The large shear strength is due to the bone insertion sites of the ligament and tendon. Characterization of this interface zone of ligament insertion to bone repeatedly found the presence of types II, IX, and X collagen 52, 53that are commonly found in cartilage tissue. In particular, type X collagen is expressed by hypertrophic chondrocytes during endochondral ossification. In the growing bone, type X collagen is co- localized with PGs and appears on the longitudinal septa of hypertrophic cartilage when the bone starts to bear the body weight. 54Type X collagen forms a network of hexagonal mesh and, when embedded in a mineralized tissue, enforces its intrinsic mechanical property. Therefore, type X collagen in the developing bone and the bone insertion sites of the ligament and tendon is thought to generate the significant shear strength to resist gravity and physical activities.
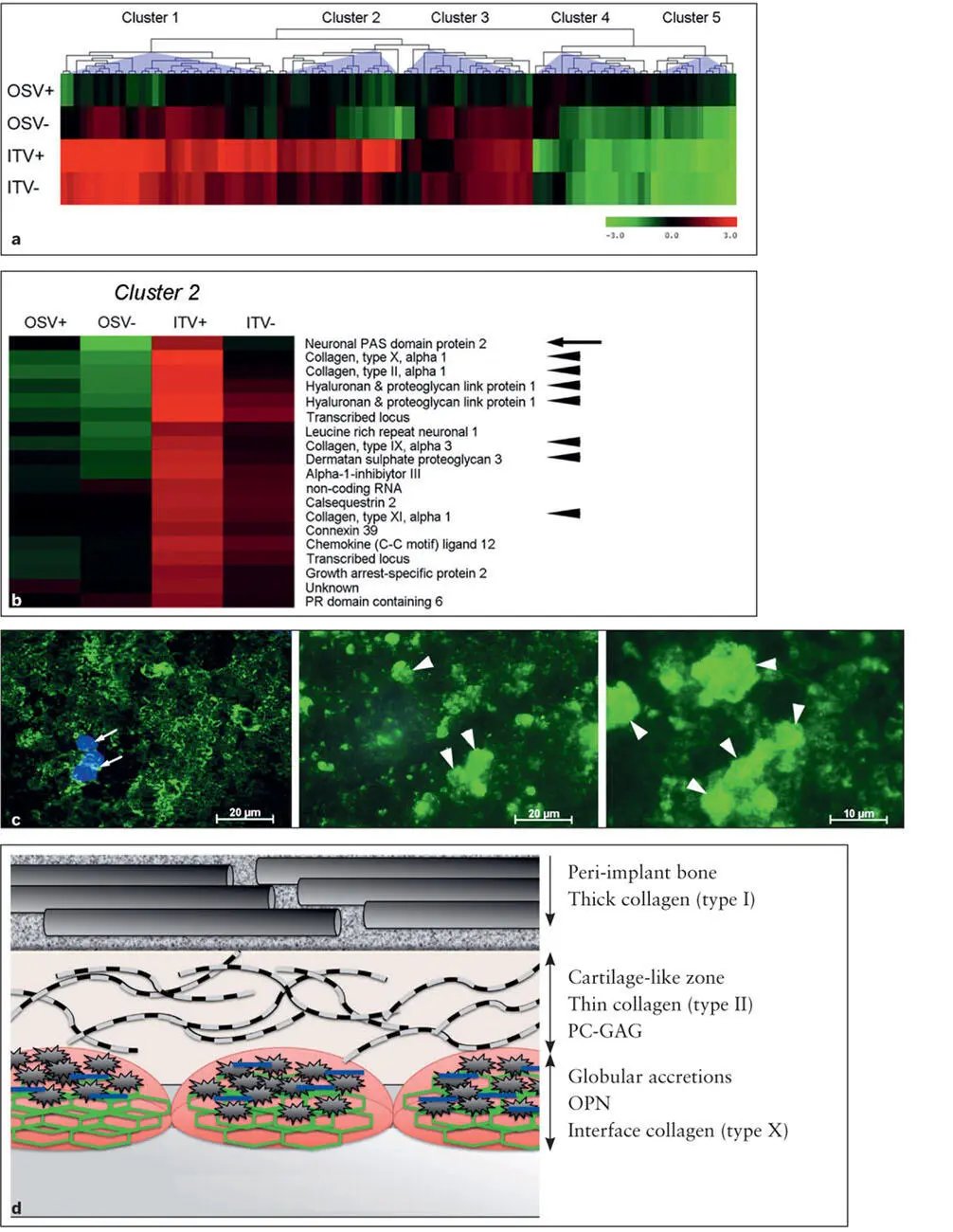
Studies involving DNA microarray reported a puzzling observation: The gene expression profile of peri-implant tissues contained not only bone-related genes but also other genes that were notably of the cartilage molecules. 55– 58Those cartilage-related molecules include PGs; types II, IX, X, and XI collagen; and hyaluronan and PG link protein. 59In other words, the presence of an implant during the healing following osteotomy surgery may create a mixture of bone- and cartilage-related molecules in peri-implant bone. Recently, type X collagen was identified in the interface tissue between bone and implant. 55It may be postulated that cartilage-related molecules such as PGs and type X collagen may be involved in the interface layer between implant and bone, potentially contributing to the shear strength of implant bonding to bone 55( Fig 2-8).
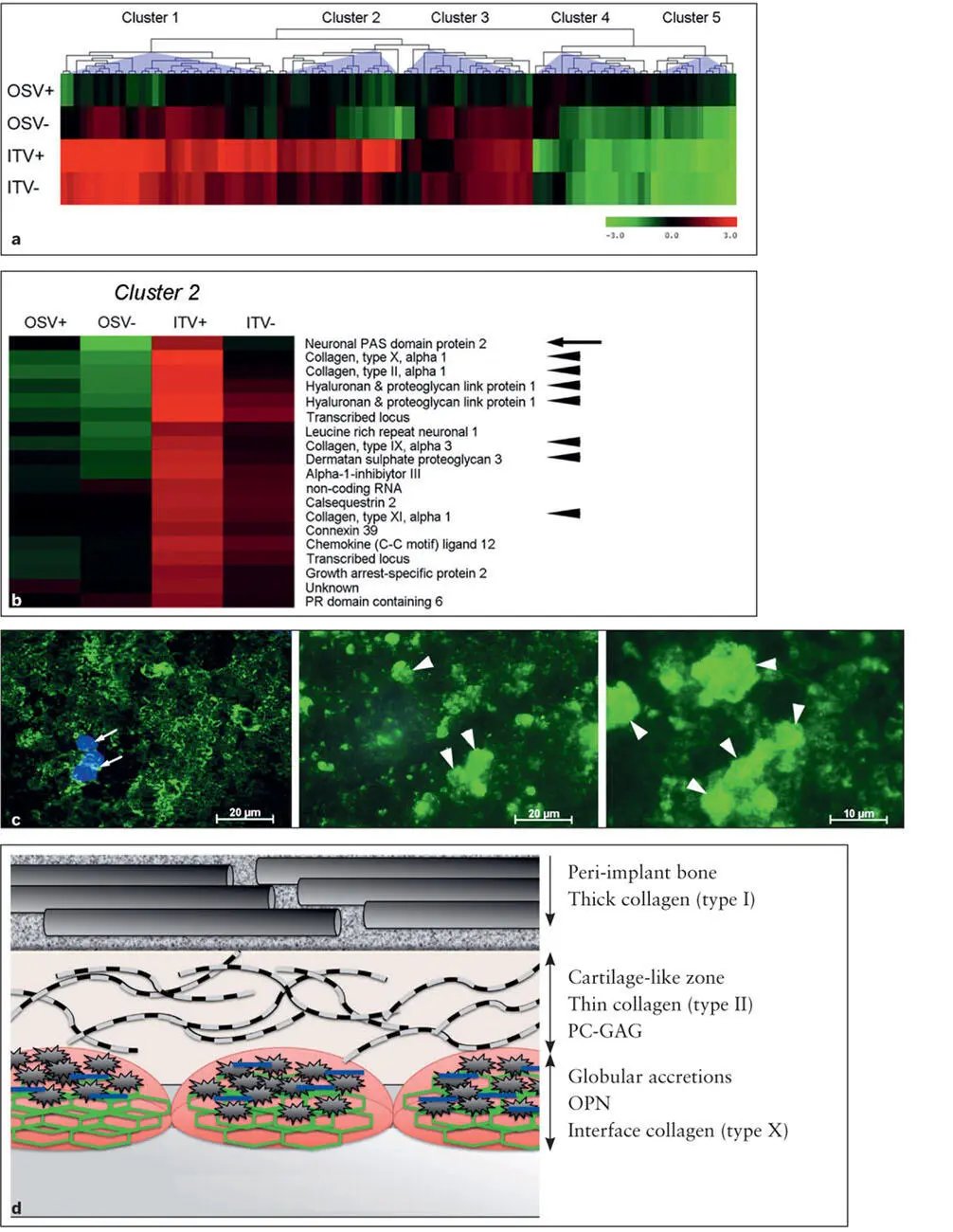
Fig 2-8 (a) The entire genome microarray gene expression of peri-implant tissue. A hierarchical cluster analysis revealed that there were five major gene groups, of which Cluster 2 exhibited the genes most sensitively associated with implant osseointegration. (b) Cluster 2 included cartilage-related ECM genes (arrowheads) . (c) Among cartilage- related genes, type X collagen (green, arrowheads) was identified within the interface zone between the bone and the implant surface. Bone marrow mesenchymal cells (blue) . (Parts a to c reprinted from Mengatto et al 55with permission.) (d) Hypothetical structure and molecular components of the bone- implant interface tissue. The cement line is composed of crystalline calcium phosphate particles (gray sunbursts) in globular accretions containing OPN (blue bars) and type X collagen (green hexagonal mesh) . These molecules may increase the stiffness and shear strength of the cement line. There is a less mineralized and relatively amorphous zone resembling cartilage tissue containing thin and sparsely arranged type II collagen fibers. The cartilage-like zone may also contain PG-GAG molecules, possibly contributing to the shock-absorbing function.
Long-term stability of peri-implant bone
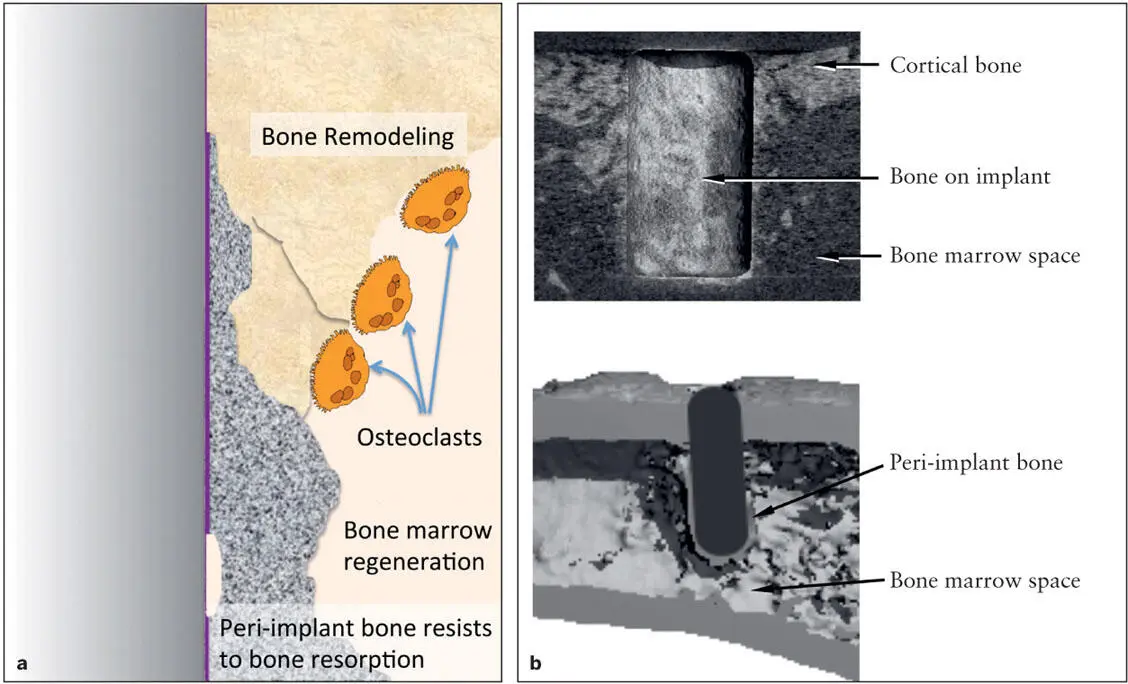
The osteotomy procedure used to prepare an implant placement site creates an ablation wound in the bone marrow. Intramembranous ossification occurs during the healing of bone marrow ablation 60and tooth extraction wounds, 61thus leading to the formation of woven bone trabeculae in the marrow space. The trabecular bone formed in response to ablation wounding is then subjected to intensive remodeling and largely resorbed to create fatty bone marrow ( Fig 2-9). Uniquely, bone tissue formed in the vicinity of implant surfaces appears to resist this catabolic bone remodeling and thus maintains the osseointegration for an extended period. 2Trabecular bone derived from distance osteogenesis may be relatively unstable and can disappear due to physiologic bone remodeling. On the contrary, peri-implant bone derived from contact osteogenesis appears to undergo slower bone marrow remodeling and remains around the implant for the long term (see Fig 2-9).
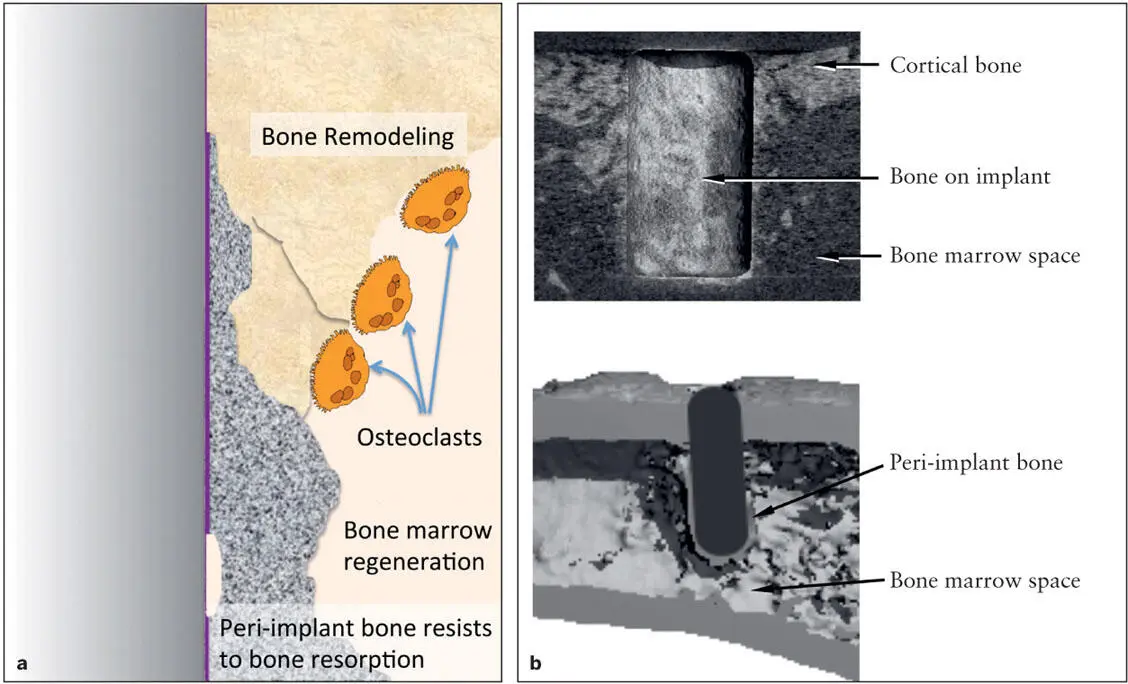
Fig 2-9 (a) A diagram of bone marrow ablation healing around an implant. The newly formed bone around the implant is subjected to osteoclastic bone resorption, regenerating the bone marrow space. It has been noted that peri-implant bone resists bone resorption activity. (b) MicroCT- reconstructed 3D picture depicting the persistent presence of peri-implant bone, with the surrounding bone marrow having lost its trabecular structure, in an experimental animal model using rats.
The rapid formation of bone marrow trabecular bone, perhaps with the woven bone characteristics, may occur 1 to 2 weeks after implant placement and may potentially contribute to the immediate implant stability. Whether the early woven bone can support the occlusal load has not been established. While the majority of woven bone may be resorbed, the remaining bone structures continue to mature. During the transition stage from woven bone resorption to the maturation of the small but well-organized trabecular bone, there may be a vulnerable period in which the degree of implant integration may temporarily decrease. This phenomenon has been observed in an animal model (Nishimura et al, unpublished data); however, its clinical significance has not been established.
Bone resorption is facilitated by osteoclasts. Osteoclasts are formed by fusion of monocytes under a combination of chemical cues including receptor activator of nuclear factor κB (RANK) ligand, or RANKL. During the developmental stage, RANKL is secreted from osteoblasts and hypertrophic chondrocytes. However, when bone is matured, RANKL is primarily secreted from osteocytes embedded in bone, which sensitively respond to mechanical stimuli such as occlusal loading. 62As discussed previously, the mechanical property of peri-implant bone may be harder than that of surrounding trabecular bone. It is conceivable that the increased mechanical properties of peri-implant bone may reduce the amount of matrix deformation that the embedded osteocytes experience, leading to reduced RANKL secretion under the normal occlusal force. Above a critical load threshold for peri- implant bone osteocytes, however, implant overloading can stimulate the osteocytes to initiate the secretion of RANKL, resulting in osteoclast formation and bone resorption. The role of mechanical loading on bone remodeling is discussed in further detail in chapter 3.
Osteoclasts strongly adhere to bone surface and form a ringlike apparatus, referred to as the sealing zone . Osteoclasts create an acidic milieu within the sealing zone and secrete proteinases such as cathepsin K to degenerate the organic matrix of bone. As a result, bone mineral HA and collagen matrix are removed. The osteoclast adhesion to the bone surface is required for this bone resorption process. It has been reported that the adhesion of osteoclasts is influenced by the bone surface topography. When mouse osteoclasts were cultured on titanium disks with different surface roughness ranging from 1 to 4.5 µm Ra, the sealing zone formation was shown to be disturbed by microtopographic obstacles. 63There was an inverse correlation between the stability of the osteoclast ring (ie, the structural integrity and sealing zone translocation rate of osteoclasts) and the increasing microtopography.
Because the adhesion of osteoclasts appears to be less effective on a rough surface, it may be postulated that the surface topography of peri-implant bone may be rougher than that of surrounding trabecular bone. The placement of an implant appears to influence biochemical compositions of peri-implant bone. Cartilage and bone comprise the major skeletal system, and both contain ECM such as collagen. There are distinct differences in the composition of ECM molecules; ie, types I and V collagen are predominant in bone, whereas types II, IX, X, and XI collagen are in cartilage. However, recent studies indicate that peri-implant bone may be composed of a mixture of bone and cartilage ECM. In a mouse model lacking type IX collagen, one of the cartilage ECM molecules was shown to develop an age-related osteoporosis-like phenotype. 64Type IX collagen maintains the space between the adjacent collagen fibers and has been shown to exist in a small amount in bone. The lack of type IX collagen appeared to manifest as a dense bone collagen network, resulting in the smoother bone surface. Osteoclasts were found to adhere widely to this mutant bone surface. Although highly speculative, the reduced susceptibility of peri-implant bone to osteoclastic bone resorption may in part be facilitated by its different biochemical compositions, such as increased type IX collagen, and bone surface topography.
Читать дальше