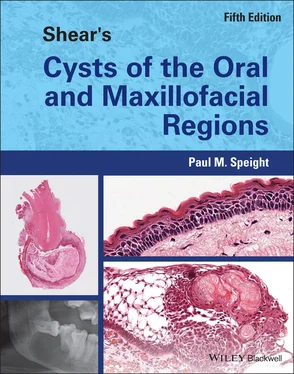
Paul M. Speight - Shear's Cysts of the Oral and Maxillofacial Regions
Здесь есть возможность читать онлайн «Paul M. Speight - Shear's Cysts of the Oral and Maxillofacial Regions» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Shear's Cysts of the Oral and Maxillofacial Regions
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:5 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 100
- 1
- 2
- 3
- 4
- 5
Shear's Cysts of the Oral and Maxillofacial Regions: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Shear's Cysts of the Oral and Maxillofacial Regions»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Shear’s Cysts of the Oral and Maxillofacial Regions
Shear’s Cysts of the Oral and Maxillofacial Regions Fifth Edition
Shear's Cysts of the Oral and Maxillofacial Regions — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Shear's Cysts of the Oral and Maxillofacial Regions», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Tay et al. (2004 ) were the first to demonstrate that RANKL was expressed in osteolytic lesions of the jaws, including radicular cysts. RANKL was expressed in the fibrous wall of radicular cysts, and its association with osteoclast recruitment was confirmed by the demonstration of tartrate‐resistant acid phosphatase (TRAP) and calcitonin‐receptor positive osteoclasts adjacent to the RANKL‐positive cells. In a more detailed analysis, Menezes et al. (2006 ) confirmed these findings, but were also able to demonstrate that RANKL and OPG were expressed by a range of cell types, including PMNs, lymphocytes, macrophages, endothelial cells, and the epithelial lining of radicular cysts. They found that RANKL was more highly expressed than OPG and that expression was greater in cysts than granulomas. Other studies have shown similar levels of expression, but have also shown, as would be expected, that RANKL expression is not specific to radicular cysts and is also found at similar or even greater levels in dentigerous cysts, odontogenic keratocysts, and ameloblastomas (Tay et al. 2004 ; Menezes et al. 2006 ; de Moraes et al. 2011 ; Soluk Tekkaşin et al. 2011 ). It is likely that the level of expression at any moment in time will be related to the degree of ‘maturation’ of the cyst or to the extent of inflammation. Kawashima et al. (2007 ) studied the kinetics of RANKL, RANK, and OPG expression in experimentally induced periapical lesions in rats. They showed that all three factors peaked at between two and three weeks, but that the greatest increase was in RANKL, with the highest RANKL/OPG ratios at this time. They also found that RANKL was expressed in a range of cell types, but these were close to the alveolar bone and were associated with activated osteoclasts. The up‐regulation of the RANKL/RANK/OPG system also correlated to increased expression of pro‐inflammatory cytokines, known to be able to activate RANKL, including IL‐1α and IL‐1β. Similar data have been presented in a number of subsequent studies (reviewed in da Silva et al. 2008 ; Graves et al. 2011 ; Belibasakis et al. 2013 ), confirming the role of inflammatory cytokines and the close association between the inflammatory response and bone resorption.
The most important cytokines involved in the process are indicated in Table 3.2, and include IL‐1α (which was originally called osteoclast‐activating factor, OAF), IL‐6, and TNF‐α. A range of chemokines are also responsible for chemotaxis of osteoclast precursors and differentiation of osteoclasts, including CXCL8/IL‐8, which has been mentioned previously as an important initiator of the process, since it is up‐regulated by LPS and also chemotactic to PMNs. Prostaglandins have also been shown to be important mediators of bone remodelling and may act to stimulate both bone deposition and resorption. There are a number of prostaglandins, but PGE 2is particularly important in bone resorption, since it stimulates expression of RANKL and inhibits OPG on osteoblasts (Blackwell et al. 2010 ). Early studies by Harris and his research group (Harris and Goldhaber 1973 ; Harris et al. 1973 ; Harris 1978 ; Meghji et al. 1989 ) were the first to demonstrate that cultures of cyst walls had potent bone‐resorbing activity, and identified prostaglandins as a key factor. Matejka et al. (1985a ,b , 1986 ) confirmed these findings and also demonstrated that the granulation tissue and the inflammatory cells in the wall of radicular cysts were the main source of PGE 2.Further studies from Harris's group (Bando et al. 1993 ; Meghji et al. 1996 ) reinforced these findings and also showed that IL‐1 and IL‐6 were the predominant cytokines with bone‐resorbing activities. In immunocytochemical studies, Bando et al. (1993 ) showed that these cytokines appeared to be synthesised primarily by the epithelial cells of the cyst lining. Kusumi et al. (2004 ) also showed that IL‐6 was the predominant cytokine in radicular cysts and found evidence for synthesis by fibroblasts in the cyst wall.
Histopathology
From the foregoing account of pathogenesis, it is clear that on histological examination a periapical lesion may show a wide variety of features. Over 100 years ago Thoma (1917 ) described five types of lesion that may be encountered in association with a non‐vital tooth. To paraphrase his descriptions into contemporary terminology, the five lesions were periapical granuloma, periapical abscess, periapical granuloma with proliferating epithelium, periapical granuloma with early cyst formation, and radicular cyst. However, we should not regard these as individual lesions, but as a continuum of changes that reflect the pathogenic pathway, with a fully developed cyst as the end result.
Some have suggested that a diagnosis of a cyst can only be made after examination of multiple serial sections to confirm the presence of a true cavity with an epithelial lining (Simon 1980 ; Nair et al. 1996 ; Ricucci and Bergenholtz 2004 ), but this is not practical or sustainable in routine clinical practice. The diagnostic histopathologist rarely receives an intact specimen, or a specimen still in continuity with the offending root apex. This is because a periapical lesion is often surgically removed during an apicectomy operation, where the apex of the tooth and associated soft tissue are removed and a filling material is placed in the root canal, thus enabling preservation and restoration of the affected tooth. Therefore, the pathologist often receives the lesion as a fragmented or irregular curettage specimen from which the diagnosis of a cyst must be deduced, in the context of the orientation of the tissues and the clinical and radiological findings. An intact specimen may be a spherical or ovoid cystic mass, but often they are irregular and collapsed. Lesions are usually 10–15 mm in diameter and rarely exceed 30 mm. The walls vary from extremely thin to a thickness of about 5 mm. As with all cystic lesions, it is important to examine the inner surface of the cyst. This may be smooth or corrugated, but mural nodules or thickenings may be seen, which often represent accumulations of cholesterol or hyaline (Rushton) bodies projecting into the lumen. The fluid contents are usually watery and brown from the breakdown of blood, but when cholesterol crystals are present they impart a shimmering gold or straw colour. Pathologists must also recall that a radicular cyst is always associated with a non‐vital tooth. If this is not the case, then an alternative diagnosis must be sought, usually needing careful correlation with clinical and radiological findings.
On histological examination, the key diagnostic criterion is to identify a variably inflamed fibrous cyst wall lined wholly or in part by stratified squamous epithelium ( Figure 3.12). The epithelial lining may be discontinuous and ranges in thickness from 1 to 50 cell layers. The majority are 6–20 cell layers thick. The nature of the lining may depend on the age or stage of development of the cyst, or on the intensity of the inflammation. In early cysts, the epithelial lining may be proliferative and show a characteristic arcading with an intense associated inflammatory process ( Figure 3.12), but as the cyst enlarges the inflammation may subside and the lining becomes thin and regular, with a certain degree of differentiation to resemble a simple non‐keratinised stratified squamous epithelium. In well‐developed cysts, the lining may vary. At sites of heavy inflammation, often adjacent to the tooth root, the epithelium may be proliferative and thickened, but away from the tooth the wall is often less inflamed and the lining becomes thin and regular ( Figure 3.11). Long‐standing cysts and residual cysts in particular may be lined by a thin, regular lining of stratified squamous epithelium ( Figure 3.13).
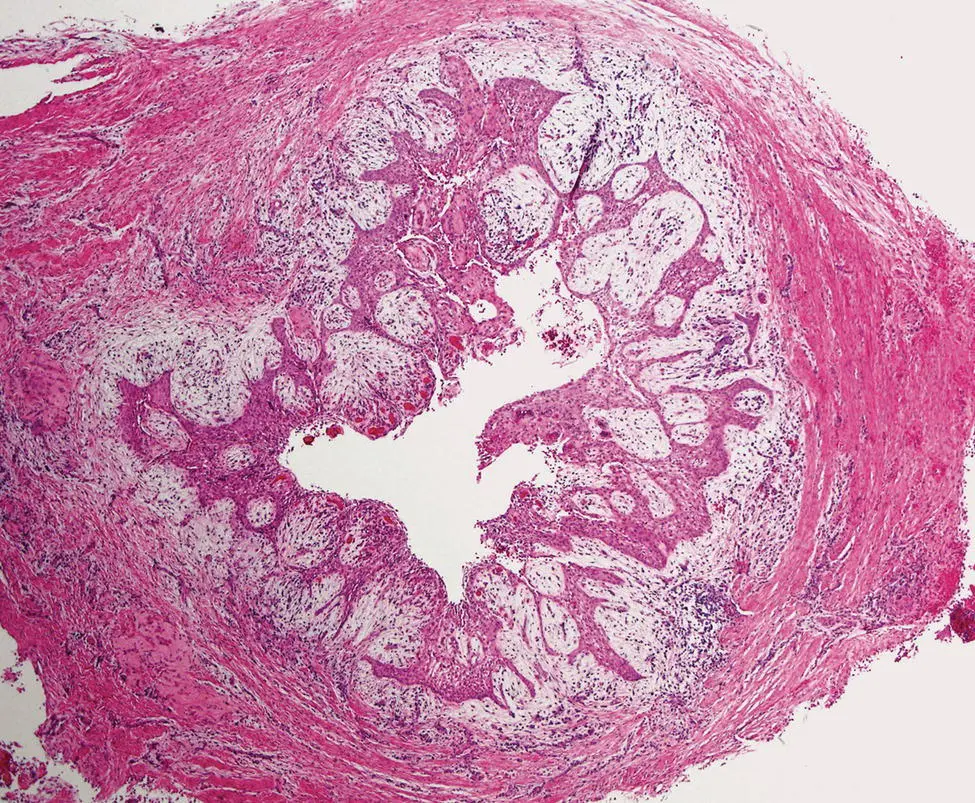
Figure 3.12 Radicular cyst. The cyst has a thick fibrous wall. The lumen is lined by proliferating and arcading epithelium.
Читать дальшеИнтервал:
Закладка:
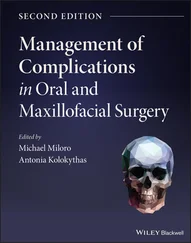
Похожие книги на «Shear's Cysts of the Oral and Maxillofacial Regions»
Представляем Вашему вниманию похожие книги на «Shear's Cysts of the Oral and Maxillofacial Regions» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Shear's Cysts of the Oral and Maxillofacial Regions» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.