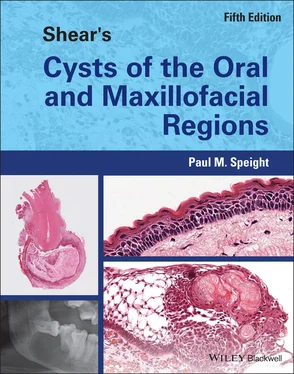
Paul M. Speight - Shear's Cysts of the Oral and Maxillofacial Regions
Здесь есть возможность читать онлайн «Paul M. Speight - Shear's Cysts of the Oral and Maxillofacial Regions» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Shear's Cysts of the Oral and Maxillofacial Regions
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:5 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 100
- 1
- 2
- 3
- 4
- 5
Shear's Cysts of the Oral and Maxillofacial Regions: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Shear's Cysts of the Oral and Maxillofacial Regions»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Shear’s Cysts of the Oral and Maxillofacial Regions
Shear’s Cysts of the Oral and Maxillofacial Regions Fifth Edition
Shear's Cysts of the Oral and Maxillofacial Regions — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Shear's Cysts of the Oral and Maxillofacial Regions», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
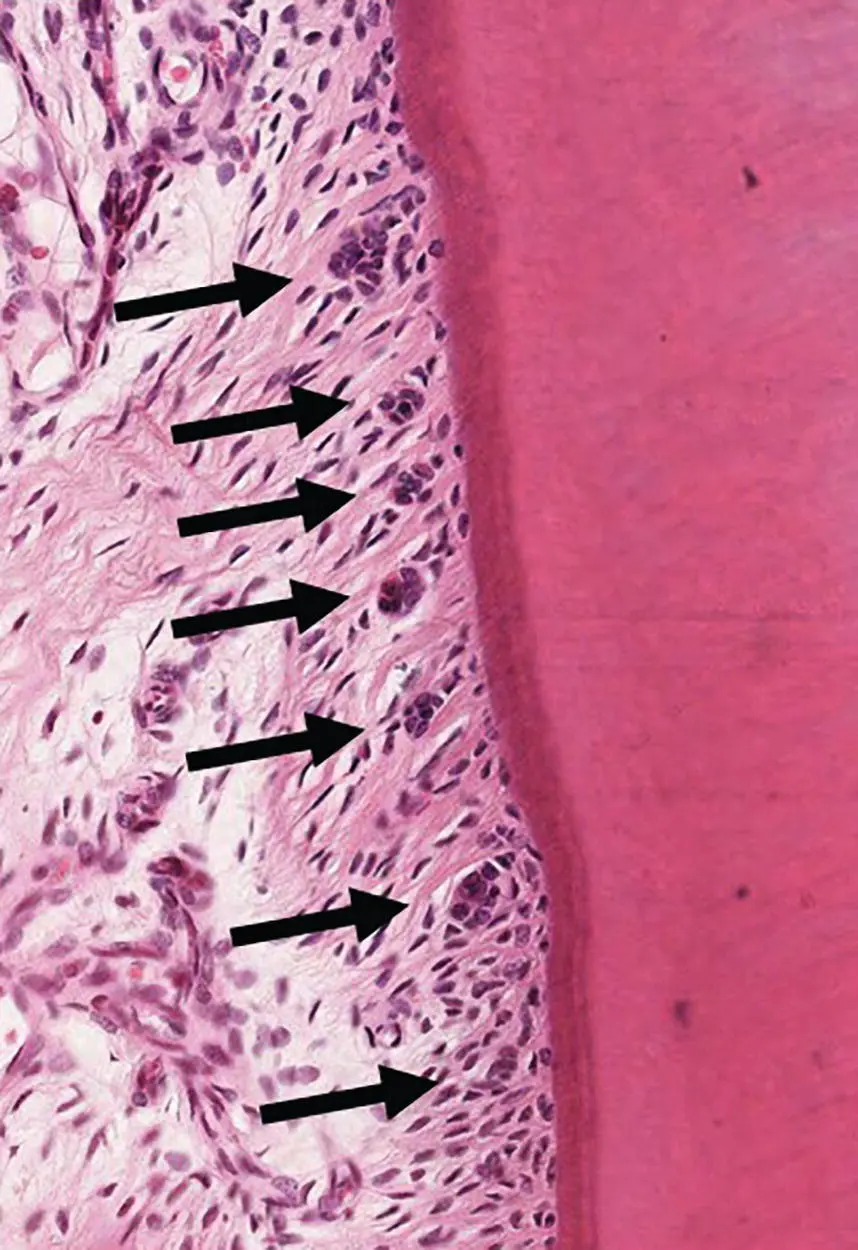
Figure 3.6 Rest cells of Malassez appear as multiple small islands of epithelium (arrows) within the periodontal ligament.
There is no doubt that the start of the process of cyst formation involves the proliferation of the epithelial cell rests within the inflamed tissues of a periapical granuloma. As discussed previously, LPS is the key factor that initiates the inflammatory and immune response, but it may also directly cause epithelial proliferation. In their study of fluids and explants from radicular cysts, keratocysts, and follicular cysts, Meghji et al. (1996 ) showed high levels of LPS in radicular cysts and demonstrated that it could directly stimulate epithelial proliferation in a dose‐dependent manner. They proposed that bacterial LPS, derived from the necrotic pulp, is the key initiating factor in the pathogenesis of radicular cysts. In this same study they also provided evidence that cytokines can directly stimulate epithelial proliferation. All cysts contained IL‐1α and IL‐6, but radicular cyst explants produced significantly more IL‐6 than either keratocysts or follicular cysts. Further experiments showed that IL‐1 and IL‐6, and culture supernatants from cyst fibroblasts, were able to stimulate epithelial proliferation in a dose‐dependent manner. Significantly, this activity was further enhanced by the addition of LPS.
In earlier experiments, the same research group (Meghji et al. 1989 ; Bando et al. 1993 ) used immunocytochemistry to localise cytokines and adhesion molecules in the walls of radicular cysts. All cysts showed positive staining for IL‐1α, IL‐1β, and IL‐6 in the epithelial lining and in vascular endothelial cells. Tumour necrosis factor (TNF) and CXCL8/IL‐8 were occasionally seen in macrophages. The cell adhesion molecules ICAM‐1 and ELAM‐1 (E‐selectin) were also identified in all lesions and were localised to endothelial cells, epithelium, and inflammatory cells.
Kusumi et al. (2004 ) produced further evidence that IL‐6 has an important role. They used reverse transcriptase polymerase chain reaction (RT‐PCR) to study a number of cytokines in tissues from 19 radicular cysts and compared expression with normal gingivae and periodontal ligament. They found variable expression of cytokines in all tissues, but most cysts expressed IL‐1β, IL‐6, CXCL8/IL‐8, TNF‐α, interferon (IFN)‐γ, and TGF‐β1, and most of these showed increased expression compared with normal tissues. All the cytokines were expressed at low levels except for IL‐6, which showed high levels of secretion from fibroblasts extracted from the radicular cysts.
These studies confirmed that the walls and epithelial lining of radicular cysts synthesise a range of cytokines and growth factors that are known to be involved in epithelial proliferation ( Table 3.2).
The role of abscess formation in the formation of a cyst will be discussed below, but there is good evidence that an acute inflammatory cell infiltration may be directly associated with epithelial proliferation, since many early studies were able to demonstrate large numbers of PMNs in the proliferating epithelium (Shear 1963a , 1964 ; Cohen 1979 ; Johannessen 1986 ). As mentioned above, LPS from the root canal stimulates CXCL8/IL‐8 secretion from periodontal fibroblasts via the co‐receptors CD14 and Toll‐like receptor (mainly TLR4). In addition, epithelial cells in periapical lesions have been shown to express CD14/TLR4 (Leonardi et al. 2015 ), and there is evidence that CXCL8/IL‐8 may directly cause epithelial proliferation as well as being a chemoattractant for PMNs (Silva et al. 2007 ; Marton and Kiss 2014 ). This would explain the association of proliferating epithelium and PMNs in early lesions.
Phase of Cyst Formation
The next phase in the pathogenesis of a radicular cyst is the process by which a cavity comes to be lined by the proliferating odontogenic epithelium. Many will think it astonishing that the actual process of cyst formation is so poorly understood, and although a number of theories have been debated for decades, there are very few observational or experimental data to support or refute any of them. There are three proposed mechanisms of cyst formation (Shear 1963a ; Summers 1974 ; Valderhaug 1974 ; Lin et al. 2007 ; Nair et al. 2008 ; Huang 2010 ):
1 Central necrosis or nutritional deficiency theory. This proposes that a cyst cavity forms within a proliferating mass of epithelial cells due to loss of nutrition followed by degeneration and death of cells in the centre of the mass.
2 Abscess theory. This postulates that the proliferating epithelium surrounds an abscess cavity, in effect walling off the central focus of inflammation. Essentially this represents the process of normal wound healing, where epithelium proliferates to cover denuded connective tissues.
3 Merging epithelial strands theory. This proposes that the proliferating epithelium forms a three‐dimensional ‘ball mass’ (Lin et al. 2007 ), which entraps inflamed connective tissue. This connective tissue then breaks down due to loss of a blood supply and a cyst cavity forms.
Proponents of each process often promote their favoured theory, while suggesting that others are not tenable (Lin et al. 2007 ; Nair et al. 2008 ; Huang 2010 ), but in fact they are not mutually exclusive and all three have a similar premise – that epithelium proliferates to surround and encase a focus of inflamed and degenerating or necrotic tissue. There is little difference, for example, between an abscess (theory 2) and necrotic connective tissue (theory 3), apart perhaps from the degree or stage of necrosis and the types of cells present. Similarly, the necrotic centre of an epithelial mass (theory 1) may contain PMNs and essentially become an abscess, a feature familiar to tumour pathologists in the form of comedo necrosis. Thus on histological examination, the presence of an abscess cavity lined by epithelium may support theory 1 or 2. Also, in the previous edition of this book we showed a photomicrograph ( Figure 3.7) of arcading epithelium surrounding inflamed connective tissue in support of theory 1 – but in fact this pattern of proliferating epithelium, with entrapment of connective tissue, is very similar to the merging epithelial strands theory of Lin et al. (2007 ) (theory 3).
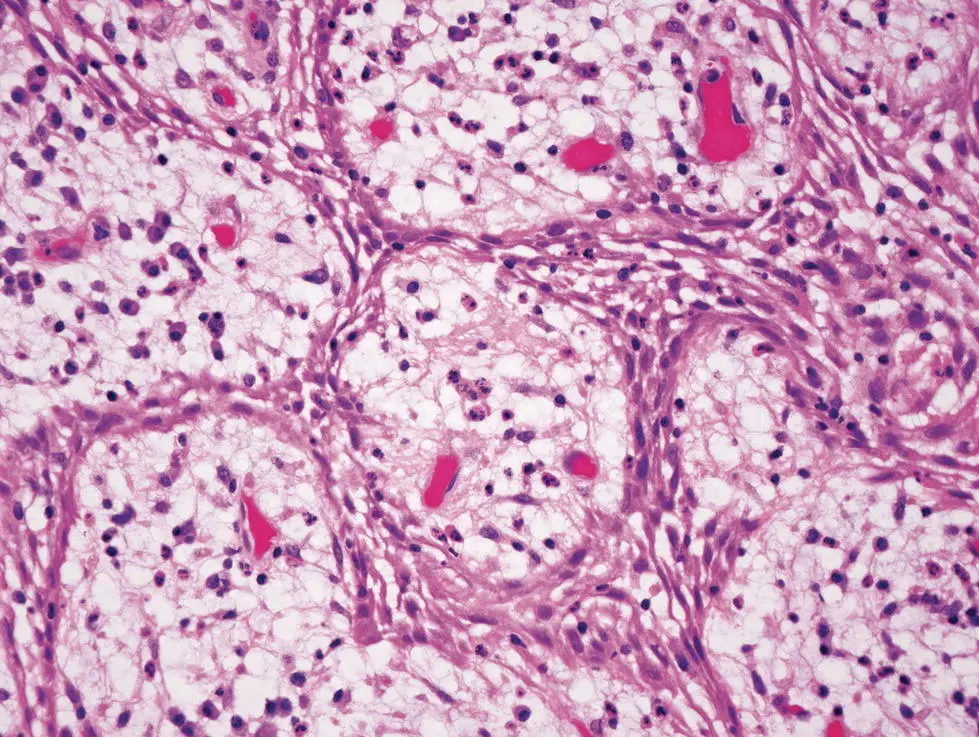
Figure 3.7 Arcades and rings of proliferating epithelium in a periapical granuloma. The epithelium surrounds islands of inflamed connective tissue that may break down to initiate early cyst formation.
In support of theory 1, there is some histological evidence for central necrosis or nutritional deficiency. In some periapical lesions, distinct clefts may be seen in sheets of epithelial cells (Shear 1963a ) ( Figure 3.8), and the proliferating epithelial masses often show considerable intercellular oedema. These intercellular accumulations of fluid coalesce to form microcysts containing epithelial and inflammatory cells, including PMNs ( Figure 3.9). These central areas have been shown to contain high levels of acid phosphatase activity and proteolytic enzymes consistent with autolysis or necrosis (Lutz et al. 1965 ; Summers 1972 , 1974 ). Microcysts may increase in size by coalescence with adjacent microcysts and, once established, the cyst increases in size by mechanisms that are discussed later.
Most information regarding cyst formation is taken from histological observation of biopsy specimens taken from humans and there are very few longitudinal studies. In experiments that have not been repeated, Valderhaug (1972 ) induced radicular cysts in monkeys. Because of the rarity of such experiments, it is worth considering some of the details of his findings. He induced pulpal necrosis sequentially in 39 teeth in 4 animals and was able to histologically examine periapical inflammation and cyst formation for up to 360 days after the pulps were removed. Of interest is that he did not observe any cysts until after 200 days, although proliferating epithelium was observed in earlier lesions. In lesions examined after 200 days, 11 of 16 (69%) developed cysts. Even after 300 days, 3 of 8 lesions showed no inflammation, but 4 had developed into cysts. Of relevance to the proposed mechanisms of cyst formation is that he did not see evidence of intraepithelial degeneration with formation of microcysts, but observed long strands of proliferating epithelium lining surfaces of granulation tissue, or arcades surrounding cores of vascularised or degenerating granulation tissue. These observations support the merging epithelial strands theory (theory 3). However, in most cases Valderhaug also observed that the proliferating epithelium was associated with PMNs, but he did not describe frank abscess formation. He also showed that in most cysts the epithelial lining was closely connected to the roots around the apical foramen, supporting the notion that the epithelium is reforming an intact integument, and that the cysts are pocket or bay cysts. In a very similar study, Valderhaug (1974 ) examined 52 primary teeth, and although periapical inflammation was common, he found small cysts only in ‘a few cases with long observation periods’. Of relevance to the theories of cyst formation is that he found that abscess formation, often with oral fistulas, was common and more frequently seen than in his previous study on permanent teeth (Valderhaug 1972 ). His findings, however, did not support the abscess theory, since ‘proliferating epithelium was not observed in the periapical area in connection with abscess formation’.
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Shear's Cysts of the Oral and Maxillofacial Regions»
Представляем Вашему вниманию похожие книги на «Shear's Cysts of the Oral and Maxillofacial Regions» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Shear's Cysts of the Oral and Maxillofacial Regions» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.