The concentration of the transported substance on either side of the membrane plays a crucial part ( Figure 3.5b). Free and facilitated diffusion(if at all possible) happens spontaneously, from a compartment containing a high concentration of the compound in question toward another compartment containing only very few of these molecules. The net diffusion comes to an end when a concentration equilibrium is reached. For energetic reasons, this process cannot be reversed.
These rules also apply within the cell. Ion channels and passive transporters can only rebalance concentration levels. Where ions or metabolites are to be transported against a concentration gradient, additional energy is required. Specific ion pumpsin the biomembrane are in place to build up the ion gradient described in Table 3.1, which is needed for many intracellular processes (particularly secondary active transport, action potential, and signal transduction):
Na+, K+‐ATPase uses ATP to pump Na+ ions out of the cell and K+ ions into the cell. Necessary to build up the membrane potential.
Ca2+‐ATPase pumps Ca2+ into the ER.
Several strategies of transporting organic compounds against a concentration gradient are available to a cell ( Figure 3.5b–e):
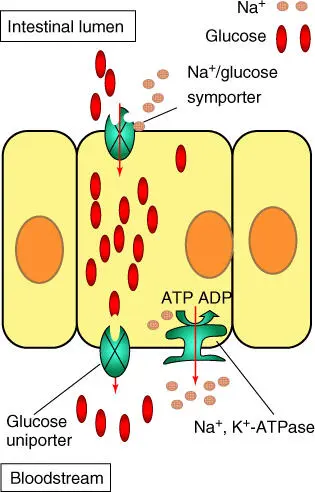
For active transport through ABC(ATP‐binding cassette)transporters. ATP can be used as energy source. ABC transporters are widespread among organisms (prokaryotes as well as eukaryotes) and are encoded by many genes. In humans, more than 50 ABC transporter genes are known. Particularly important are the MDR genes coding for multidrug resistanceproteins such as P‐glycoprotein(P‐gp). They are often very strongly expressed when a drug has been applied over longer periods. If, for example, such a drug has penetrated a tumor cell through diffusion, it is pumped out immediately into the extracellular space, thus losing its effectiveness ( Figure 3.5d). The best known is P‐gp (MW 170 kDa; two ATP‐binding sites and 12 transmembrane regions), encoded by the MDR1 gene. P‐gp is active in gut epithelia and in many other tissues. Furthermore, MRP1 and 2 (multiple resistance‐associated protein, 190 kDa, two ATP‐binding sites, and 17 transmembrane regions) are important, which are encoded by MRP1 and MRP2 genes ( Figure 3.5e). Overexpression of MDR proteins is also responsible for drug resistance in some malaria‐causing parasites.Apart from active transport with direct use of ATP, there are many other active transport mechanisms in a cell. These are referred to as secondary active transporters. They make use of an ion gradient that has been built up to transport a specific metabolite against the concentration slope, using ATP. Depending on whether the ions that share the pathway are concentrated on the same or the opposite side of the biomembrane, the transport is called symport or antiport. The transport mechanism resembles a revolving door, which can be operated from the inside as well as the outside. Within an individual cell, more than one transporter may be needed for one specific substance, depending on the concentration within the cell and in the extracellular space. This has been well researched by studying glucose transporters in intestinal cells ( Figure 3.6). There is a Na+ symporter on the luminal side, pumping glucose into the intestinal cell against a gradient. As the glucose concentration in the blood is lower, all that is needed is a simple uniporter to carry the glucose along the concentration gradient. The sodium ions that have been enriched inside the cell are pumped out of the cell using Na+, K+‐ATPase.
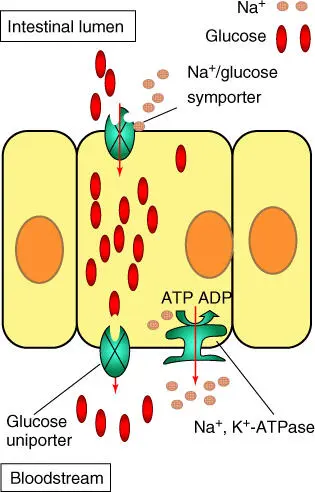
Figure 3.6 Glucose transporters in an intestinal cell. Glucose is pumped from the intestine into the cell by a Na +/glucose symporter and leaves it again using a uniporter, following the concentration gradient.
Research on genome projects of diverse organisms showed that genomes contain many transporter genes, although their specificity and function are still partly unknown. Finding answers to these questions is not only relevant to the understanding of cellular transport processes but also extremely important for pharmaceutical research. The pharmacokinetics( Chapter 25) of a compound is a crucial aspect. Although we often know that an active agent is taken up (i.e. it is bioavailable), we still do not know whether the uptake is the result of diffusion, the use of a transporter, endocytosis, or receptor‐mediated endocytosis.
3.1.1.3 Receptors and Signal Transduction at Biomembranes
Apart from ion channels and transporters, there are many other membrane proteins contained in the cytoplasmic membrane, such as receptors, enzymes, and anchor proteins. Some of these are schematically shown in Figure 3.5a.
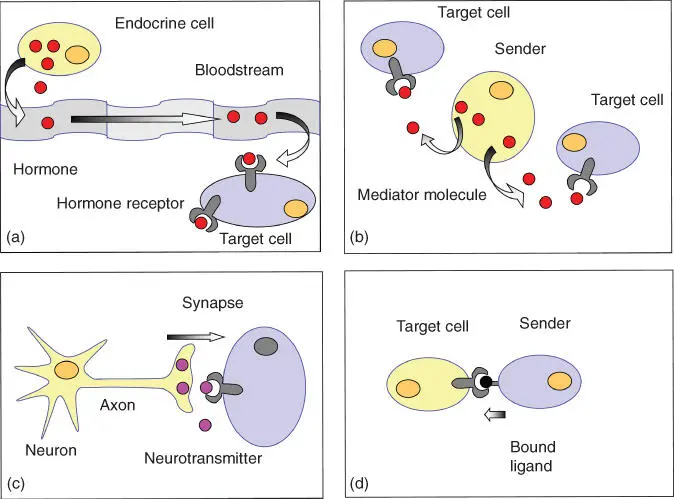
In a multicellular organism, the cells must be able to recognize and process signals from outside, coming from other cells or tissues. There are several cellular communication options ( Figure 3.7):
Endocrine signals (hormones) are produced by endocrinal gland cells (Table 3.2) and are released into the bloodstream. They circulate through the body and are picked up by receptors in the target cells – sometimes in a very distant part of the body – where they spring into action. In other words, hormones have a systemic effect. Hydrophilic and polar hormones (adrenaline and growth factors) bind to cell surface receptors, whereas lipophilic hormones (e.g. steroidal hormones, thyroxine, retinoic acid, vitamin D3) diffuse into the target cells to bind to intracellular receptors. These act as transcription regulators, controlling the expression of hormone‐regulated genes.Paracrine signals have an effect on their immediate surroundings. Released from a tissue cell, they are recognized and processed by neighboring cells. Their effect is local (e.g. prostaglandins).In direct cell‐to‐cell interaction, a cell presents a membrane‐bound signaling molecule to another cell carrying a membrane receptor that recognizes the molecule. Examples are found in the immune system (e.g. MHC complex and T‐cell receptors).In neuronal signal transduction, an electric signal (action potential) is transformed into a chemical signal at the synapse. Neurotransmitters are released that are recognized and processed by the receptors of a postsynaptic target cell.
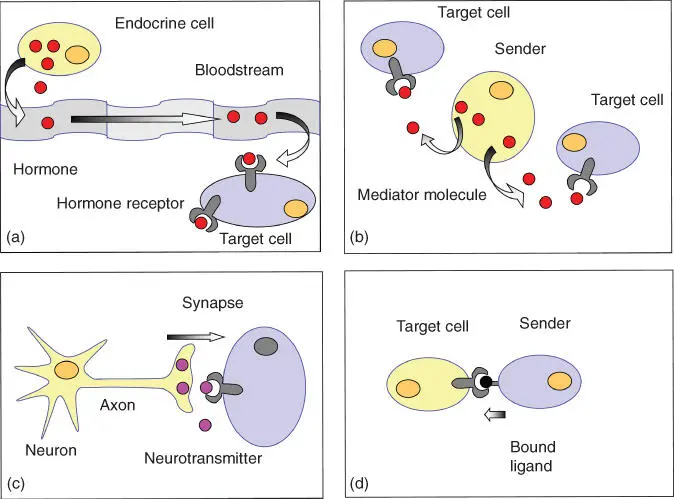
Figure 3.7 Schematic view of communication pathways between cells. (a) Endocrine signaling. (b) Paracrine signaling. (c) Synaptic signaling. (d) Contact‐dependent signaling.
Source: Alberts et al. (2015). Adapted with permission of Garland Science.
Table 3.2 Most important hormones in humans.
| Hormone |
Hormone gland |
Target |
Activity/function |
| Releasing hormones (P) |
Hypothalamus |
Adenohypophysis |
Regulate release of hormones from adenohypophysis |
| Inhibitory hormones (P) |
Hypothalamus |
Adenohypophysis |
Regulate release of hormones from adenohypophysis |
| Oxytocin (P) |
Hypothalamus |
Uterus, mammary gland |
Stored and released from neurohypophysis; stimulates uterus contractions, milk secretion, love, and empathy |
| Thyreotropin (GP) |
Adenohypophysis |
Thyroid |
Stimulates synthesis and secretion of thyroxin |
| Adrenocorticotropic hormone (ACTH) (P) |
Adenohypophysis |
Adrenal cortex |
Stimulates secretion of hormones of adrenal cortex |
| Luteinizing hormone (LH) (GP) |
Adenohypophysis |
Gonads |
Stimulates secretion of sex hormones from ovary and testes |
| Follicle‐stimulating hormone (FSH) (GP) |
Adenohypophysis |
Gonads |
Stimulates development of egg and sperm cells |
| Somatotropin (hGH) (P) |
Adenohypophysis |
Bones, liver, muscles |
Stimulates protein synthesis and growth |
| Prolactin (P) |
Adenohypophysis |
Mammary |
Stimulates milk production |
| Melanocyte stimulating hormone (MSH) (GP) |
Adenohypophysis |
Melanocytes |
Regulates pigmentation of skin |
| Endorphins, enkephalins (P) |
Adenohypophysis |
Neurons of spinal cord |
Analgesic properties |
| Adiuretin (ADH, vasopressin) (P) |
Neurohypophysis |
Kidneys |
Stimulates water reabsorption and increases blood pressure |
| Melatonin (AA) |
Epiphysis |
Hypothalamus |
Regulates biological rhythms (e.g. day/night rhythm) |
| Thyroxin (AA) |
Thyroid |
Many tissues |
General stimulant of metabolism |
| Calcitonin (P) |
Thyroid |
Bones |
Stimulates bone formation, lowers Ca 2+levels in blood |
| Parathormone (P) |
Parathyroid |
Bones |
Stimulates bone absorption, increases Ca 2+levels in blood |
| Thymosins (P) |
Thymus |
Leukocytes |
Activates T‐cell activity |
| Glucagon (P) |
Pancreas |
Liver |
Stimulates glycogen breakdown, increases blood sugar levels |
| Somatostatin (P) |
Pancreas |
Pancreas |
Inhibits release of glucagon, insulin, and digestive enzymes |
| Insulin (P) |
Pancreas |
Liver, muscles |
Stimulates uptake of glucose and glycogen formation |
| Gastrin (P) |
Stomach |
Stomach |
Stimulates release of digestive juices, enhances motility of stomach |
| Secretin (P) |
Duodenum |
Pancreas, stomach, gall bladder |
Regulates digestion processes, induces contraction of gall bladder |
| Adrenaline/noradrenaline (AA) |
Adrenal medulla |
Heart, liver, blood vessels |
Stimulates glycogen breakdown; stimulate heart, circulation, and blood pressure |
| Cortisol (glucocorticoid) (S) |
Adrenal cortex |
Muscles, many tissues |
Regulates stress reactions, stimulates metabolism of proteins and lipids, undergoes gluconeogenesis, inhibits inflammatory reactions |
| Aldosterone (mineral corticoid) (S) |
Adrenal cortex |
Kidneys |
Stimulates excretion of K +and ammonium ions and Na +reabsorption |
| Estrogen (S) |
Ovary |
Mammary, uterus |
Regulates development and function of female sexual characters and sexual behavior |
| Progesterone (gestagen) (S) |
Ovary (corpus luteum) |
Uterus |
Important for pregnancy and embryonic development |
| Testosterone (S) |
Testes |
Diverse tissues |
Regulates formation of sperm cells, development and function of male sexual characters and sexual behavior; can enhance aggressiveness |
| Atrial natriuretic peptide (ANP) (P) |
Heart |
Kidneys |
Stimulates Na +excretion |
| Vitamin D (S) |
Skin |
Bones, kidneys |
Enhances blood Ca 2+level |
P, peptide or protein; S steroid; GP, glycoprotein; AA, amino acid derivative.
Читать дальше

![Andrew Radford - Linguistics An Introduction [Second Edition]](/books/397851/andrew-radford-linguistics-an-introduction-second-thumb.webp)