12 12 Giadinis ND, Psychas V, Polizopoulou Z, et al. Acute coenurosis of dairy sheep from 11 flocks in Greece. N Z Vet J 2012; 60(4): 247–253.
13 13 Ozmen O and Mor F. Acute lead intoxication in cattle housed in an old battery factory. Vet Hum Toxicol 2004; 46(5): 255–256.
14 14 Johnson PJ, Mrad DR, Schwartz AJ and Kellam L. Presumed moxidectin toxicosis in three foals. J Am Vet Med Assoc 1999; 214(5): 678–680.
15 15 Brownlow MA, Dart AJ and Jeffcott LB. Exertional heat illness: a review of the syndrome affecting racing Thoroughbreds in hot and humid climates. Aust Vet J 2016; 94(7): 240–247.
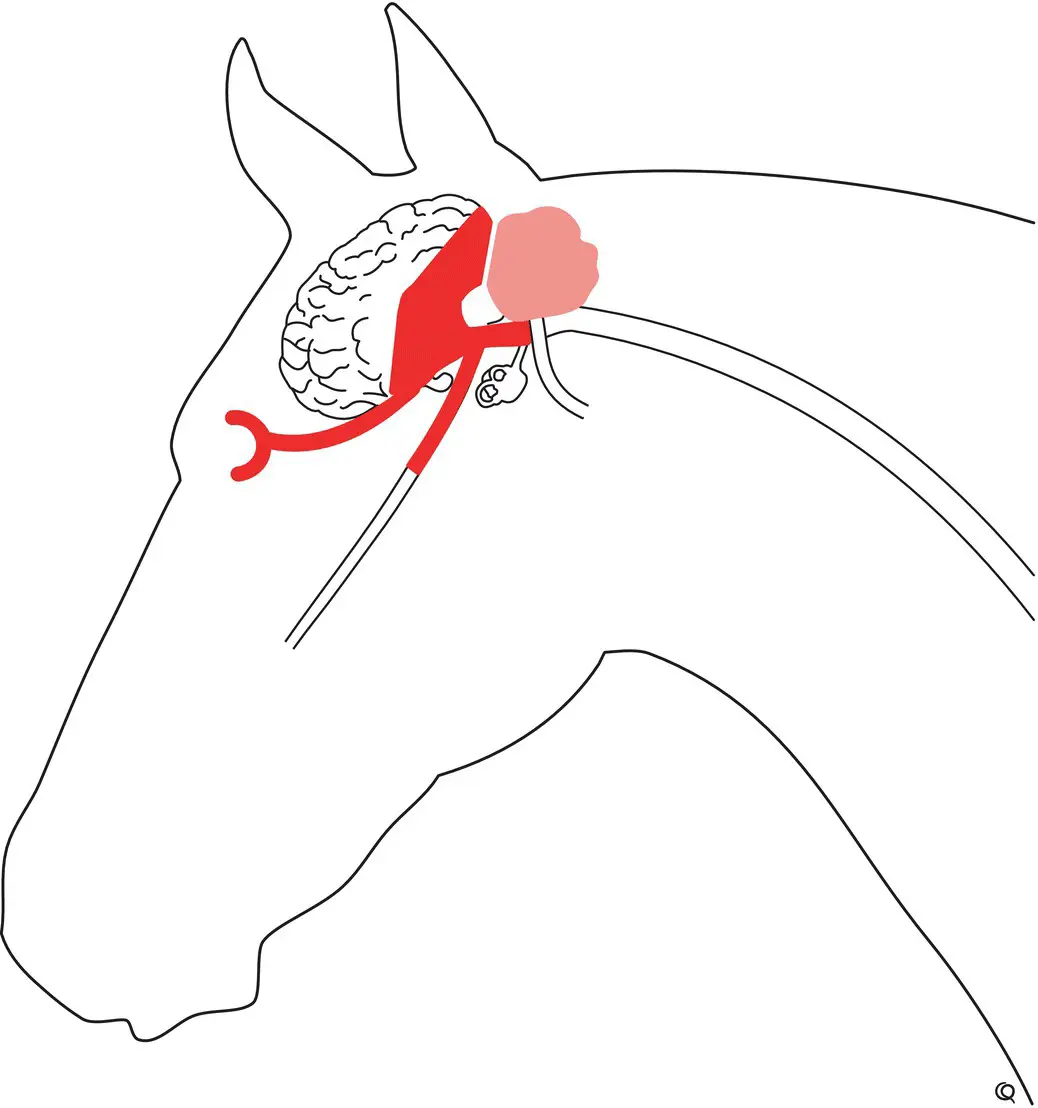
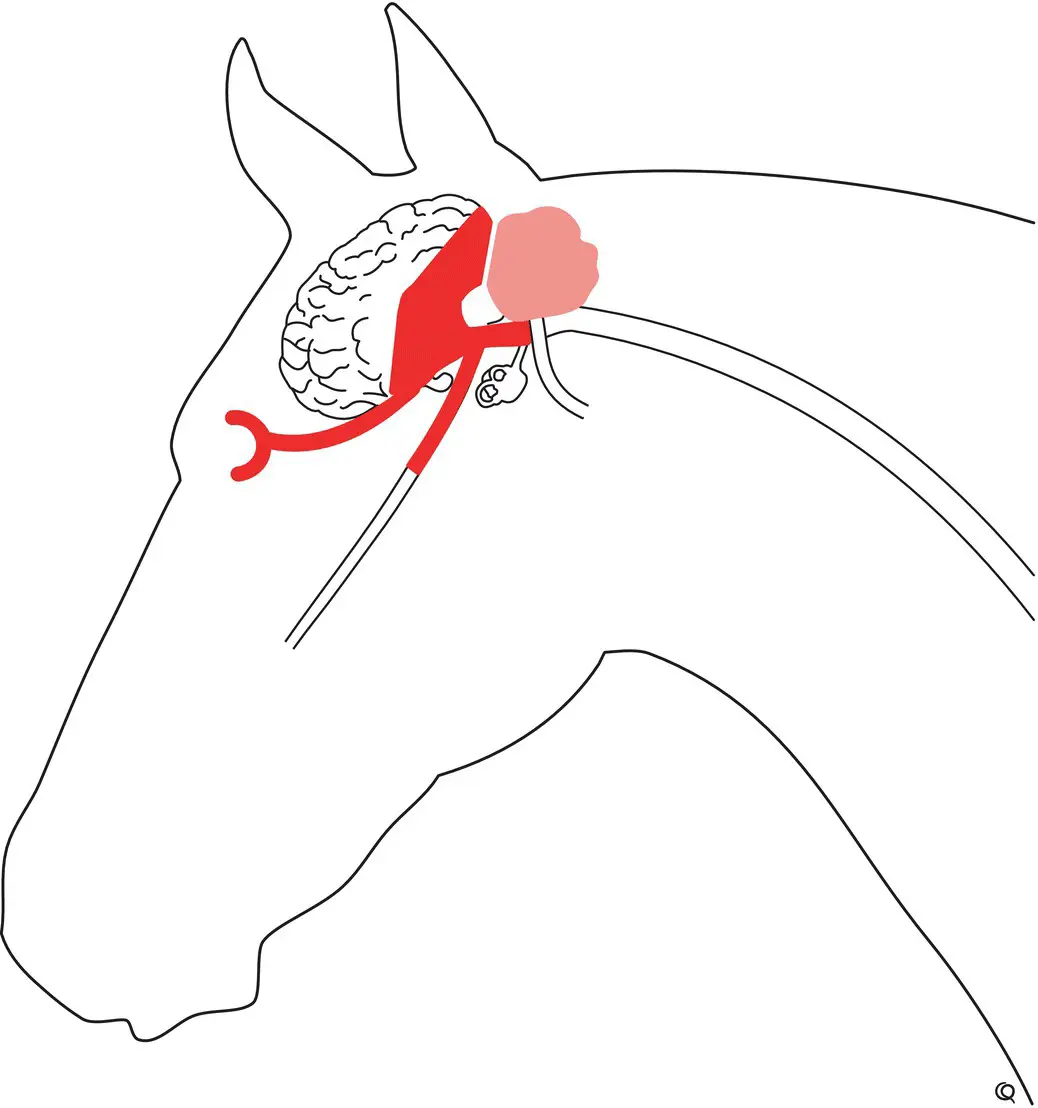
The visual and pupillary light pathways should be reviewed ( Figure 2.9) as well as the discussion on testing for vision in the neurologic examination section in Chapter 2. Some cases of reduced vision with the associated pupillary changes are given here as examples of blindness in large animals ( Figure 9.1).
Often animals suffering from forebrain lesions are blind with depressed menace responses in one or both eyes. A central blindness or amaurosis, with pupillary reflexes intact, occurs in an eye contralateral to a lesion involving an optic tract, dorsal thalamus (lateral geniculate nucleus), optic radiation part of the internal capsule, or the visual cortex predominantly in the occipital lobe of the cerebral hemisphere. These structures constitute the central visual pathways. Central to the chiasma, one optic tract receives circa >80% of all visual and light pathway fibers from the contralateral eye, and these functionally different fibers pass together in the first portion of the optic tract to the level of the caudal thalamus where the pupillary light fibers separate to synapse on the pretectal nucleus and thence to the parasympathetic oculomotor nucleus in the midbrain ( Figure 2.7). Thus, one would expect that, as well as central contralateral blindness due to a lesion involving the (light and visual) afferent, immediate postchiasmal optic tract fibers, there should be (bilaterally) suppressed pupillary motor function evident when light is shone in the blind eye. However, clinically this is very difficult to discern. On the other hand, occasionally it is possible to detect visual field deficits with some selective and focal lesions involving these central visual pathways as discussed in the neurologic examination section in Chapter 2.
A lesion in the eye or optic nerve on one side, with the other eye and its optic system normal, results in blindness and a suppressed menace response in that eye with slightly dilated pupils (mydriasis) and poor pupillary constriction in both eyes when light is shone in the blind eye. The degree of mydriasis evident will depend on the ambient light that the other normal eye is exposed to. A patient can be clinically blind with an absent menace response and a slightly dilated pupil in one eye due to an eye or optic nerve lesion, and can still have some pupillary constriction in response to a very bright strobe light shone in that eye. This discrepancy comes down to difficulties in determining when an animal is totally blind, and the fact that visual path fibers are probably damaged more readily with various eyeball and optic nerve lesions than are light pathway fibers destined for the oculomotor nuclei in the midbrain. With respect to visual perception, possibly the most sensitive test of crude visual pathway input is to place a blind patient having no menace responses in a dark enclosed area with a brightly lighted exit available to see if the patient can discern the escape route.

Figure 9.1 Following head trauma, bilateral blindness with dilated and nonresponsive pupils in a fully conscious horse as in top figure, is most likely due to bilateral optic nerve injury. In comparison, blindness with a normally responsive pupil, as in bottom figure, is more likely due to a contralateral, central, thalamic, or caudal cerebral lesion.
The swinging light test can be useful to help sort out difficult visual deficits too, as performing and interpreting consensual or indirect pupillary light reflexes in large animals is problematic, particularly with partial lesions, and often having to perform the examination in daylight without access to a darkened environment (see case example in Chapter 10).
It is often good to recall that even partial sunlight is brighter than any commonly used, handheld penlight or ophthalmoscope.
Here, it must be recalled that blinking in response to a bright light, the dazzle response, does not involve the visual pathways from the thalamus to the visual cortex, and the presence of this response does not equate with intact vision. Its presence does indicate that light is stimulating the light pathways into the midbrain and thence to the facial nucleus, but it should not replace testing the true pupillary light and menace responses as outlined. Thus, it is conceivable that a dazzle response can be present in a centrally blind patient that also has no oculomotor nerve function and therefore no pupillary light reflexes, a very unlikely clinicopathologic scenario.
The prognosis for acquired peripheral blindness is bad compared to that for central visual pathway lesions. Apart from eye diseases, most common causes of only peripheral blindness would be head trauma, 1,2sphenopalatine sinus infection and neoplasia, 3progressive ethmoid hematoma, and various anthelmintic toxicities. 4–7In comparison, the prognosis for partial central blindness is better as such patients are able to compensate well and at times to regain quite amazing degrees of apparent visual acuity.
The postictal period may be associated with temporary central blindness presumably due to neuronal exhaustion in central visual pathways. Also neonates, although they can see, have poor menace responses in the first 1 or 2 weeks of life. 8
Finally, degrees of blindness occur with many ocular diseases. Of some note is that with cases of congenital peripheral blindness, there can be associated abnormal eyeball positions, with the globe directed dorsally and sometimes wavering, searching eyeball movements. Removal of obstacles and provision of a “buddy” that wears a bell are some of the provisions that assist in caring for a blind horse. 9,10The reader is referred to texts of ophthalmology and particularly to chapters on neuro‐ophthalmology in large animals. 911–18
1 1 Matz K, Gerhards H, Heider HJ and Drommer W. Bilateral blindness after injury in a riding horse. Tierarztl Prax 1993; 21(3): 225–232.
2 2 Reppas GP, Hodgson DR, McClintock SA and Hartley WJ. Trauma‐induced blindness in two horses. Aust Vet J 1995; 72(7): 270–272.
3 3 Sano Y, Okamoto M, Ootsuka Y, et al. Blindness associated with nasal/paranasal lymphoma in a stallion. J Vet Med Sci 2017; 79(3): 579–583.
4 4 Button C, Jerrett I, Alexander P and Mizon W. Blindness in kids associated with overdosage of closantel. Aust Vet J 1987; 64(7): 226.
5 5 Barlow AM, Sharpe JA and Kincaid EA. Blindness in lambs due to inadvertent closantel overdose. Vet Rec 2002; 151(1): 25–26.
6 6 Borges AS, Mendes LC, de Andrade AL, Machado GF and Peiro JR. Optic neuropathy in sheep associated with overdosage of closantel. Vet Hum Toxicol 1999; 41(6): 378–380.
7 7 Pollio D, Michau TM, Weaver E and Kuebelbeck KL. Electroretinographic changes after intravenous lipid emulsion therapy in a dog and a foal with ivermectin toxicosis. Vet Ophthalmol 2018; 21(1): 82–87.
Читать дальше