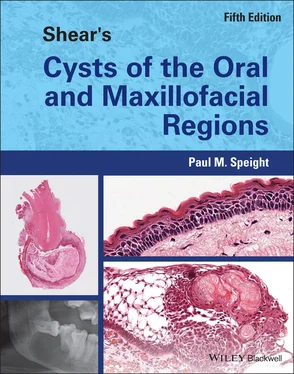
Paul M. Speight - Shear's Cysts of the Oral and Maxillofacial Regions
Здесь есть возможность читать онлайн «Paul M. Speight - Shear's Cysts of the Oral and Maxillofacial Regions» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Shear's Cysts of the Oral and Maxillofacial Regions
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:5 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 100
- 1
- 2
- 3
- 4
- 5
Shear's Cysts of the Oral and Maxillofacial Regions: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Shear's Cysts of the Oral and Maxillofacial Regions»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Shear’s Cysts of the Oral and Maxillofacial Regions
Shear’s Cysts of the Oral and Maxillofacial Regions Fifth Edition
Shear's Cysts of the Oral and Maxillofacial Regions — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Shear's Cysts of the Oral and Maxillofacial Regions», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Ward et al. (2004 ) used mathematical modelling to simulate odontogenic cyst growth. They assumed a spherical cyst lined by a semi‐permeable membrane and with a central osmotic pressure as a result of accumulation of degraded cellular material. The model supported the conclusions of the early experimental work, that osmotic pressure played an important part in cyst growth. Interestingly, the model also confirmed the findings of Kubota et al. (2004 ), and suggested that as the cyst became larger, osmotic pressure played a lesser part and cell proliferation became more important.
Osmotic pressure must be maintained by a high concentration of soluble proteins in the cyst fluid. Electrophoretic studies (Toller and Holborow 1969 ; Toller 1970a ) demonstrated that radicular cyst fluids contained small molecular‐sized albumin and β 1‐globulin in quantities comparable with the patient's serum, but had fewer, if any, of the larger protein molecules. α‐ and β 2‐ globulins were greatly diminished or absent, and γ‐globulins (mainly immunoglobulins) varied greatly in quantity, but were most often found in inflamed cysts. They showed that more than half display levels of immunoglobulins much higher than the patient's own serum. In 19 cyst fluids in which levels of IgG, IgA, and IgM were measured independently, all three were significantly raised in most of the non‐keratinising cysts. Immunofluorescent staining showed that lymphoid cell aggregates in the walls of radicular cysts often included numerous plasma cells.
Skaug (1973 , 1974 , 1976b , 1977 ) confirmed that fluid from non‐keratinising jaw cysts contained high concentrations of proteins, including immunoglobulins, but supported the view that accumulation of cyst fluid resulted essentially from inadequate lymphatic drainage of the cyst cavity. He suggested that plasma protein exudate and hyaluronic acid, as well as the products of cell breakdown, contributed to the high osmotic pressure of the cyst fluid.
These data suggest that the accumulation of proteins in the cyst lumen is a combination of a serum exudate, an inflammatory exudate, and breakdown products of cells, including luminal epithelial cells and inflammatory cells. It is likely therefore that the luminal pressure, necessary for cyst expansion, is greatest when the cyst is most inflamed, at earlier stages of development. As a cyst gets larger and matures, inflammation may subside, the rate of growth will slow, and a state of equilibrium may be reached. This is supported by the study of Kubota et al. (2004 ) and the model proposed by Ward et al. (2004 ), who both show that pressure and the rate of growth decrease with size of the lesion.
Although osmotic pressure may provide the stimulus for expansion, it does not operate alone and, as mentioned above, a complex cascade of molecular events is responsible for growth. Growth must be accompanied by further epithelial proliferation, and by degradation of adjacent connective tissues and bone resorption.
Epithelial Proliferation
The stimuli for epithelial proliferation have been discussed previously, but in an established cyst LPS plays a less important role, and epithelial growth is sustained by cytokines and growth factors resulting from the inflammatory response ( Table 3.2) (Bernardini et al. 2015 ; Silva et al. 2007 ; Lin et al. 2007 ; Nair 2004 ). However, as the cyst matures and inflammation subsides, the rate of cell proliferation may be relatively low. Soluk Tekkeşın et al. (2012a) showed that only about 1.0% of cells were positive for Ki‐67 in the epithelial lining of radicular cysts, compared to 2.0% or more in odontogenic keratocysts. They also found that radicular cysts showed higher levels of the pro‐apoptotic protein Bax and low levels of bcl‐2, suggesting that low levels of proliferation are accompanied by high levels of apoptosis. Others have identified apoptotic markers in radicular cysts and have suggested that this contributes to their slow growth (Loreto et al. 2013 ). As the cyst continues to expand, this slow proliferation and high levels of apoptosis probably lead to the thinning of the epithelial lining that is seen in long‐standing and residual cysts ( Figure 3.11).
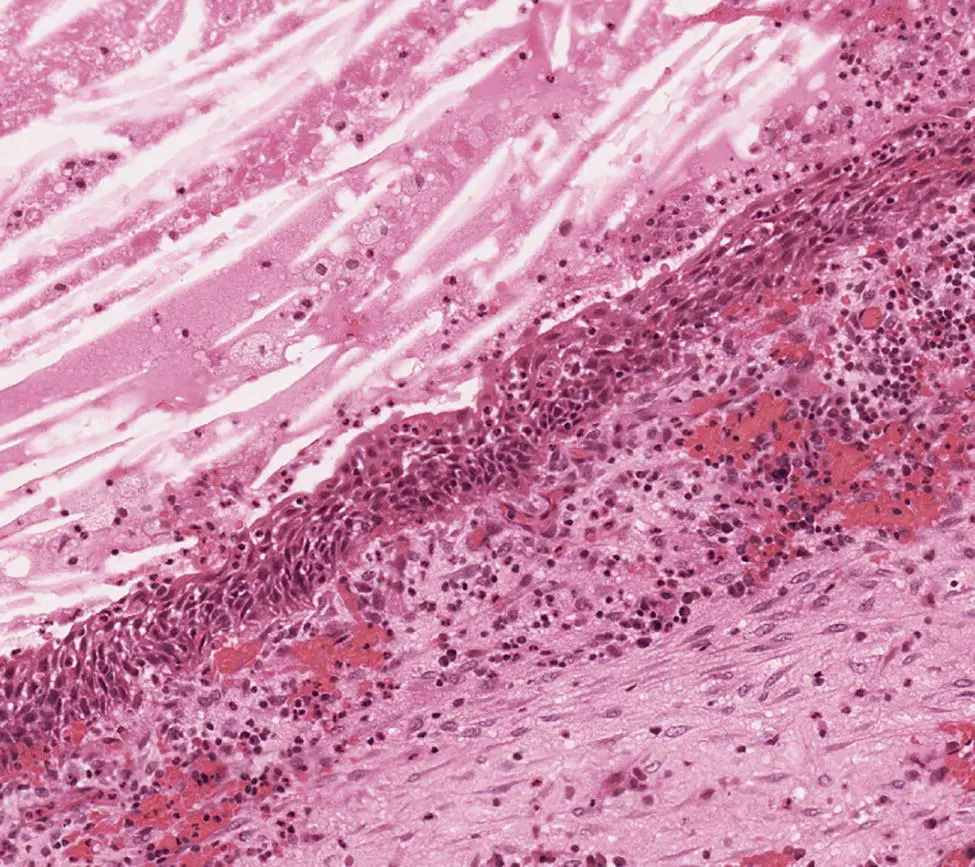
Figure 3.11 A long‐standing radicular cyst. The cyst wall has become fibrous with little inflammation and the epithelial lining is relatively thin and regular. Note the considerable cellular and proteinaceous debris in the lumen (top left).
Degradation of the Connective Tissues and Bone Resorption
The next crucial element of cyst growth is degradation of the connective tissues. Among the most important and widely studied factors are the matrix metalloproteinases (MMPs). These are a large family of calcium‐dependent and zinc‐containing proteases, capable of degrading a wide range of extracellular matrix proteins. A number of studies have shown expression of MMPs in odontogenic cysts, including the gelatinases (MMP‐2 and MMP‐9; Teronen et al. 1995a ; Kubota et al. 2000 ; D'addazio et al. 2014 ; Alvares et al. 2017 ; Andrade et al. 2017 ) and collagenases (MMP‐1, MMP‐8, and MMP‐13; Teronen et al. 1995b ; Lin et al. 1997 ; Wahlgren et al. 2001 ; D'addazio et al. 2014 ; Andrade et al. 2017 ), suggesting a role for these enzymes in cyst growth and development. Furthermore, MMP activity increases with the intensity of inflammation and is often more prominent in periapical granulomas than in established cysts (Lin et al. 1997 ; Andrade et al. 2017 ). In keeping with this, inflammatory cytokines, especially IL‐1, up‐regulate active MMP‐9 in odontogenic cysts (Kubota et al. 2000 ) and increased numbers of mast cells are associated with MMP activation in odontogenic cysts (Teronen et al. 1996 ; Rodini et al. 2008 ; Andrade et al. 2017 ). Inflammation in radicular cysts is also associated with secretion of neutrophil collagenase (MMP‐8) and with increased expression of plasminogen activator (Tsai et al. 2004 ), which indirectly forms plasmin that may also activate MMPs.
All odontogenic cysts are encased in the bone of the jaws, and therefore any expansion must be associated with bone resorption. Normal bone undergoes continuous remodelling controlled by a number of factors, the most important of which are receptor activator of nuclear factor kappa B (RANK), its ligand (RANKL), and osteoprotegerin (OPG, also known as osteoclastogenesis inhibitory factor). These form the RANKL/RANK/OPG system, which is primarily responsible for bone homeostasis (Graves et al. 2011 ; Kular et al. 2012 ). RANK is expressed on the surface of osteoclasts and their precursor cells and when bound by RANKL promotes osteoclast formation and maturation. OPG secreted by osteoblasts acts as a decoy receptor and binds RANKL to prevent activation by RANK. RANKL is primarily cell bound on the surface of osteoblasts and in normal bone osteoblast–osteoclast interactions is the main method of bone turnover regulation. In pathological conditions, however, RANKL may be secreted by osteoblasts and a number of other cell types, including Th1 lymphocytes, endothelial cells, and epithelial cells, and may function as a soluble receptor. It should also be noted that RANKL is the only cytokine that can stimulate osteoclastogenesis, although a number of other factors support recruitment of osteoclast precursors, or promote osteoclast maturation and activation ( Table 3.2).
Perturbation of the RANKL/RANK/OPG system is involved in all pathological conditions associated with bone resorption, and many studies have now provided evidence for its role in increased osteoclast activity in many odontogenic lesions, including radicular cysts (Tay et al. 2004 ; Menezes et al. 2006 ; da Silva et al. 2008; de Moraes et al. 2011 ; Graves et al. 2011 ; Soluk Tekkaşin et al. 2011 ; Belibasakis et al. 2013 ).
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Shear's Cysts of the Oral and Maxillofacial Regions»
Представляем Вашему вниманию похожие книги на «Shear's Cysts of the Oral and Maxillofacial Regions» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Shear's Cysts of the Oral and Maxillofacial Regions» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.