Irene Roberts - Neonatal Haematology
Здесь есть возможность читать онлайн «Irene Roberts - Neonatal Haematology» — ознакомительный отрывок электронной книги совершенно бесплатно, а после прочтения отрывка купить полную версию. В некоторых случаях можно слушать аудио, скачать через торрент в формате fb2 и присутствует краткое содержание. Жанр: unrecognised, на английском языке. Описание произведения, (предисловие) а так же отзывы посетителей доступны на портале библиотеки ЛибКат.
- Название:Neonatal Haematology
- Автор:
- Жанр:
- Год:неизвестен
- ISBN:нет данных
- Рейтинг книги:4 / 5. Голосов: 1
-
Избранное:Добавить в избранное
- Отзывы:
-
Ваша оценка:
- 80
- 1
- 2
- 3
- 4
- 5
Neonatal Haematology: краткое содержание, описание и аннотация
Предлагаем к чтению аннотацию, описание, краткое содержание или предисловие (зависит от того, что написал сам автор книги «Neonatal Haematology»). Если вы не нашли необходимую информацию о книге — напишите в комментариях, мы постараемся отыскать её.
Neonatal Haematology — читать онлайн ознакомительный отрывок
Ниже представлен текст книги, разбитый по страницам. Система сохранения места последней прочитанной страницы, позволяет с удобством читать онлайн бесплатно книгу «Neonatal Haematology», без необходимости каждый раз заново искать на чём Вы остановились. Поставьте закладку, и сможете в любой момент перейти на страницу, на которой закончили чтение.
Интервал:
Закладка:
Irene Roberts
Abbreviations
2,3‐DPG2,3‐diphosphoglycerateADAadenosine deaminaseADPadenosine diphosphateAGMaorto‐gonado‐mesonephrosaHUSatypical haemolytic uraemic syndromeAIHAautoimmune haemolytic anaemiaALLacute lymphoblastic leukaemiaALPSautoimmune lymphoproliferative syndromeAMLacute myeloid leukaemiaAPTTactivated partial thromboplastin timeATDasphyxiating thoracic dystrophyATRUSamegakaryocytic thrombocytopenia and radio‐ulnar synostosisBCGbacille Calmette–GuérinBCSHBritish Committee for Standards in HaematologyBHFSBart's hydrops fetalis syndromeBPIbactericidal/permeability‐increasing proteinBSSBernard–Soulier syndromeCAMTcongenital amegakaryocytic thrombocytopeniaCDAcongenital dyserythropoietic anaemiaCHSChédiak–Higashi syndromeCMVcytomegalovirusCNScentral nervous systemCOVID‐19coronavirus disease 19DATdirect antiglobulin testDBADiamond–Blackfan anaemiaDICdisseminated intravascular coagulationDNAdeoxyribonucleic acidECMOextracorporeal membrane oxygenationEDTAethylene diaminetetra‐acetic acidELPearly lymphoid progenitorEMAeosin‐5‐maleimideEOSearly‐onset sepsisEPOerythropoietinERFEerythroferroneFFPfresh frozen plasmaFNAITfetal/neonatal alloimmune thrombocytopeniaFPD/AMLfamilial platelet disorder with propensity to acute myeloid leukaemiaFRCfragmented red cellG6PDglucose‐6‐phosphate dehydrogenaseG6PT1glucose‐6‐phosphate transporter 1G‐CSFgranulocyte colony‐stimulating factorGpglycoproteinGPIglucose phosphate isomeraseHbhaemoglobin concentrationHDFNhaemolytic disease of the fetus and newbornHELLPhaemolysis, elevated liver enzymes and low plateletsHIEhypoxic ischaemic encephalopathyHIVhuman immunodeficiency virusHKhexokinaseHLHhaemophagocytic lymphohistiocytosisHNAhuman neutrophil antigenHPAhuman platelet antigenHPFHhereditary persistence of fetal haemoglobinHPLChigh performance liquid chromatographyHPPhereditary pyropoikilocytosisHShereditary spherocytosisHSChaemopoietic stem cellHUShaemolytic uraemic syndromeIBMFSinherited bone marrow failure syndromesICHintracranial haemorrhageIG%immature granulocyte percentageIGFinsulin‐like growth factorIgGimmunoglobulin GIgHimmunoglobulin heavy chainIgMimmunoglobulin MIL‐6interleukin‐6IPFimmature platelet fractionIRFinterferon regulatory factorITPautoimmune thrombocytopeniaIUGRintrauterine growth restrictionIUTintrauterine transfusionIVHintraventricular haemorrhageIVIgintravenous immunoglobulinJAK2Janus kinase 2JMMLjuvenile myelomonocytic leukaemiaKHEKaposiform haemangioendotheliomaKMPKasabach–Merritt phenomenonLADleucocyte adhesion deficiencyLDHlactate dehydrogenaseLOSlate‐onset sepsisMAHAmicroangiopathic haemolytic anaemiaMAIPAmonoclonal antibody‐specific immobilisation of platelet antigensMCAmiddle cerebral arteryMCHmean cell haemoglobinMCHCmean cell haemoglobin concentrationMCVmean cell volumeMDSCmyeloid‐derived suppressor cellML‐DSmyeloid leukaemia of Down syndromeMPALmixed phenotype acute leukaemiaMPVmean platelet volumeNAnot applicableNADPHnicotinamide adenine dinucleotide phosphateNECnecrotising enterocolitisNETsneutrophil extracellular trapsNICENational Institute for Health and Care ExcellenceNICUneonatal intensive care unitNLRneonatal leukaemoid reactionNRBCnucleated red blood cellNS/MPDNoonan syndrome‐associated myeloproliferative disorderPCCprothrombin complex concentratePCRpolymerase chain reactionPFKphosphofructokinasePGKphosphoglycerate kinasePKpyruvate kinasePMNpolymorphonuclearPTprothrombin timeRNAribonucleic acidRPribosomal proteinsRSVrespiratory syncytial virusRUSAT1radio‐ulnar synostosis with amegakaryocytic thrombocytopeniaSARS‐CoV‐2severe acute respiratory syndrome coronavirus‐2SCNsevere congenital neutropeniaSGAsmall for gestational ageSIFDsideroblastic anaemia, B‐cell immunodeficiency, periodic fevers, and developmental delaySLEsystemic lupus erythematosusTACOtransfusion‐associated circulatory overloadTA‐GvHDtransfusion‐associated graft‐versus‐host diseaseTAMtransient abnormal myelopoiesisTAPStwin anaemia–polycythaemia sequenceTARthrombocytopenia with absent radiiTGFβtransforming growth factor βTOPsTransfusion of Prematures trialTPItriosephosphate isomeraseTPOthrombopoietinTRALItransfusion‐related acute lung injuryTTthrombin timeTTPthrombotic thrombocytopenic purpuraTTTStwin‐to‐twin transfusion syndromeVKDBvitamin K‐dependent bleedingVWDvon Willebrand diseaseVWFvon Willebrand factorWBCwhite cell countWHOWorld Health OrganizationXLSAX‐linked sideroblastic anaemiaXLTX‐linked thrombocytopenia
1 The full blood count and blood film in healthy term and preterm neonates
Introduction
Haemopoiesis is the process that ensures life‐long production of haemopoietic cells. In newborn infants the process has many distinct features that differ from those in older children and adults. These differences reflect both the ontogeny of haemopoiesis during fetal development and the unique interaction between the fetus and mother, as well as the effects of birth itself. The sequential changes in the sites and regulation of haemopoiesis during development also help to explain the natural history of many neonatal haematological problems.
Brief outline of the ontogeny of haemopoiesis
Haemopoiesis in humans begins in the yolk sac between 2 and 3 weeks post‐conception ( Fig. 1.1). 1,2This is known as primitive haemopoiesis. Studies in other species, particularly in mice, indicate that the predominant cell types produced in the yolk sac are erythroid cells and macrophages. 2,3While megakaryocytes and lymphoid cells may also be yolk sac‐derived, the current consensus of opinion is that true, long‐lived haemopoietic stem cells (HSC) arise from a region of specialised endothelium (‘haemogenic’ endothelium), which is localised to the ventral wall of the dorsal aorta in a region known as the aorto‐gonado‐mesonephros (AGM). 4–6In humans, haemopoiesis begins in the AGM at around 5 weeks post‐conception and is known as definitive haemopoiesis. 6–8Haemopoiesis in the aortic wall is only transient, presumably because this region lacks the necessary physical space and specialised microenvironment to support expansion and differentiation of the HSC and progenitor populations required to meet the needs of the growing fetus.
By 6 weeks post‐conception, HSC and progenitor cells have migrated to the fetal liver, 8,9which remains the main site of blood cell production throughout fetal life 10,11and AGM haemopoiesis ceases. The first signs of haemopoiesis in the bone marrow are evident from around 11 weeks post‐conception. 8,12Although fetal bone marrow is able to give rise to cells of all lineages, it is becoming clear that the predominant cell types produced in the bone marrow are B lymphocytes and their progenitor cells together with granulocytes, monocytes and their progenitors. Although erythropoiesis and megakaryopoiesis take place in the fetal bone marrow from the end of the first trimester, most red blood cell and megakaryocyte production takes place in the fetal liver until shortly before term. 8Thus, for preterm infants, the liver is the main haemopoietic organ at and shortly after birth; this is likely to be a contributory factor in a number of disorders, including the haematological abnormalities seen in neonates with Down syndrome (see pages 154–160 and 206).
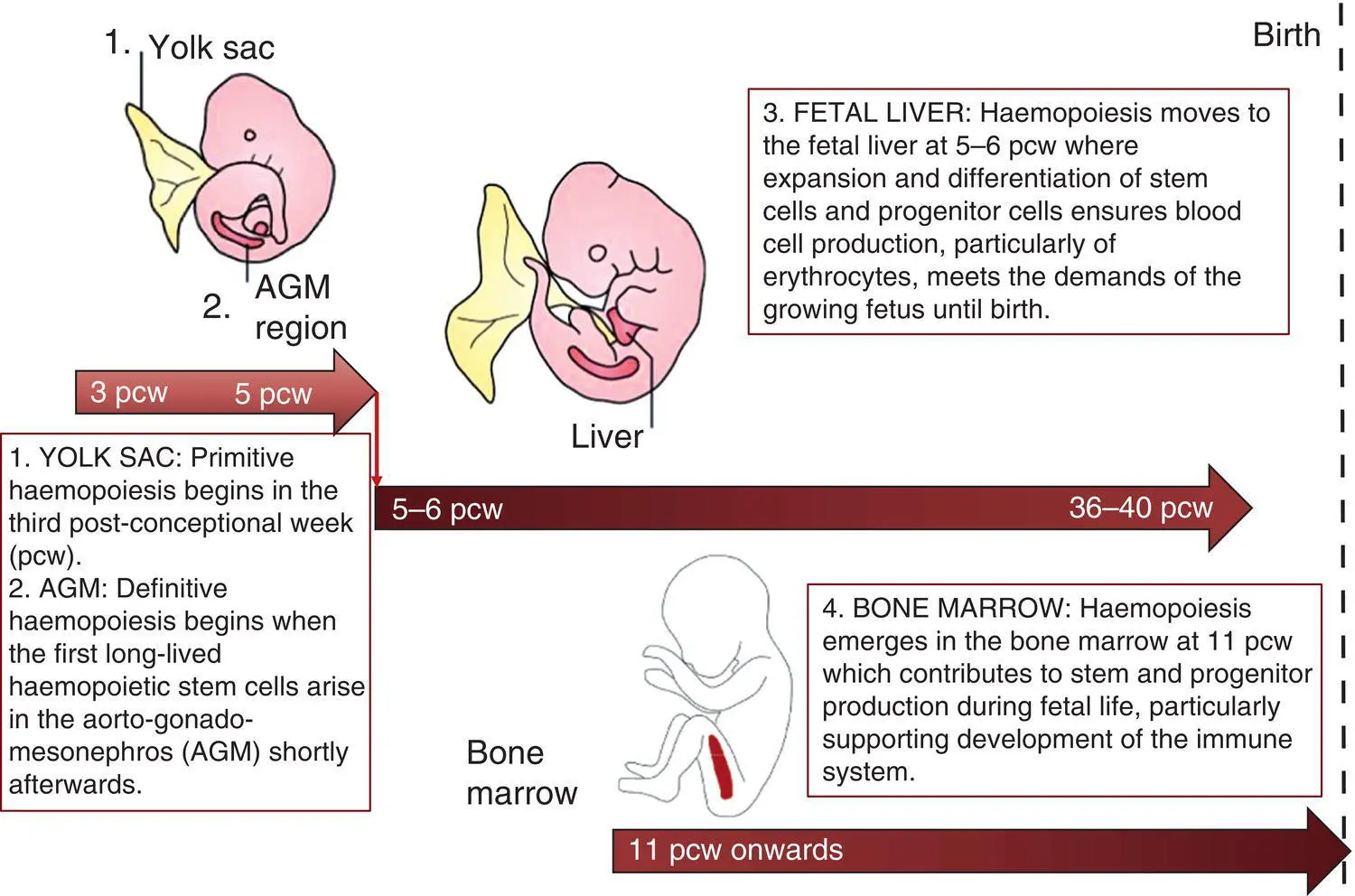
Fig. 1.1 Ontogeny of human haemopoiesis in embryonic and fetal life. AGM, aorto‐gonado‐mesonephros; pcw, post‐conceptional week. Based on references 1 and 2.
Properties of fetal haemopoietic stem and progenitor cells
Major advances in the immunological and molecular tools available to analyse haemopoietic stem and progenitor cells have allowed us to build up a much clearer picture of the process of haemopoiesis in fetal life and how this differs from adult life. Fetal HSC, like adult HSC, are the cells at the top of the haemopoietic hierarchy ( Fig. 1.2). When HSC divide, they do so either through a process of ‘self‐renewal’, where they generate more HSC (sometimes referred to ‘symmetric cell division’), or through asymmetric division during which one of the two daughter cells differentiates into progenitor cells, which in turn generate the mature cells of all the haemopoietic lineages ( Fig. 1.2). 9
Читать дальшеИнтервал:
Закладка:
Похожие книги на «Neonatal Haematology»
Представляем Вашему вниманию похожие книги на «Neonatal Haematology» списком для выбора. Мы отобрали схожую по названию и смыслу литературу в надежде предоставить читателям больше вариантов отыскать новые, интересные, ещё непрочитанные произведения.
Обсуждение, отзывы о книге «Neonatal Haematology» и просто собственные мнения читателей. Оставьте ваши комментарии, напишите, что Вы думаете о произведении, его смысле или главных героях. Укажите что конкретно понравилось, а что нет, и почему Вы так считаете.