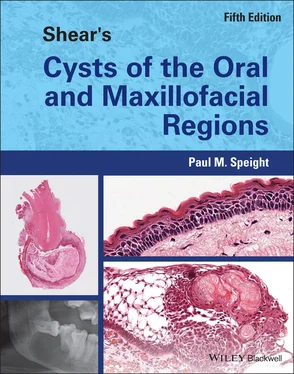
Paul M. Speight - Shear's Cysts of the Oral and Maxillofacial Regions
Здесь есть возможность читать онлайн «Paul M. Speight - Shear's Cysts of the Oral and Maxillofacial Regions» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Shear's Cysts of the Oral and Maxillofacial Regions
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:5 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 100
- 1
- 2
- 3
- 4
- 5
Shear's Cysts of the Oral and Maxillofacial Regions: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Shear's Cysts of the Oral and Maxillofacial Regions»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Shear’s Cysts of the Oral and Maxillofacial Regions
Shear’s Cysts of the Oral and Maxillofacial Regions Fifth Edition
Shear's Cysts of the Oral and Maxillofacial Regions — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Shear's Cysts of the Oral and Maxillofacial Regions», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
The proportion of B lymphocytes has been reported to be about 20% (Kontiainen et al. 1986 ), with plasma cells varying from 2% (Kontiainen et al. 1986 ) to 13% (Stern et al. 1982 ). As would be expected, the vast majority (over 75%) of plasma cells express immunoglobulin (Ig)G, with 15–20% IgA and very few IgE or IgM (Stern et al. 1981 ; Smith et al. 1987 ). Other cell types that play a role in periapical lesions include macrophages, mast cells, and Langerhans cells (Pulver et al. 1978 ; Kontiainen et al. 1986 ; Drazic et al. 2010 ). Langerhans cells may be of particular interest because they have been found in the epithelial linings of radicular cysts (Contos et al. 1987 ; Matthews and Browne 1987 ; Gao et al. 1988a ; Liapatas et al. 2003 ) and are most prominent in areas of heavy inflammation. Although they are known to be important in antigen presentation, it has been suggested that they may also be associated with epithelial proliferation (Carillo et al. 2010 ). Non‐immune cells, including fibroblasts, endothelial cells, and epithelial cells, are also present and may be involved in producing relevant cytokines and growth factors. Lesions also contain PMNs and primary or secondary abscess formation may be a key factor in cyst formation (see later in this chapter).
Although the main initiating factor of a periapical lesion is bacterial LPS, the lesions are then sustained by a complex network of inflammatory mediators, including cytokines, chemokines, and the eicosanoids (mainly prostaglandins). These have multiple roles in cell activation and migration, in epithelial proliferation, and in bone resorption. In early lesions there is good evidence that the chemokine CXCL8/IL‐8 is important since it is absent in normal pulp, but found in about 95% of periapical lesions. LPS stimulates periodontal ligament fibroblasts to secrete CXCL8/IL‐8, which has a pivotal role in PMN migration and therefore in lesion initiation (reviewed in Silva et al. 2007 ; Graunaite et al. 2012 ; Marton and Kiss 2014 ). This chemokine is also important in bone resorption. Other pivotal cytokines are the interleukins, especially IL‐1 and IL‐6, which have roles in activating PMNs and lymphocytes, and in bone resorption (reviewed in Graunaite et al. 2012 ). Table 3.2lists a number of selected biological factors that may be involved in the pathogenesis of radicular cysts. Mostly this list is derived from the reviews mentioned previously (Bernardini et al. 2015 ; Marton and Kiss 2014 ; Graunaite et al. 2012 ; Graves et al. 2011 ; Silva et al. 2007 ; Lin et al. 2007 ; Nair 2004 ). The actions of those factors thought to have important or specific roles in the formation of radicular cysts are discussed in the sections that follow.
Phase of Initiation
It is generally agreed that the source of epithelium for a radicular cyst is the epithelial cell rests of Malassez. During tooth development the epithelial root sheath of Hertwig maps out the shape of the roots and initiates dentine formation. When tooth formation is complete, the sheath disintegrates and epithelial remnants remain in the periodontal ligament as the rest cells of Malassez. There are two common misconceptions about these cells: first, that they are small islands; and second, that they have no normal function. It is now clear that the epithelial remnants form a network or mesh that lies in the periodontal ligament and surrounds or embraces the tooth root. Only in histological sections do they appear to be isolated islands ( Figure 3.6). It is now also apparent that the cell rests of Malassez have a number of important functions in normal periodontal homeostasis, including cementogenesis, healing and regeneration (Keinan and Cohen 2013 ; Xiong et al. 2013 ). They are thus important in maintaining periodontal health during all the normal challenges of tooth movement and function as well as in responses to trauma, orthodontic tooth movement, and periodontitis. These properties are being exploited in the development of therapeutic approaches to promote periodontal regeneration in the management of periodontal diseases (Xiong et al. 2013 ).
Table 3.2 Biological factors that have a role in the pathogenesis of radicular cyst.
| Factors | Cell(s) of origin | Target cell (ligand(s)) | Key function |
|---|---|---|---|
| Bacterial factors | |||
| LPS (endotoxin) | Bacteria | Fibroblasts and many cell types (CD14/TLR) | Induces a wide range of mediators, including CXCL8/IL‐8, TNF‐α, IL‐1, RANKL, OPG. Indirectly stimulates bone resorption |
| Cytokines | |||
| IL‐1α | Macrophages, PMN, osteoclasts, epithelial cells, dendritic cells | Attracts and activates PMNs; stimulates production of prostaglandins, proteolytic enzymes, cytokines IL‐6, IL‐8; stimulates bone resorption and inhibits bone formation (originally called osteoclast‐activating factor, OAF) | |
| IL‐1β | Macrophages | Monocytes | Inhibits osteoclast formation and bone resorption |
| IL‐6 | Macrophages, epithelial cells, PMN, Th2 cells, B lymphocytes, endothelial cells, fibroblasts | Activates and stimulates PMNs and T cells; stimulates differentiation of B lymphocytes into plasma cells; stimulates osteoclasts and bone resorption; down‐regulates production of IL‐1 | |
| TNF‐α | Macrophages, Th1 cells, PMN, fibroblasts | Activates lymphocytes and macrophages; stimulates bone resorption | |
| IL‐17 | Th17 | Up‐regulates secretion of IL‐1, IL‐6, TNF‐α, and IL‐8 secretion; attracts PMNs; stimulates osteoclasts and bone resorption | |
| GM‐CSF | Macrophages, T lymphocytes, endothelial cells, PMN | Functionally activates macrophages and PMNs | |
| TGF‐β | Lymphocytes (Treg), macrophages, fibroblasts, osteoblasts, osteoclasts, epithelial cells | PMNs, macrophages | Anti‐inflammatory; suppresses T and B lymphocytes; down‐regulates production of IL‐1, IL‐6, TNF‐α, and IFN‐γ; blocks production of nitric oxide by macrophages; inhibits bone resorption; inhibits Th17 and promotes Treg formation |
| IFN‐γ | Th1 cells, dendritic cells | Th lymphocytes | Activates macrophages; induces IL‐1 production; inhibits RANKL and bone resorption |
| IL‐12 | Th1 cells, macrophages, dendritic cells | Up‐regulates IL‐1 and IFN‐γ; stimulates Th1 differentiation; suppresses Th2 differentiation | |
| IL‐10 | Macrophages, dendritic cells, lymphocytes (Treg) | Anti‐inflammatory; down‐regulates IL‐1 and IFN‐γ; inhibits action of RANKL and bone resorption | |
| IL‐4 | Th2 cells | Inhibits bone resorption; inhibits Th17 formation; down‐regulates IL‐1 | |
| RANKL | Normally present on osteoblasts; also Th1cells, endothelial cells, fibroblasts, PMNs, epithelial cells; may be soluble | Osteoclasts and precursors (RANK) | Activates osteoclasts; positively regulates bone resorption |
| OPG | Osteoblasts, some epithelial cells, endothelial cells, B cells | Osteoblasts (RANKL) | Decoy receptor for RANKL and blocks RANK/RANKL pathway; inhibits osteoclastogenesis and negatively regulates bone resorption |
| Chemokines | |||
| CXCL8 (IL‐8) | Macrophages, PMN, Th1 cells, Th17 cells | CXCR1‐2 | Attracts PMNs and macrophages; chemotaxis and differentiation of osteoclasts |
| CXCL12 (SDF‐1α) | Endothelial cells | Osteoclast precursors (CXCR4); PMNs | Chemotaxis and differentiation of osteoclasts; attracts PMNs; up‐regulates MMPs |
| CCL7 (MCP‐3) | Endothelial cells, lymphocytes, fibroblasts, plasma cells | Osteoclasts and precursors | Chemotaxis and differentiation of osteoclasts |
| CCL5 (RANTES) | T cells, fibroblasts, osteoclasts, osteoblasts | Osteoclasts and precursors (CCR1, CCR5) | Chemotaxis and differentiation of osteoclasts |
| CCL‐2 (MCP‐1) | Osteoblasts | Osteoclasts and precursors (CCR2) | Chemotaxis and differentiation of osteoclasts |
| CCL3 (MIP‐1α) | Fibroblasts, osteoclasts, osteoblasts | Macrophages (CCR1), lymphocytes/Th1 (CCR5) | Chemotaxis and differentiation of osteoclasts; attracts macrophages |
| CCL4 (MIP‐1β) | Th1 cells | Chemotaxis and differentiation of osteoclasts; activates macrophages | |
| Prostaglandins | |||
| Prostaglandins (PGE 2) | Macrophages, fibroblasts, inflammatory cells, epithelial cells, endothelial cells | Osteoclasts (receptors EP 1–EP 4) | Stimulates osteoclasts and bone resorption |
GM‐CSF, granulocyte‐macrophage colony‐stimulating factor; IFN, interferon; IL, interleukin; LPS, lipopolysaccharides; MCP, monocyte chemoattractant protein; MIP, macrophage inflammatory protein; MMP, matrix metalloproteinase; OPG, osteoprotegerin; PMN, polymorphonuclear leukocyte; RANK, receptor activator of nuclear factor kappa B; RANKL, receptor activator of nuclear factor kappa B ligand; RANTES, regulated upon activation, normal T cell expressed and presumably secreted; SDF, stromal cell‐derived factor; TGF, transforming growth factor; TLR, Toll‐like receptor; TNF, tumour necrosis factor; Treg, regulatory T cell.
Читать дальшеИнтервал:
Закладка:
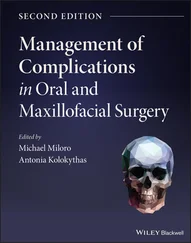
Похожие книги на «Shear's Cysts of the Oral and Maxillofacial Regions»
Представляем Вашему вниманию похожие книги на «Shear's Cysts of the Oral and Maxillofacial Regions» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Shear's Cysts of the Oral and Maxillofacial Regions» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.