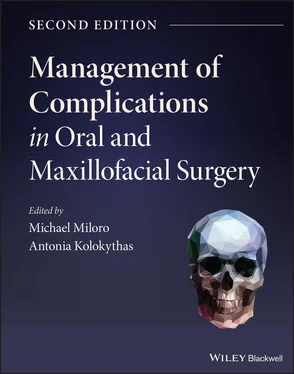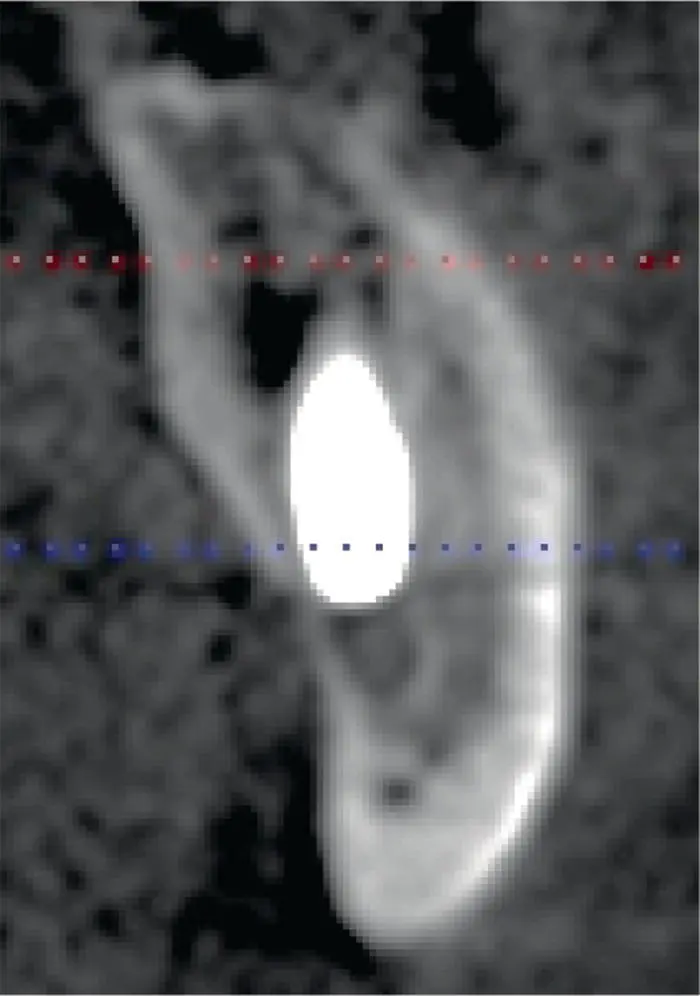
Fig. 3.4. A closer CBCT view of an implant violating the IAC.
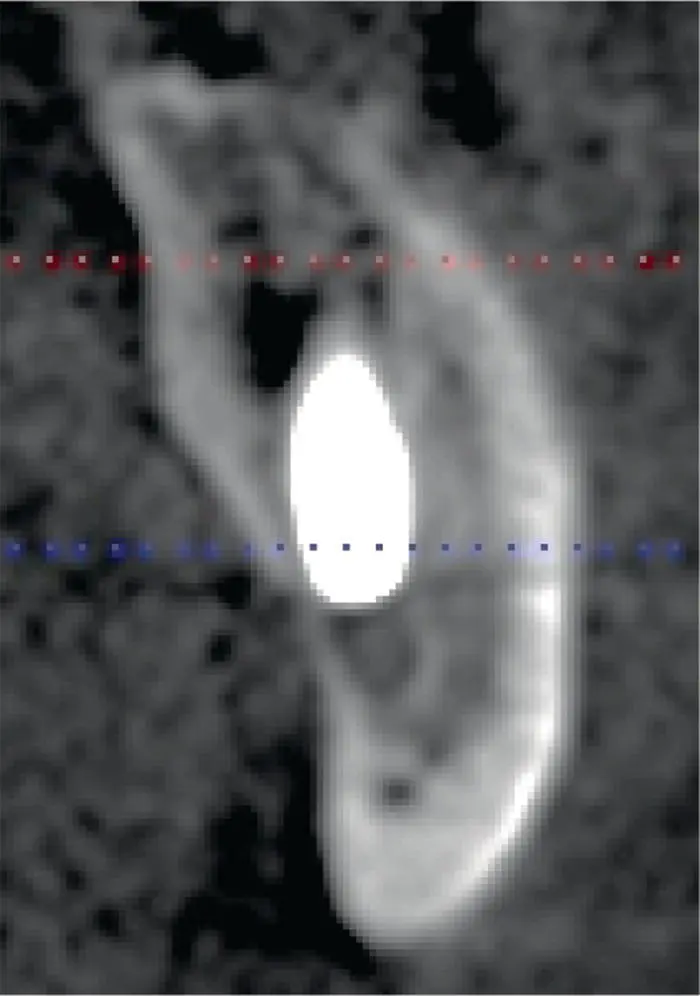
Algorithm 3.1: Nerve Injury
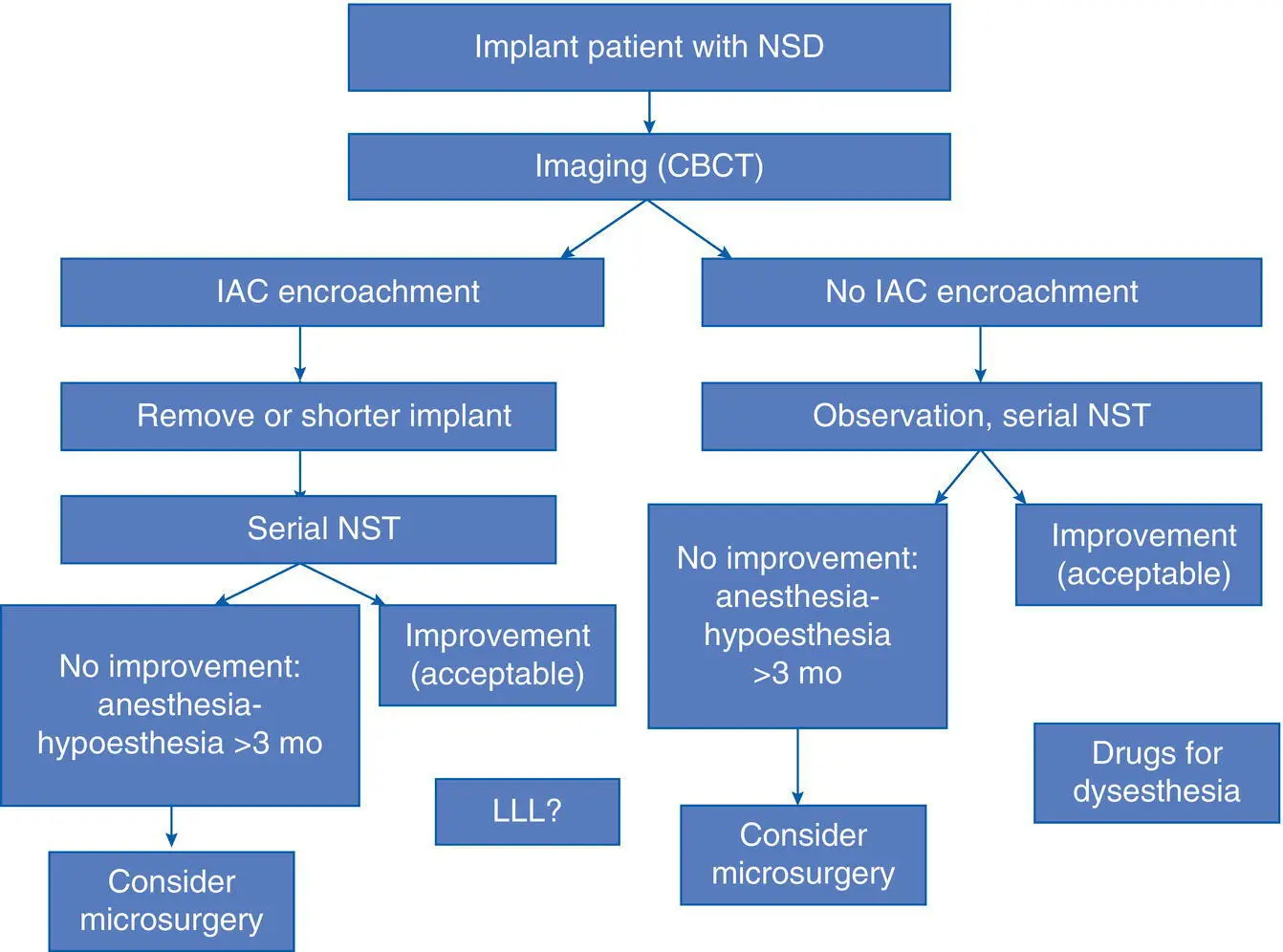
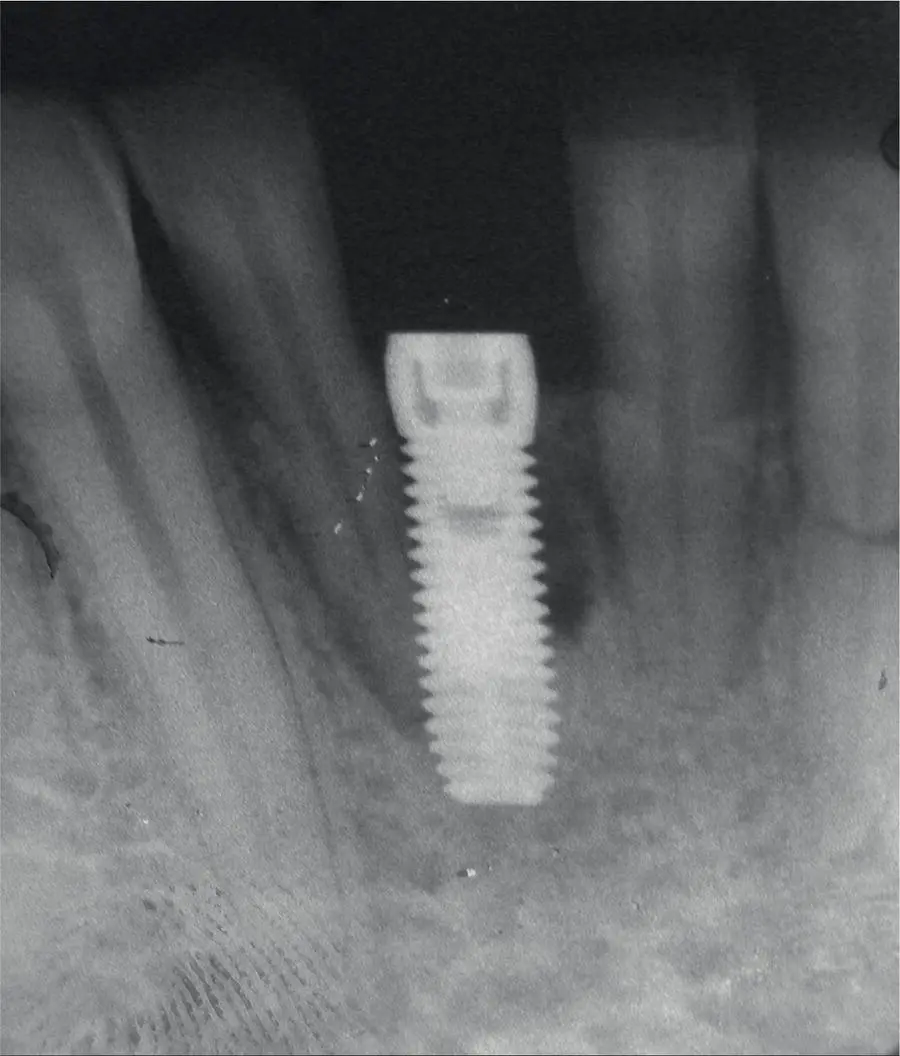
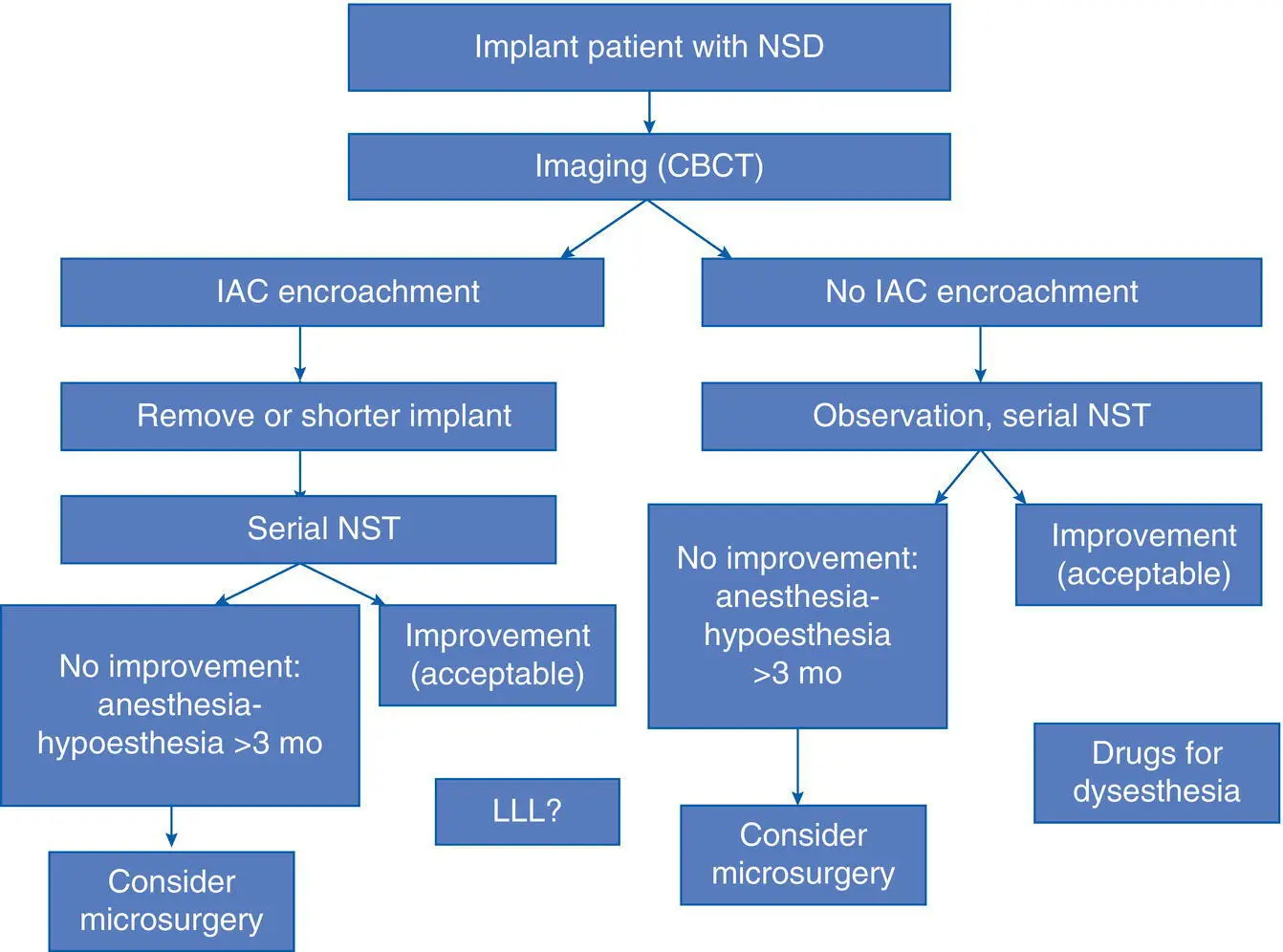
Fig. 3.5. Damage to the adjacent tooth and bone loss due to poor implant position.

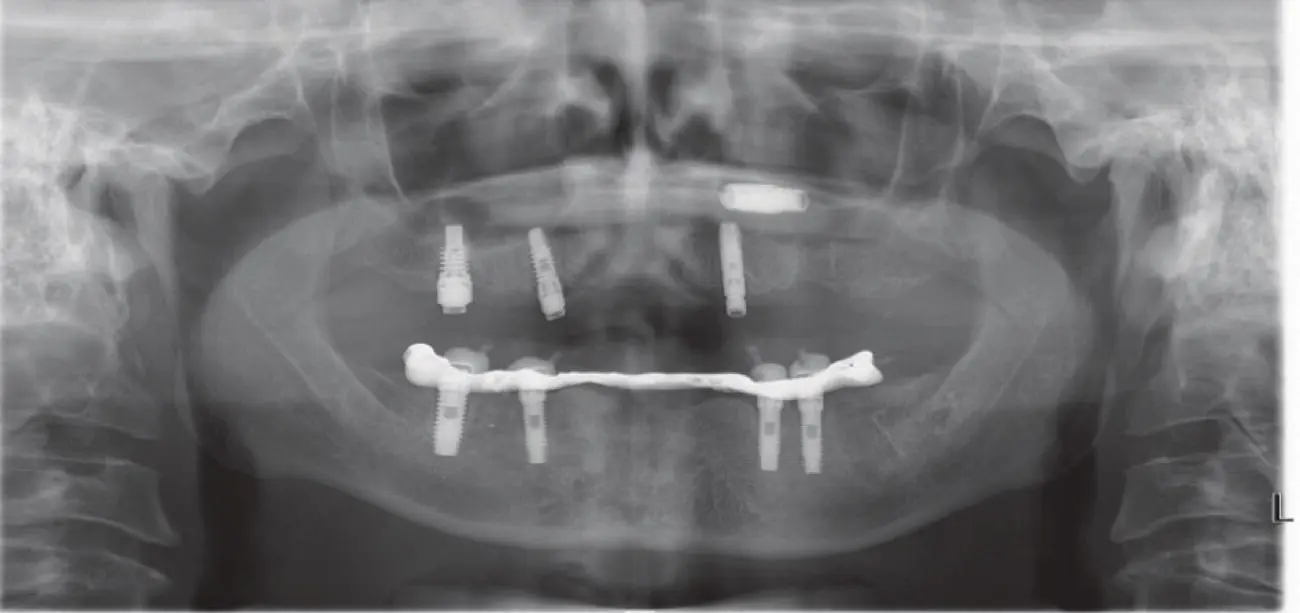
Fig. 3.6. Implants placed too close together compromising gingival esthetics and periodontal health.
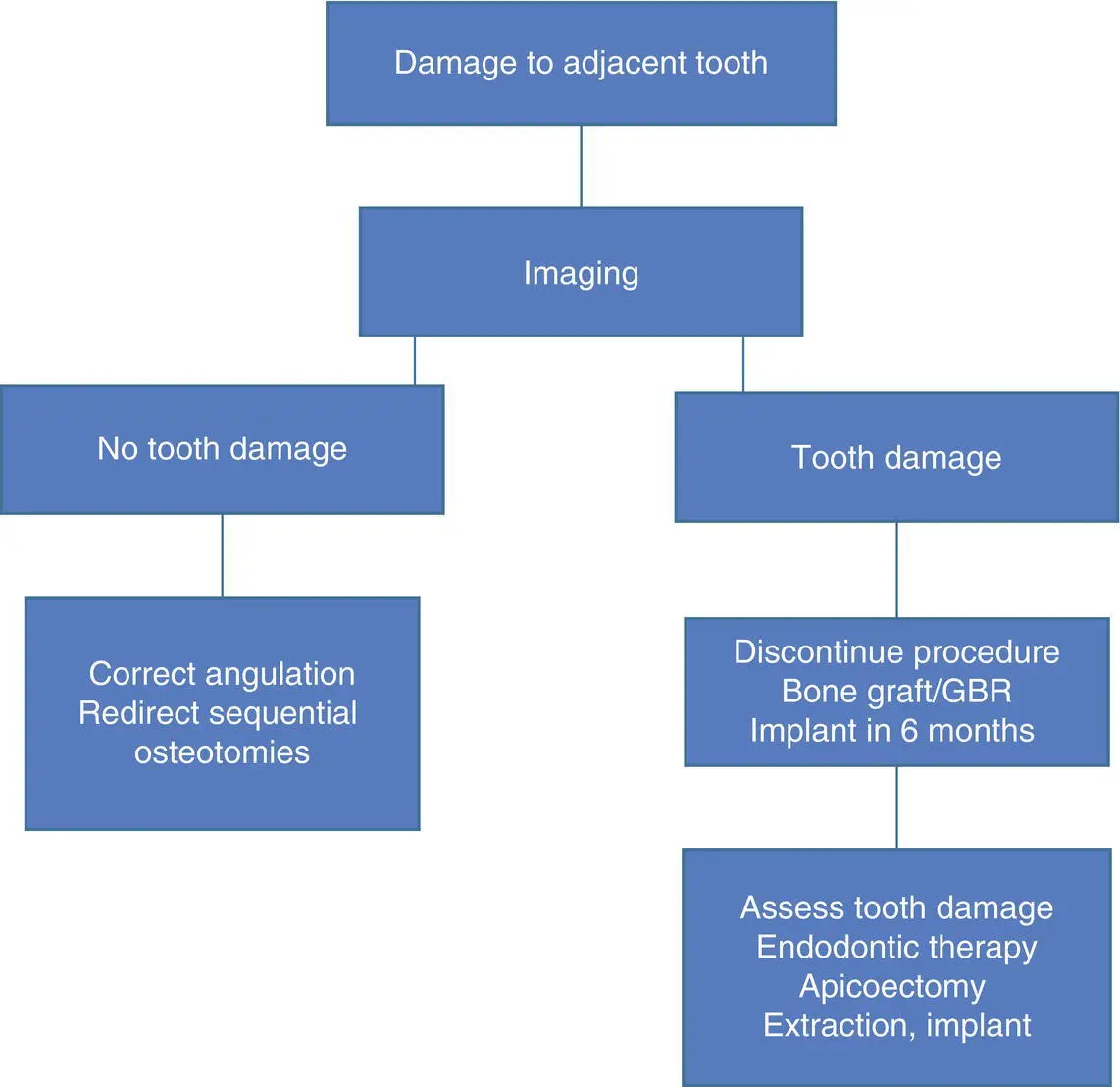
In order to prevent excessive tilting and improper angulation during implant placement, some form of paralleling technique should be utilized by the clinician, if the implants are being placed in a freehand fashion. The use of intraoperative periapical radiographs with a guide pin or implant pilot drill after the initial osteotomy is useful to guide the need for redirection of the implant osteotomy as it is prepared further for implant placement ( Algorithm 3.2). Of course, the use of a CT‐generated surgical guide or dynamic navigation techniques may also be beneficial in reducing the possibility of iatrogenic injury to adjacent teeth. Furthermore, based on a landmark study [22], in order to minimize heat‐induced hard tissue injury and indirect damage to adjacent teeth, copious irrigation at a temperature <47 °C per minute must be maintained. However, as mentioned, it is not possible to irrigate the tip of the drill within the bone (note: internally irrigated drills had been used in the past, but became clogged with bone debris and were not very functional), so sharp, new drills should be used at the correct drill speed to avoid excessive heat generation.
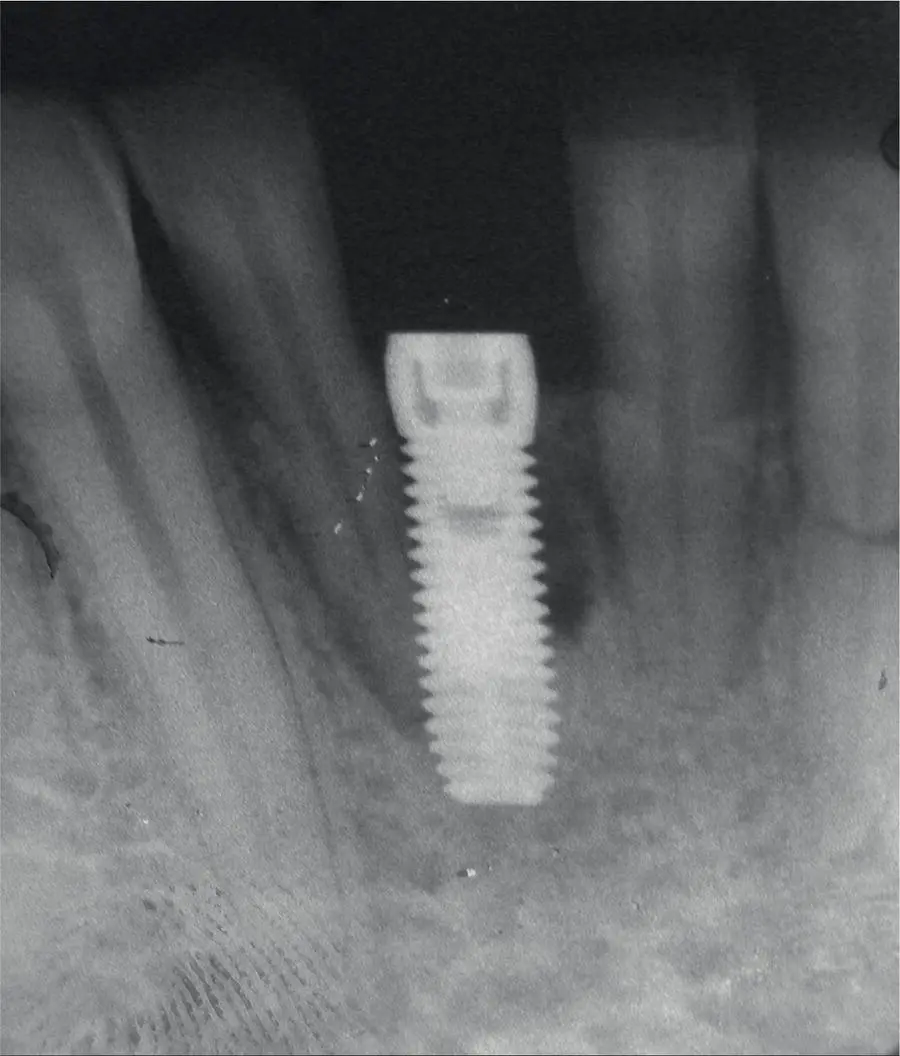
Fig. 3.7. Periapical radiograph showing implants placed too close together resulting in bone loss.
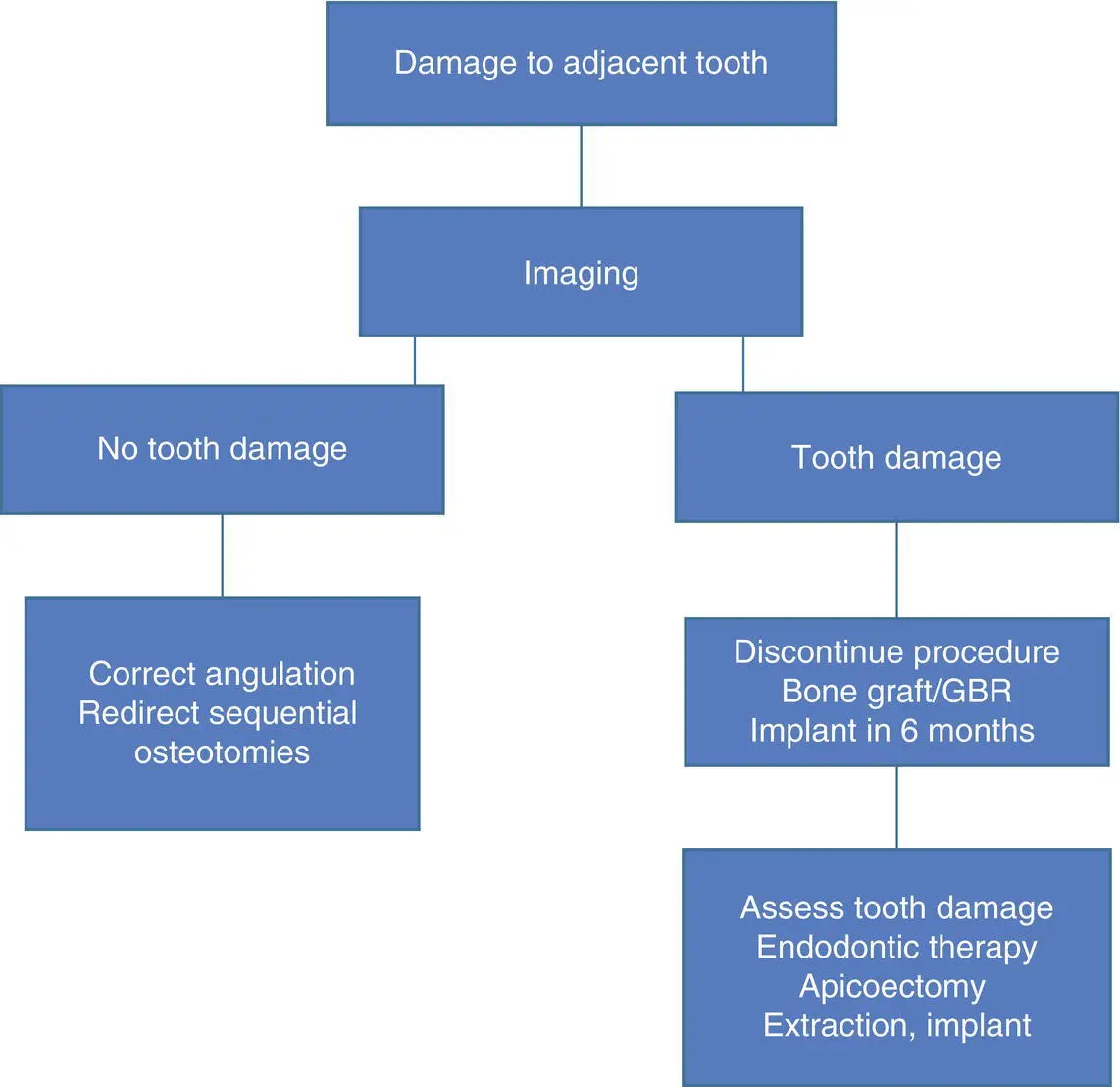
Algorithm 3.2: Damage to Adjacent Teeth
Implant Displacement and Migration
Since iatrogenic displacement of implants may occur during the surgical procedure, it is prudent to include this risk in the informed consent discussion. Due to its location and size, proximity to the posterior maxillary teeth, and poor quality bone in the posterior maxilla, the maxillary sinus is a target site for displaced objects ( Figures 3.8and 3.9). Teeth and tooth roots, root canal filling materials, and dental implants are common objects that are displaced into the maxillary sinus, and case reports in the literature cite these occurrences. Displacement, or migration, of dental implants into the maxillary sinus can be an acute or a delayed event. The causes for an acute displacement include insufficient vertical maxillary bone (<4.0 mm) below the sinus floor, leading to poor primary implant stability, and either immediate or delayed migration of the implant into the sinus. An incorrect surgical plan could be responsible if that plan should have considered the use of sinus floor elevation prior to implant placement to augment bone height for implant stability. Also, the use of improper surgical techniques that violate the Schneiderian membrane or unsuccessful bone regeneration after prior sinus lifting results, again, in insufficient bone to ensure implant stability [23]. More commonly, an implant is displaced at the time of placement, although several reports describe implants that have migrated into the maxillary sinus several weeks, months, or years after initial placement or even after osseointegration and prosthetic restoration has occurred. It is unclear what causes the migration of such implants, but the most accepted reasons are osteopenia/osteoporosis alone, or in combination with excessive occlusal forces, and inflammatory reactions around the implants leading to constant bone destruction and implant mobility [23]. On occasion, the displacement of an implant into the maxillary sinus is found at the middle meatus, or displaced from the nose, due to the action of the mucociliary elevator of the sinus membrane in an attempt to clear the foreign body from the sinus. The treatment of such an incident, whether acute or delayed, includes implant retrieval via a Caldwell–Luc lateral maxillary wall antrostomy, or transnasal endoscopy or transoral endoscopy, and the surgeon may elect to augment the sinus with bone grafting at the same time if another implant is planned in the future in that same site. In rare clinical situations, when a surgeon places a pterygoid implant, the implant can become displaced into the pterygomaxillary or infratemporal fossae. The two known causes leading to this complication are poor primary implant stability and inappropriate surgical techniques usually by using a wider diameter implant and an incorrect inclination of the pterygoid implant during its insertion. A CT‐guided endoscopic removal of a dental implant, whereby the endoscope can be passed through the nasal cavity into the maxillary sinus, terminating into the pterygomaxillary fossa, may be used for implant retrieval. A displaced implant in the infratemporal fossa can be removed preferentially via an intraoral maxillary posterior vestibular approach or a pre‐auricular with hemicoronal approach, if necessary for an implant in a location inaccessible from a transoral approach. In an attempted implant retrieval procedure, further implant displacement can occur, making the process more challenging. Therefore, a waiting period of three to six weeks to allow for adequate fibrosis to occur around the implant in order to stabilize its location may help to facilitate its removal [24, 25]. In these cases, 3D imaging should be used to locate the implant precisely in the soft tissues, and it is possible that CT guidance with needle localization may be required if the implant is in a location that is difficult to access.
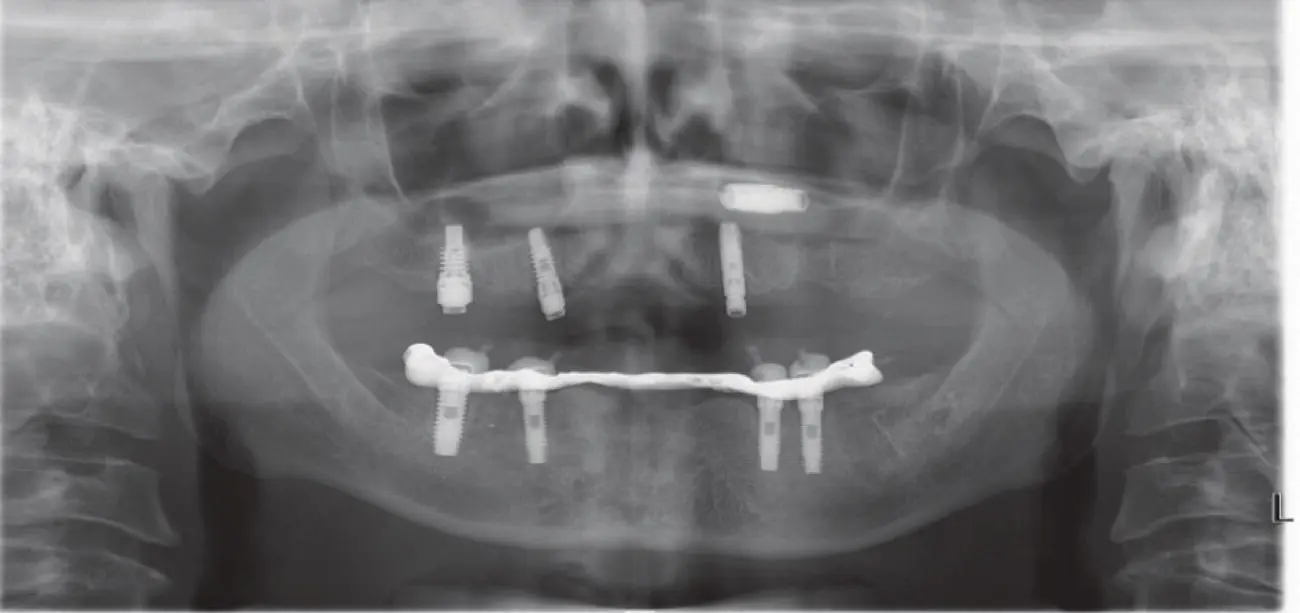
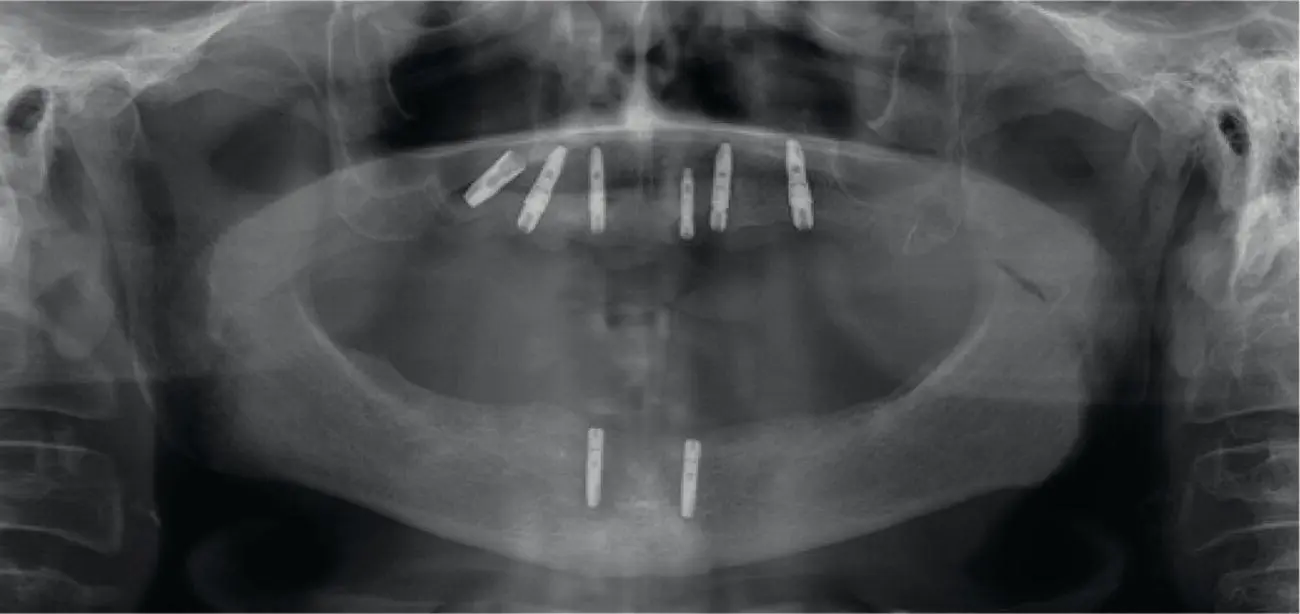
Fig. 3.8. Implant displacement into the left maxillary sinus.
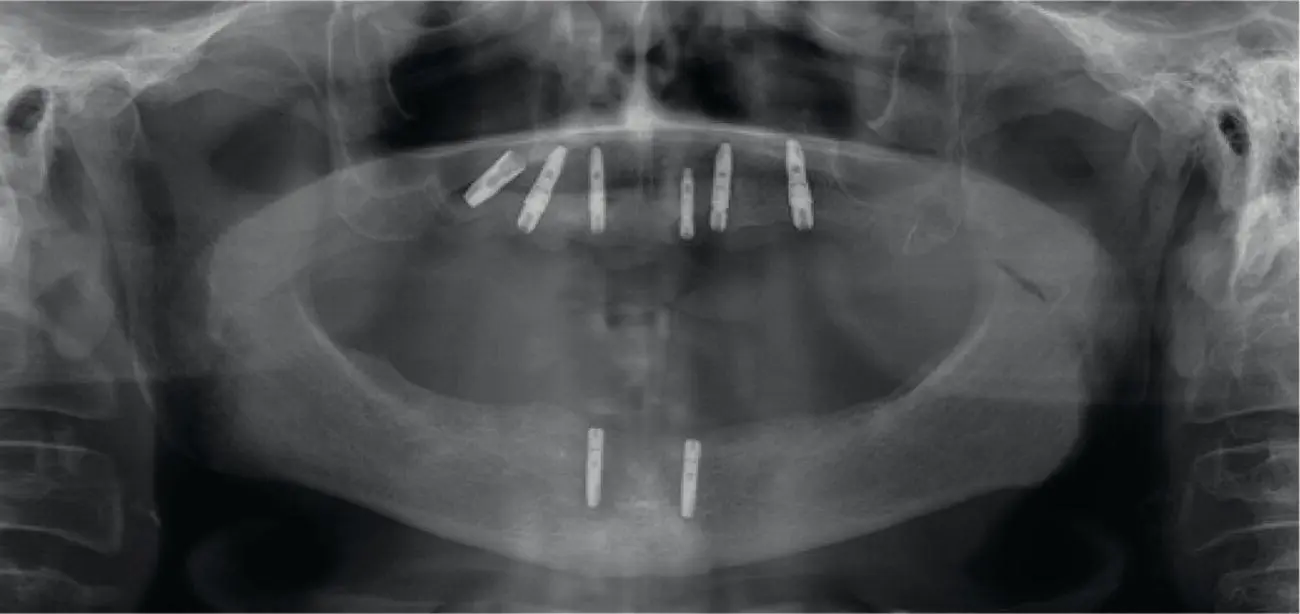
Fig. 3.9. Implant displacement into the right maxillary sinus.
Dental implant displacement can occur not only during a maxillary implant procedure but also during mandibular implant surgery. Involvement of anatomical spaces such as the sublingual and submandibular spaces during implant placement is an uncommon complication. There have been few case reports in the literature for each location, and, in these cases, the implants reportedly migrated to those spaces in a delayed fashion. Poor implant positioning, lack of primary implant stability, violation or resorption of the lingual cortex primarily due to peri‐implantitis, and fracture of the lingual cortex during implant placement are all some reported causes of these complications [26, 27]. Once recognized, a CT scan is used to locate and plan for implant removal. If the displaced implant is present in the sublingual space, an intraoral approach can be utilized, whereas an extraoral approach should be used to access the submandibular space, especially if the implant is not palpable intraorally in the floor of the mouth. Lastly, overdrilling of the osteotomy site with a lack of primary implant stability, and presence of a focal osteoporotic bone marrow defect, can lead to implant displacement into the IAC or the porous marrow of the mandibular body, as discussed previously [28]. After performing a CBCT scan, the implant removal should be achieved via an osteotomy through an intraoral approach ( Algorithm 3.3).
Читать дальше