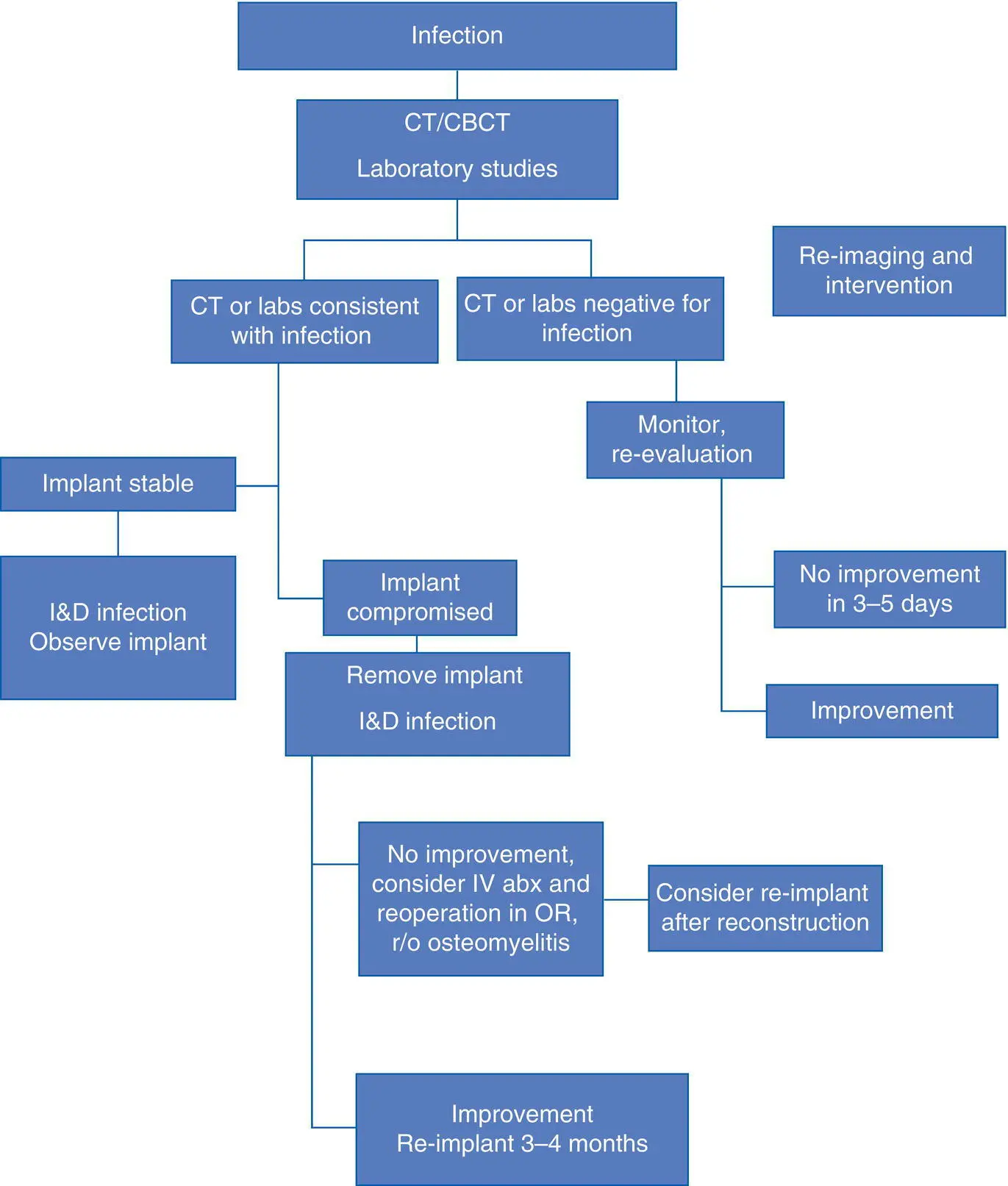
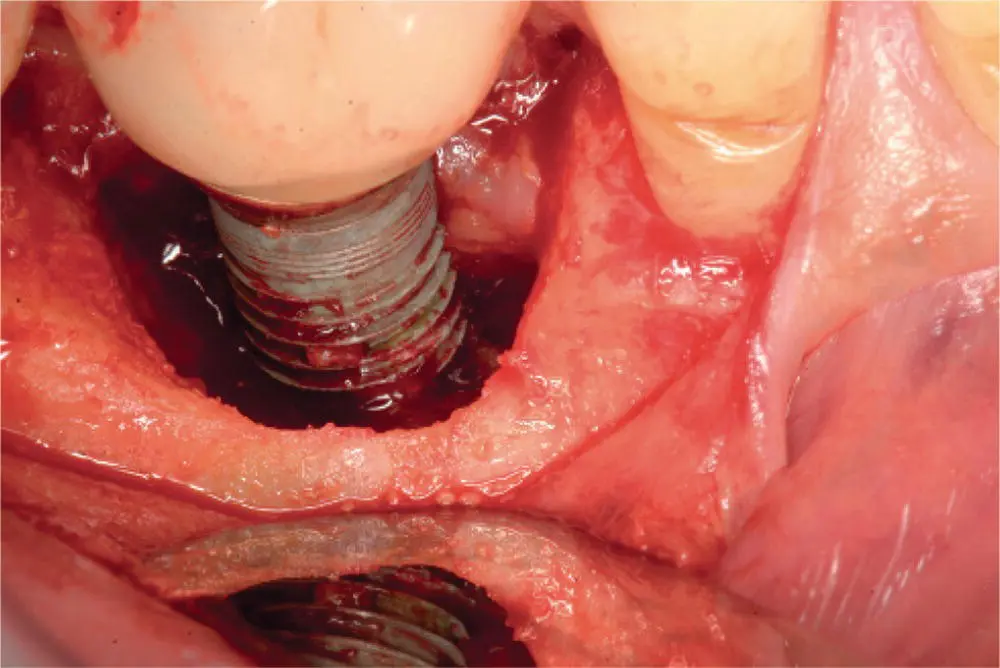
Fig. 3.16. Peri‐implantitis leading to bone loss (crater‐like defect).
Table 3.5. Peri‐implant mucositis versus peri‐implantitis
| Clinical parameter |
Peri‐implant mucositis |
Peri‐implantitis |
| Increased probing depth |
+/− |
+ |
| BOP |
+ |
+ |
| Suppuration |
+/− |
+ |
| Implant mobility |
− |
+/− |
| Radiographic bone loss |
− |
+ |

Fig. 3.17. Periapical radiograph showing bone loss due to peri‐implantitis.
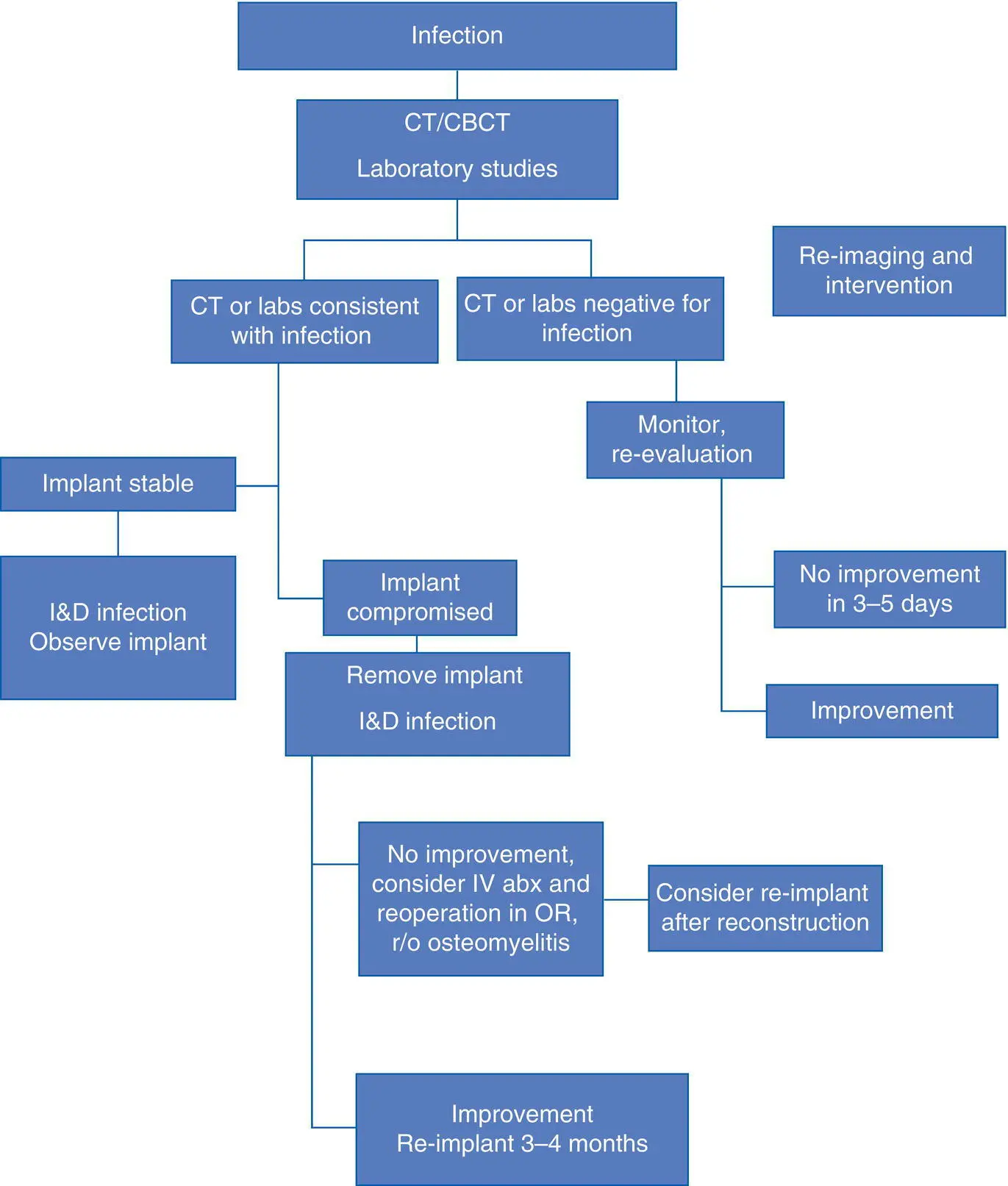
A clear distinction needs to be made between increased probing depths around a dental implant and an established diagnosis of peri‐implantitis. Often bone levels around the implant may be ideal; however, a soft tissue pannus formation, in the form of a gingival pseudo‐pocket, may lead inexperienced clinicians to diagnosis a case of peri‐implantitis [36]. Although this excessive pseudo‐pocket is not ideal and can lead to oral hygiene issues with eventual bone loss, this is not an inevitable consequence. With meticulous oral hygiene maintenance and close follow‐up, this region can often be maintained without any untoward effects. In certain circumstances, gingivectomy may be required for excessive soft tissue, but careful attention must be paid to not affect the esthetic outcomes of the soft tissues, especially in the anterior esthetic zone. Once a diagnosis of peri‐implantitis has been established, the clinician must control the contributing factors, assess the presence of keratinized tissue, and evaluate the implant surface, implant location, restorative issues, and the presence of parafunctional habits [37]. Since these factors have been discussed previously, the discussion will focus on the surgical management of the implant with localized bone loss and inflammation with the understanding that other contributing factors have been addressed in order to optimize the outcome. Many of the initial stages of peri‐implantitis can be managed similar to periodontal disease. Nonsurgical peri‐implant debridement includes chemical and mechanical debridement. Chemical debridement with various topical agents such as chlorhexidine, citric acid, hydrogen peroxide, and tetracycline can be used. Mechanical debridement with implant scalers, titanium brushes, and lasers can be used. These techniques should be combined with patient education on the use of meticulous oral hygiene to help decrease peri‐implant soft tissue inflammation allowing for increased tissue adherence (soft tissue seal) around the implant fixture [38]. This increased tissue tone decreases bacterial migration along the implant surface and can prevent further infection and bone loss. More advanced cases of peri‐implantitis, with up to 50% bone loss, must be assessed regarding a guarded long‐term implant prognosis. If the implant is deemed salvageable, this will require open surgical debridement, bone grafting with guided tissue membrane regeneration, and temporary removal of the existing restoration [39]. Once appropriate bone and soft tissue healing has occurred, with evidence of adequate osseous regeneration around the implant, the implant may be uncovered and prosthetically restored. Peri‐implantitis that has progressed to greater than 50% bone loss, implant mobility, and recurring infections often necessitate implant removal and bone grafting with delayed implant replacement and restoration ( Algorithm 3.7).
Algorithm 3.7: Peri‐implantitis
There are a variety of biomechanical and prosthetic complications of implant dentistry ( Table 3.6), and fracture of dental implants and fractured implant components are other complications that have become more common with the increased number of implants being placed by dentists and specialists. From a prosthodontic standpoint, porcelain fractures from an implant crown are managed the same as porcelain fractures from a crown on a natural tooth ( Figure 3.18). If the crown is screw‐retained, it is removed easily, and repaired or replaced. With regard to fractured components within the body of the dental implant (e.g., abutment screws, cover screws, healing abutments), the process is more complex, since if the fractured components cannot be retrieved the implant will require removal and replacement [40]. Once identified, the loose portions of the fractured implant or components should be removed in order to avoid aspiration or ingestion ( Figure 3.19). Ideally, blind attempts at retrieval should be avoided since this may lead to the fractured foreign body becoming permanently lodged in the implant necessitating implant removal, even with integrated implants, since they will not be able to be restored properly. Visualization of the internal channel of the implant can be extremely difficult, especially in the posterior maxilla and mandible, and for this reason magnification is required when attempting to retrieve a broken screw or other part within an implant body. There are several commercially available screw retrieval kits on the market that can assist in removal of fractured implant components. These must be used with caution since they often involve the use of rotary instrumentation within the delicate inner channel of the implant and iatrogenic damage will also require implant removal. In many cases, the fractured screw or implant part can be removed with basic dental hygiene instruments and some patience. Once the fractured screw is visualized using either loupes or microscopic magnification, a solution of chlorhexidine gluconate can be used as irrigation and lubrication to loosen the fractured screw. Any manipulation of the screw should be in a counterclockwise fashion in order to promote backing out of the screw. In certain circumstances, a fine ultrasonic tip on a Cavitron device can help to rotate out the fractured implant component. Careful inspection of all fractured pieces should be done to ensure that all pieces are accounted for and removed. Once removed, an appropriately sized healing abutment should be placed, and imaging should confirm full seating of the newly replaced components. Prior to utilizing the previously placed crown, all efforts should be made to diagnose the etiology of the previous fracture of the restoration. Abutment screws in general are made to tolerate significant forces, but excessive angulation errors (>20°) or poor occlusal planning may lead to screw fracture [41]. These factors should be addressed and corrected in treatment planning for the new restoration.
Читать дальше